Meningitis (1)
advertisement

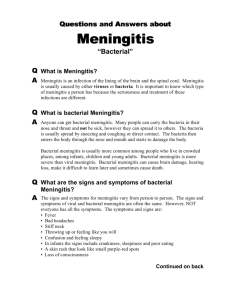
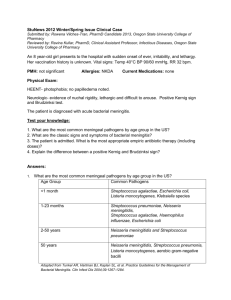
Infections of The Central Nervous System CNS Infections: • Encephalitis: Infection of brain parenchyma. • Meningitis: Infection of meninges. • Meningoencephalitis. • Myelitis: Infection of spinal cord tissue. • Subdural empyema. Brain abscess. • Acute disseminated encephalomyelitis: post viral infection encephalitis that is mediated by cross reactivity against myelin. • Bovine spongiform encephalopathy: Prions Natural defense mechanism of CNS: • The blood-brain barrier: endothelial cells that line brain capillaries (with tight junctions), astrocytic end-feet and thick basement membrane. • Local immune responses of CNS. Local Immune Responses of CNS: The CNS has an intrinsic immunological surveillance mechanism that depends on: • Presence of specific antigen presenting cell; the microglial cells. • Virchow-Robin spaces (the perivascular sheaths surrounding the blood vessels) contain lymph-like system of macrophages and lymphocytes. Blood-Brain barrier: prevent the passage of microbes and it’s toxic substances into the brain and CSF. However, the blood-brain barrier also: • Prevents the passage of humoral immune components (complement and antibodies) to the site of infection. • Prevents the cellular infiltration of WBCs to the site of infection. • Reduces the penetration of many antimicrobial drugs. Neurotropism and Microbial Virulence: Neurotropism: ability of some pathogenic microbes to infect the nervous system cells due to presence of specific virulence factors and specific receptors. Examples: Viruses: Poliovirus infects the motor neurons of the spinal cord and medulla. Mumps virus invades ependymal cells lining the ventricles in the fetal brain. (complication: 50% of patients develop meningitis, but only 5% are symptomatic). Bacteria: Capsules has anti-phagocytic capacity and resist complement mediated lysis. K1 capsular antigen (polysaccharide rich in sialic acid) increase the bacterial adherence ability to the meninges. In some strains of Escherichia coli and group B Streptococcus). Ports of entry to CNS: One of three routs: • Hematogenous rout: Respiratory epithelia, bite of animals (rabies virus) or transplacental (rubella virus). • Neural rout: rabies virus, HSV-1 &2 and Naegleria fowleri. • Direct inoculation (trauma, surgery or congenial defects). Classification of meningitis: • According to clinical presentation: acute, subacute and chronic. • According to etiology: bacterial, viral (aseptic meningitis), fungal, protozoal. • Acute meningitis is usually bacterial or viral in etiology. • In all cases of suspected bacterial meningitis, antibiotic therapy must be administrated immediately. Acute Meningitis (bacterial and viral) Etiology of acute bacterial meningitis: varies with the age of the patients: • Neonates and infants younger than 3 months of age; group B streptococci (50%), E. coli (20%), and Listeria monocytogenes and others (up to 10%). • In infants older than 3 months, children and adults: Streptococcus pneumonia, Neisseria meningitides (outbreaks), and Haemophilus influenzae type b (in non immunized). Pathogenesis: • Upper or lower respiratory infection or carrier state: Neisseria meningitides , Streptococcus pneumonia & Haemophilus influenzae type b. • Bacteremia; capsule resist humoral mediated destruction. • Reach CNS through choroid plexus, due to lack of tight junctions between endothelial cells (loss of blood-brain barrier); direct access to the CSF. • Blood to the choroid plexus to the ventricular CSF to ependymal cells lining the ventricles to periventricular brain tissues. Damage and Destruction: • CSF glucose, protein& oxygen content supports bacterial multiplication (in Pia, arachnoid & CSF). • Bacterial exotoxins and endotoxin (LPS) production cells death. • Infiltration and proliferation of microglial cells. Chemotaxis of neutrophils & lymphocytes from choroid plexus and Virchow-Robin space. Cytokines produced (edema & damage). • Increased Intracranial pressure (ICP). • Increased ICP (Intracranial pressure): due to hematomas (break BBB), cerebral edema and decreased CSF reabsorption and increased secretion. • Reduced cerebral perfusion pressure (blood flow pressure to the brain) due to: Increased Intracranial pressure. Reduced mean arterial pressure secondary to shock. This will results in: thrombosis and ischemia, and so neuronal infarction. So damage results from: bacterial toxins, cytokines effects and infarction due to increased ICP, reduced