Reproductive
System
Diseases and
Disorders
Lindsea Vaudt
Shelby Engel
Female Anatomy and Physiology
Male Anatomy and Physiology
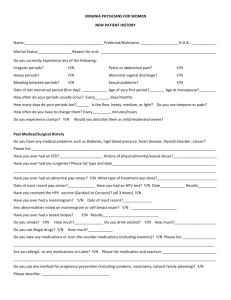
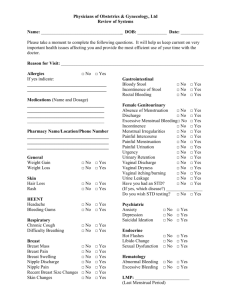
Common Signs and Symptoms
Female
Male
Abdominal and pelvic pain
Fever and malaise
Abnormal vaginal drainage
Burning, itching, or both of the genitals
Pain during sexual intercourse
Any change in breast tissue
Abnormal discharge from the nipple
Urinary disorders, including frequency, dysuria, nocturia, and
incontinence
Pain in the pelvis, groin, or reproductive organs
Lesions on the external genitalia
Swelling or abnormal enlargement of the reproductive organs
Abnormal penile discharge
Burning, itching, or both of the genitals
Diagnosis – Physical examinations, bimanual examinations,
pap smears, biopsy, laparoscopy, x-rays, blood testing,
mammograms, digital rectal examinations, cystoscopy,
and lab testing
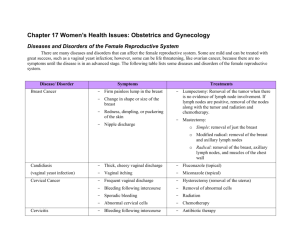
Female Reproductive System Diseases
Menstrual
abnormalities
Premenstrual syndrome
Amenorrhea
Dysmenorrhea
Menorrhagia
Metrorrhagia
Menopause
Vaginitis
Vaginitis
Inflammation of the vagina and vulva
Symptoms:
Redness and swelling of the vagina and vulva
Unusual vaginal discharge
Vaginal and genital burning
Vaginal and genital itching
Can increase risk for
HIV, AIDS, and other STDs
Infertility
Pelvic inflammatory disease
Premature birth low birth weight, stillbirth, and
complications
Causes
Infectious
Bacterial vaginosis
Chlamydia
Genital herpes
Gonorrhea
Poor genital hygiene
Trichomoniasis, a STD caused by a parasite
Yeast Infection
Noninfectious
Irritating substances to genitals
Leaving tampons in too long
Sexual abuse in girls
Antibiotics
Wearing thongs or tight fitting underwear, pants
Prevention
Abstaining
from sexual activity
Avoiding exposure of the genitals to
irritating substances
Changing tampons frequently
One sexual relationship in which neither
partner has an infection
Getting regular, routine medical care,
including pelvic exams
Not wearing tight fitting bottoms
Wiping from front to back after bowel
movements
Using a new condom for sexual acts
Treatment
Antibiotic
medications
Antifungal creams or pills for yeast
infection
Antiviral medications for genital herpes
Topical crams may be prescribed to ease
the discomfort of itching and burning
Amenorrhea
Absent menstrual periods for more than 3 monthly
menstrual cycles
Primary: menstruation never starts
Secondary: menstrual periods become abnormal,
irregular or absent
Causes
Natural reasons: Pregnancy, breast feeding,
menopause
Ovulation abnormality
Birth defect, anatomical abnormality, or other
medical conditions
Eating disorder
Over exercise or strenuous exercise
Thyroid disorder
Obesity
Amenorrhea cont.
Signs and symptoms:
Headache
Milky nipple discharge
Hair loss
Excess facial hair
Vision changes
Weight gain or loss
Can cause infertility or osteoporosis (with low
estrogen levels)
Prevention – Maintaining a normal weight
Treatment
Progesterone supplements (hormone treatment)
Oral contraceptives (ovulation inhibitors)
Dietary modifications (to increase caloric and fat
intake)
Calcium supplementation to reduce bone loss
Dysmenorrhea
Menstrual condition: severe and frequent
cramps and pain during menstruation
Primary: from beginning and usually lifelong
Secondary: due to physical cause or another
medical condition
Causes
Primary:
Chemical imbalance in the body: particularly
prostaglandin and arachidonic acid
Secondary:
Other medical conditions: endometriosis (tissues
becomes implanted outside the uterus),
Resulting in internal bleeding, infection, and pelvic
pain.
Treatment
Aspirin and ibuprofen
Oral contraceptives (ovulation inhibitors)
Progesterone (hormone treatment)
Dietary modifications
Vitamin supplements
Regular exercise
Heating pad across the abdomen
Hot bath or shower
Abdominal massage
Endometrial ablation: a procedure to destroy
the lining of the uterus
Endometrial resection: a procedure to
remove the lining of the uterus
Hysterectomy
Dysmenorrhea cont.
Symptoms:
Cramping in the lower abdomen
Pain in the lower abdomen
Low back pain
Pain radiating down the legs
Nausea
Vomiting
Diarrhea
Fatigue
Weakness
Fainting
Headaches
Prevention and risks:
Don’t smoke
Don’t drink alcohol during menses
Stay a healthy weight
Greater risk are those who started menstruating before
11 years old
Diseases of the Breast
Quite uncommon
Screening
1 in 8 women in the United States ranging from
mild to life-threatening
Men can also be affected
Self-examinations and mammography
Any change from normal in tissue shape or
appearance in males or females should be
called to the attention of a physician
Disease and Disorders
Fibrocystic Disease
Mastitis
Breast Cancer
Fibrocystic Disease
Most common breast disorder of premenopausal
women between ages 30-55
Thought to be linked to estrogen levels
Causes an increased risk of cancer
Symptoms:
Irregular, lumpy feeling in the breast (usually in the
upper outer quadrant area)
Breast discomfort that is persistent or occurs on and
off (peaking around the menstrual period and
receding after)
Breast often feeling heavy, full, and tender
A tendency to run in families
Fibrocystic Disease cont.
Diagnosis – Made by feeling, or palpation, or lumpy
areas in the breast
Multiple cysts make it difficult to detect
Breast ultrasounds
If there is a suspicious area a surgical biopsy can be
performed
Treatment – Measures to decrease breast pain include:
Elimination of caffeine in the diet
Reduction of salt intake
The use of a mild diuretic the week prior to menstruation
Use of mild analgesics
Prevention – Often not preventable, but decreasing
dietary fat and caffeine intake can help
Research showed that 90% of women who stopped wearing
a bra showed improvement in symptoms
Mastitis
Inflammation on the breast tissue
Broad term covering a variety of diseases and disorders
Type commonly thought of is puerperal (childbirth)
Symptoms:
Occurs when bacteria from the nursing baby’s mouth or
mother’s hands enter the breast tissue through the nipple
Redness
Heat
Swelling
Pain
Bloody discharges from the nipple
Diagnosis – Made on the basis of symptoms
Treatment – Antibiotics, application or heat, analgesics,
and a firm support brassiere to decrease discomfort
Prevention – Emptying breast completely when breast
feeding
Breast Cancer
Adenocarcinoma of the breast ducts
Most common neoplasm affecting breast tissue and
occurs in 1 out of 8 females
Early detection = monthly self-examinations and
routine mammograms
Cause is unknown, but risk factors include:
Age 40 and over
Family member affected with breast cancer
Onset of menses before age 13
Menses continuing after age 50
Nullipara (none or no births)
First child after age 30
Obesity
Chronic breast disease
Brassiere wear time
Breast Cancer cont.