perfusion and thrombosis. Clinical presentation of N. meningitides infection: Meningitis, meningococcemia or meningitis with meningococcemia. Mortality rate in meningococcemia is ̴ 70 %. Symptoms: General symptoms: Headache, high fever & vomiting. Meningitis: photophobia, neck stiffness, seizures (20%), and skin rash (50%). Meningococcemia: purpuric skin rash (endothelia necrosis); hypotension, thrombosis causes disseminated intravascular coagulopathy (DIC); multiple organ failure and death. Subdural Empyema • Collection of pus between the dura mater and arachnoid mater (usually unilateral). • In infants, and young children; it occurs as a complication of meningitis. • In adults; it occurs as a complication of otitis media, mastoiditis or paranasal sinusitis (mainly frontal and ethmoid sinusitis; 2 weeks later). • Infection spreads intracranial through thrombophlebitis. Acute Viral Meningitis (Aseptic Meningitis): Aseptic meningitis: Negative CSF bacterial culture. Causes: • Enteroviruses. • Mumps virus. • Arboviruses. • Herpes viruses. • Lymphocytic Choriomeningitis virus • Other viral causes: Adenovirus, Measles, HIV: in 5-10 % of AIDS patients. Enteroviruses: Family: Picornaviridae. Enteroviruses: Echoviruses, Coxsackievirus A and B viruses, Poliovirus. • Currently more than 85% of viral meningitis are due to non-polio Enteroviruses. Coxsackievirus B accounts alone for more than 60% of meningitis in infants younger than 3 months. Enteroviruses 70 and 71 has a strong neurotropism that results in encephalitis with polio-like paralysis. Mumps virus: Paramyxoviridae. In parts of the world where vaccine is not applicable; it causes 10% of cases. Arboviruses: Arthropod-borne infection associated with 5% of cases. Herpes viruses:HSV-1 and HSV-2 (account 4% of the cases). Lymphocytic Choriomeningitis virus: Arenaviridae; meningitis with lymphocytic infiltration of choroid plexuses. Encountered from hamsters, rats or mice by inhalation route, ingestion route or contaminated wound. Mild or asymptomatic except for immunocompromised. Chronic Meningitis Causes: Bacteria: Mycobacterium tuberculosis. Fungi: Cryptococcus neoformans. CNS Tuberculosis: • Tuberculous Meningitis. • Spinal cord tuberculosis. Tuberculous Meningitis: • Pathogenesis: During primary pulmonary infection; tubercle bacilli may disseminate to the meninges or brain parenchyma through lymphatics. • These bacilli are contained within subpial or subependymal granulomas that remain latent unless the cellular immunity decreases. • When immunity decrease the size of foci increases; ruptures into the CSF & subarachnoid space causing basilar cisterns meningitis. • As the cellular immunity returns granulomas (tuberculoma, caseous abscess, cold abscess) are reformed. • Basilar meningitis may lead to: o Cranial nerves III, VI, VII dysfunction. o Obstructive hydrocephalus & increased ICP. Spinal cord tuberculosis: The earliest lesion are in the lumbar or thoracic vertebra (vertebral osteomyelitis). - Might be complicated by spinal epidural abscess; rupture of abscess may cause spinal meningitis. - Involvement of the dorsal columns of the spinal cord results in loss of position sensation. Resemble tabes dorsalis caused by Treponema pallidum (neurosyphilis). Fungal Meningitis: Cryptococcus neoformans: • Melanin producing yeast reproduce by budding. In tissues it has a large polysaccharide capsule. • Found in soil contaminated by birds excreta. • It causes infection in immunocompetent patients (20% of cases) and children. • Primary infection in the lung is usually asymptomatic. Due to resistance of phagocytosis and decreased cell-mediated immunity; carried by bloodstream to the brain (subacute or chronic meningitis). Amebic Meningitis or Meningoencephalitis: -Primary amebic meningitis: Naegleria fowleri; the freshwater brain-eating amoeba. -Secondary amebic meningitis: Entamoeba histolytica. Naegleria fowleri Meningitis: - Classified as ameboflagellate. Salt, chlorine & pH-sensitive microbe. Heat tolerant at 45.8ᵒC. - Exposure to river’s water (swimming) causes this rare and lethal infection within 1-2 weeks. - Mortality rate 97% Pathogenesis: -Port of entry: Neural route: through olfactory nerve endings. Migration through the cribriform plate of ethmoid bone to parenchymal cells of olfactory bulbs. -Reach subarachnoid space; meningitis, acute ependymitis; encephalitis. Diagnosis of Meningitis • Clinical history & examination. • Laboratory Diagnosis: CSF analysis o Turbidity and increased opining pressure. o Hematology analysis: Leukocytes count and differential count. o Biochemistry analysis: glucose &protein. o Microbiology Laboratory: • Direct Microscopy and culture. • Detection of microbial genetic material by PCR. • Rapid tests: serology In Hematology Laboratory: Leukocytes count and differential count: Normal Leukocytes count: 0-6 cells/mm3 (lymphocytes). - If it is > 1000/cumm : suspect bacterial infection. - If it is < 300/cumm : suspect viral infection. Differential count: - if % neutrophils is >50% : suspected bacterial infection. - if % of neutrophils < 50% and lymphocytes dominates: suspect viral infection. In Biochemistry Laboratory: Glucose: - Decreased level: suspected bacterial infection. - Normal Level: suspect viral infection. Protein: • Increased protein: bacterial infection. • Increased or normal protein level: Viral infection. In Microbiology Laboratory: Direct Microscopy: CSF specimen should be concentrated by centrifugation; and the pellet will be used for: Gram’s stain: gram positive or negative cocci or bacilli. Z.N stain: for acid-fast bacilli; M. tuberculosis Capsule stain: for Streptococcus pneumoniae. India ink wet-mount: for all capsulated microbes specially Cryptococcus yeasts. The Budding capsulated yeast Cryptococcus neoformans as shown in India ink wet mount . The Gram’s negative diplococci (N. meningitidis) inside polymorphnucleated neutrophils. (Gram’s stain). Gram positive lancet shape capsulated diplococci (S. pneumoniae) Mycobacterium (Z.N Stain); lymphocytic infiltration. Microbial cultivation and identification: Isolation of Streptococcus pneumoniae: (most common cause in adults): - Gram positive lancet-shaped capsulated cocci. - Alpha hemolytic on blood agar. - Optochin sensitive. O P Isolation of Neisseria meningitidis: (most common between the ages of 2-18 years, outbreaks). -Gram negative diplococci inside polymorph nucleated phagocytes (in CSF). -Fastidious bacterium grow best on chocolate agar and at microaerophilic conditions of 5-10 % CO2. -Oxidase positive. - Glucose and maltose fermenters. Isolation of Haemophilus influenzae: (infants and young children): - Pleomorphic Gram’s negative coccobacilli. - Fastidious (similar to N. meningitidis). Only grow on chocolate agar because it needs hemin and NAD. - Type b capsule can be examined by Quellung swelling test or immunofluorescent staining. Quellung reaction Satellitism of H. influenzae around S. aureus growth Isolation of Group B Streptococci : (Streptococcus agalactiae): - The leading cause of neonatal meningitis and septicemia with high mortality rate. - Found normally in the vagina and cervix of female carriers. Transmitted during birth. - Gram positive cocci in chains. - Beta hemolytic activity. - Bacitracin resistant. Isolation of E. coli: - Neonatal meningitis. - Gram negative bacilli. K1 Capsular antigen. - Lactose fermenters. Indole positive. - Metallic green sheen on EMB medium. Detection of microbial genetic material by PCR: PCR has a significant diagnostic value for: Detection of Mycobacterium genes in CSF. Detection of viral genetic material in CSF (RT-PCR). Serology: direct agglutination: A-Microbial capsule. B-Microbial exotoxins. Streptococcus B N. meningitidis Positive H. influenzae b E.coli S. pneumoniae Control Case Study: A 32-year-old lady immigrated from India to the United States 2 years ago. Four weeks following her arrival, her oldest child returned from child care with chicken pox. Two weeks later, she developed the disease. Over the next week she developed headache, fever and vomiting and after a week became stupor. Physical examination: impaired eye movements. Chest radiography showed lobar pneumonia. computerized tomography (CT) scan showed enlarged ventricles suggestive of acute hydrocephalus Lumbar puncture revealed high elevated opening pressure, and the CSF showed 350 WBCs/mm3, of Which 87% were lymphocytes. The CSF protein was 168 mg/dl (increased), and the glucose was 20 mg/dl(decreased). Gram’s stain and acid-fast stain of CSF showed negative results. A positive PCR results confirmed mycobacterial meningitis. She was treated with isoniazid, rifampin, pyrazinamide, and streptomycin with steroids for 2 months. With resolution of symptoms, she was discharged to receive 10 additional months of therapy with isoniazid and rifampin. 1-How does chicken pox activate this infection? 2-What is the explanation for eye movement abnormalities? 3-How do the CSF finding in this case compare with other viral or bacterial meningitis? 4-Why are multiple drugs required for the treatment of this case?