Symptoms: Nontender lump of varying size…often no visual
symptoms
Diagnosis – Presence of lump, mammogram, and biopsy
(definitive test that can be performed by aspiration or surgery)
Treatment – Usually surgical removal of the mass or the breast
followed by chemotherapy, radiation therapy, or both
Lumpectomy – removal of the lump only
Simple or total mastectomy – removal of the breast and nipple
Modified radical mastectomy – removal of the breast, nipple, and
lymph nodes
Radical mastectomy – removal of the breast, nipple, lymph nodes,
and underlying chest muscles
Disorders of Pregnancy
Ectopic
Pregnancy
Spontaneous abortion (miscarriage)
Morning sickness
Hyperemesis Gravidarum
Toxemia
Abruptio placentae
Placenta previa
Ectopic Pregnancy
Ectopic
pregnancies occur in 1 in every
40 to 1 in every 100 pregnancies.
Hormones may play a role
Most common site is with in one of the
tubes where the egg passes from the
ovary to the uterus.
Causes
Birth defect in the fallopian tubes
Complications of a ruptured appendix
Having an ectopic pregnancy before
Scarring from past infections or surgery
Age over 35
Had surgery to untie tubes (tubal sterilization)
to become pregnant
Having had many sexual partners
In vitro fertilization
Having your tubes tied (tubal ligation) - more
likely 2 or more years after the procedure
Symptoms
Abnormal vaginal bleeding
Low back pain
Mild cramping on one side of the pelvis
Pain in the lower belly or pelvic area
If ruptures and bleeds symptoms may get
worse:
Fainting or feel faint
Intense pressure in the rectum
Low blood pressure
Pain in the shoulder area
Severe, sharp, and sudden pain in the lower
abdomen
Prevention
Avoiding risk factors for pelvic inflammatory
disease (PID) such as having many sexual
partners, having sex without a condom, and
getting sexually transmitted diseases (STDs)
Early diagnosis and treatment of STDs
Early diagnosis and treatment of salpingitis and
PID
Stopping smoking
Treatment
Ectopic pregnancies is a life-threatening
condition
If ruptures--- shock--- Blood transfusion
Surgery is done to stop blood loss, repair tissue
damage
Hyperemesis Gravidarum
Severe
Nausea
Vomiting
Weight loss
Electrolyte disturbance
Signs and symptoms:
Severe nausea and vomiting
Food aversions
Weight loss of 5% or more of pre-pregnancy weight
Decrease in urination
Dehydration
Headaches
Confusion
Fainting
Jaundice
Extreme fatigue
Low blood pressure
Rapid heart rate
Loss of skin elasticity
Secondary anxiety/depression
Treatment
Dietary
changes
Rest
Antacids
More
severe
Stay in the hospital
Mother
IV
receives fluid and nutrition through a
No known prevention
Abruptio Placentae
Separation
of the placenta from its
attachment to the uterus wall before the
baby is delivered
Direct causes are rare but include
Injury to the belly area
Sudden loss of uterine volume
Risk Factors
Blood clotting disorders
Smoking
Cocaine use
Diabetes
Alcohol
High blood pressure during pregnancy
About half of placental abruptions that lead to
the baby's death are linked to high blood pressure
Large number of past deliveries
Older mother
Premature rupture of membranes
The bag of water breaks before 37 weeks into the
pregnancy
Symptoms:
Prevention:
Abdominal pain
Back pain
Frequent uterine contractions
Uterine contractions with no relaxation in between
Vaginal bleeding
Don’t drink alcohol
Don’t smoke
Don’t use recreation drugs
Early and regular prenatal care
Manage conditions like diabetes and high blood
pressure
Treatment:
Fluids through IV
Blood transfusions
Unborn baby watched for signs of distress
C section may be needed
Male Reproductive System Diseases
Most common diseases affecting the male
reproductive system include infection and
diseases affecting the prostate
Diseases
Prostatitis
Benign Prostatic Hyperplasia
Prostatic Carcinoma
Epididymitis
Orchitis
Testicular tumors
Cryptorchidism (undescended testicle)
Prostatitis
Inflammation of the prostate gland
More common in men over 50 years old
Cause can be unknown or result of a urinary tract
infection or infection by STDs
Symptoms:
Dysuria (painful urination)
Pyuria (pus in urine)
Fever
Lower back pain
Diagnosis – Made on the basis of urinalysis, urine
culture, and digital rectal examinations
Treatment – Depends on the cause, but antibiotic
therapy with penicillin, warm sitz baths, increased
fluid intake, and analgesics
Prevention – Avoid smoking, drinking plenty of fluids,
seek early treatment for urinary symptoms, and
practice good hygiene by keeping the penis clean
Benign Prostatic Hyperplasia
Enlargement of the prostate due to normal cells
overgrowing and enlarging
Common in men over 60
About 50% of males over 65 have some degree of
prostate enlargement
Cause is unknown, but is thought to be due to hormonal
changes
Alterations in testosterone, estrogen, and androgen
levels (associated with aging)
Symptoms:
Nocturia (frequently getting up in the night to urinate)
Inability to start urination
Weak urinary stream
Inability to empty bladder (can cause frequent urinary tract
infections)
Diagnosis – Made on the basis of symptoms and digital
rectal examinations
BPH cont.
Treatment – Symptomatic and might include prostatic
massage, sitz baths, and catheterizations
Regular sexual intercourse can be helpful in reducing
prostatic congestion
Transurethral – Chisel away the excess prostate tissue
causing urinary obstruction
Prevention – No known preventative measures
Annual prostate exam after age 40
Prostatic Carcinoma
Neoplasm of the prostate usually affects men over
50
Cause is unknown…some believe testosterone
levels are involved
Caucasian men are affected with prostate
cancer 10 times more often than Oriental men
Grows in the outer layer or the prostate and often
shows no symptoms until it has metastasized
Environmental and lifestyle factors involved and diets
high in fat
Common sites = bones of the spine and pelvis
Symptoms: Similar to BPH as the urethra becomes
obstructed
Prostatic Carcinoma
Diagnosis – Digital rectal examination will reveal a hard,
abnormal mass and blood testing…biopsy is the definitive
test
Treatment – Depends on the age and physical condition of
the individual and the degree of metastasis
Administration of estrogen to counteract testosterone
Surgical orchiectomy – removal of the testicles to halt
testosterone production (many urologists do not believe this
improves the survival rate)
A combination of both treatments
Chemotherapy and radiation therapy might also be beneficial
Over 60 – most likely outlive the cancer and die of some
other disease process
Younger individuals and those with extensive metastasis do
not have such a positive prognosis
50%-75% live 5 years or more
Prevention – No preventative measures…annual prostate
examination is recommended for early detection
Epididymitis
Inflammation of the epididymis
Common causes include prostatitis, urinary tract infection,
mumps, and STDs (chlamydia, syphilis, and gonorrhea)
Most common disease of the male reproductive system
and usually only effects one epididymis
Symptoms:
Swollen, hard, and painful epididymis
Scrotal pain and swelling
Diagnosis – Made on the basis of symptoms, urinalysis, and
urine culture
Treatment – Prompt, appropriate antibiotic therapy, bed
rest, analgesics, use of a scrotum support, and avoidance
of alcohol, spicy foods, and sexual stimulation
Makes walking difficult
Delay in treatments can cause sterility (inability to impregnate a
female)
Prevention – Sexual absitenence, use on condoms to
prevent STDs and prompt treatment of causative infections
Orchitis
Inflammation of one or both testes
Usually due to bacterial or viral infection or trauma
Viral mumps is the most common cause in adult males
Commonly occurs in conjunction with or as a complication
of epididymitis
Symptoms:
Swelling, pain, and tenderness in one or both testes
Fever
Malaise
Diagnosis – Made on the basis of symptoms, blood testing,
and urinalysis
Treatment – Depends on the cause, but antibiotic therapy
is usually effective…when caused by mumps it is treated
symptomatically and includes bed rest and analgesics and
antipyretic medications
Prevention – Aimed at causative factors and includes
mumps vaccinations and prevention of infection from STDs
Sexually Transmitted Diseases
Acquired
immunodeficiency syndrome
Hepatitis
Genital
herpes
Gonorrhea
Syphilis
Tertiary (late or latent)
Chlamydial infection
Trichomoniasis
Genital warts
Gonorrhea
Bacterium
Grows in warm, moist areas of the
reproductive tract
Annually about 820,000 people in the US
Cervix, uterus, fallopian tubes, urethral
Mouth, throat, eyes, anus
570,000 among 15-24 years of age
Causes:
Having sex with someone who has the disease
Anal, vaginal, or oral sex
Can spread from mother to baby during
childbirth
Gonorrhea cont.
Very mild or no symptoms
Men: burning sensation when urinating
Women:
White, yellow, or green discharge
Painful or swollen testicles
Painful or burning sensation when urinating
Increased vaginal discharge
Vaginal bleeding between periods
Treatment – ASAP especially if
pregnant…medication
Prevention:
Condom use
Avoid having sexual intercourse
One partner who is not infected
Syphilis
Serious STD
Can become chronic, life threatening disease
Bacterium
Annually 55,400 people in the US
In 2011, 72% occurred among men who have sex
with men
360 reports of children in 2011
Causes
Person to person by direct contact with syphilis sores
Genitals
Vaginal
Anus
Rectum
Lips
Mouth
During vaginal, anal, or oral sexual contact
Pregnant women can pass it to unborn child
Symptoms
First symptom can appear in 10 to 90 days
PRIMARY stage:
Single sore--- multiple sores
Where syphilis entered the body
Firm, round, painless
Will go away without treatment
Infection can progress to the secondary stage
if no treatment
SECONDARY stage:
Skin rashes or sores in the mouth, vagina, anus
Not itchy
Rough, red, or reddish brown spots on palms or bottom
of feet
Large, raised, gray or white lesions on mouth, underarm,
groin
Fever, swollen lymph glands, sore throat, patchy hair
loss, headaches, weight loss, muscle aches, fatigue
Latent and Late Stage
Symptoms will go away without treatment BUT…
without appropriate treatment, the infection will
progress to the latent or late stages
Can last for years
15% of people not treated
bad muscle movements, paralysis, numbness,
gradual blindness, and dementia
Damages internal organs, including brain, nerves,
eyes, heart, blood vessels, liver, bones, and joints
Death
Treatment – Easy to treat in early stages, no over
the counter drugs, antibiotics
Prevention – Not by washing genitals after sex,
condom use, abstain from sex when infected, and
one partner without infection
Chlamydial Infection
Most commonly reported STD in the US
Sexually active females 25 years and younger
need testing every year
Bacterium
Can cause serious damage to a woman’s
reproductive organs
In 2011, 1,412,781 cases where reported in the
US
1 in 15 sexually active females age 14-19 years
have Chlamydia
Causes:
Having sex with someone infected
Anal, vaginal, oral
Pregnant woman to her baby during childbirth
Symptoms
“Silent Infection”
Can damage a woman’s reproductive organs
Women:
Infects the cervix and urethra
Abnormal vaginal discharge
Burning sensation when urinating
Untreated---- spread up to uterus and fallopian
tubes
Pelvic inflammatory disease
Lead to infertility
Men:
Discharge from penis
Burning sensation when urinating
Pain and swelling in one or
both testicles
Treatment
Antibiotics
Prevention:
Condom
use
Abstain form vaginal, anal, and oral sex
One partner who is not infected
Sexual Dysfunction
Can limit the ability of the individual to reproduce
and to develop a close, nurturing sexual
relationship with a significant other
Human sexual cycle – Arousal…sexual
intercourse…climax…feelings of pleasure and
relaxation
Any disorder that interrupts this cycle can be
considered a dysfunction
Disorders
Dyspareunia
Female Arousal-Orgasmic Dysfunction
Impotence (erectile dysfunction)
Premature Ejaculation (rapid ejaculation or rapid
climax)
Infertility
Dyspareunia
Condition of experiencing pain or discomfort with
sexual intercourse
Can affect both males and females, but more
common in women
Not considered a disease but, rather, a symptom of
a psychological or physical disorder
Female - Intact hymen, vaginal deformity, insufficient
lubrication, sensitivity to spermicide, presence of an STD,
bladder infection, pelvic inflammatory disease, and
endometriosis
Male – Penile deformity, presence of an STD, abnormally
tight foreskin (phimosis), prostatitis, and epididymitis
Psychological conditions – history of past sexual abuse,
anxiety, guilt, and fear of pregnancy
Symptoms: Pain can be mild to severe and appear in
genitals, pelvis, and low back…females might feel
pain specifically in the clitoris, labia, and vagina
Dyspareunia cont.
Diagnosis – General examination, description of
pain, and time of occurrence
Treatment – Restrictions of extended foreplay, use
of lubricating jelly, and manual stretching of the
vaginal opening prior to intercourse
Infections need to be treated appropriately and
surgery may be needed to correct deformities,
remove tumors, and treat endometriosis
Counseling
Prevention – Not preventable when caused by
sexual trauma or abuse…avoid vaginal yeast
infections, STDs, bladder infections, and sex on
days near menstruation due to increased
tenderness
Female Arousal-Orgasmic Dysfunction
Lack of sexual desire or responsiveness in a female
Commonly due to psychological conditions such
as stress, depression, fatigue, past sexual abuse,
guilt, and anxiety
Symptoms: Inability to produce and maintain
adequate vaginal lubrication and vasocongestive
response
Diagnosis – History or complaint of the inability to
reach orgasm
Treatment – Physical exam to rule out physical
disorders and possible sex therapy
Prevention – Education on healthy sex attitudes
and sexual stimulation techniques
Infertility
Inability of a couple to achieve pregnancy after 1 year of
unprotected sexual intercourse
Can be due to male or female disorders or both
About 1 in 10 couples experience infertility
Common causes:
Female
Male
Presence of STD
Hormonal disorders
Abnormality of reproductive organs
Endometriosis
Scarring from PID or blockage or fallopian tubes
Development of vaginal antibodies that kill sperm
Presence of STD
Chronic genitourinary infection or blockage of the tract
Structural abnormalities
Hormone imbalances
Diagnosis – Female = complete medical and gynecologic
history and examination; Male = complete medical history
and physical examination with semen analysis
Infertility cont.
Treatment – Surgery to correct anatomical
abnormalities or remove blockages or medication
therapy to correct endocrine and hormone
imbalances and treat infection
Fertility drugs, artificial insemination with husband sperm
(AIH), artificial insemination with donor sperm (AID), and
in vitro fertilization (IVF)
Prevention:
Avoid smoking and drinking
Eat a healthy diet
Avoid excessive exercise
Avoid STDs
Maintain proper body weight to reduce possibility of
hormone imbalance
Check with doctor if taking and medications or herbal
remedies
Trauma and Rare Diseases
Rape – Sexual intercourse (vaginal or anal) without
consent or against the will of the involved individual
Vaginal Cancer - Rare form of cancer that occurs in
the daughters of mothers who used the synthetic
hormone diethylstilbestrol (DES) to prevent
spontaneous abortion
Puerperal Sepsis - Infection in the endometrium,
usually with streptococcus bacteria, following
childbirth
Victims – Any age and either sex, but is primarily and act
of violating females
Recovery from rape is difficult and crisis intervention
counselors are often needed
Other names = Puerperal fever and childbed fever
Hydatidiform Mole - Formation of grape-like cysts in
the uterus that fill the uterus and give indications of
pregnancy
Effects of Aging
Females
Internal organs shrink in size, vaginal secretions
diminish, and there is less elasticity of the vagina
Women over 65 should be screened regularly for
disorders such as cancer of the uterus and ovaries
Males
Production of testosterone and the formation of
sperm decreases
Size of the testes can also diminish, some loss of
elasticity of the penis and scrotum causing them to
look more wrinkled and sagging
Prostate slowly enlarges around age 50
Routine rectal examination for all adult males over
age 50
References
Neighbors, M. & Tannehill-Jones, R. (2010). Human
diseases (3rd ed.) Clifton Park, NY: Delmar
Cengage Learning.
http://www.bettermedicine.com/topic/endometri
osis/dysmenorrhea?p=2
http://www.mayoclinic.com
http://americanpregnancy.org/pregnancycompli
cations/hyperemesisgravidarum.html
http://www.cdc.gov