Eicosanoids
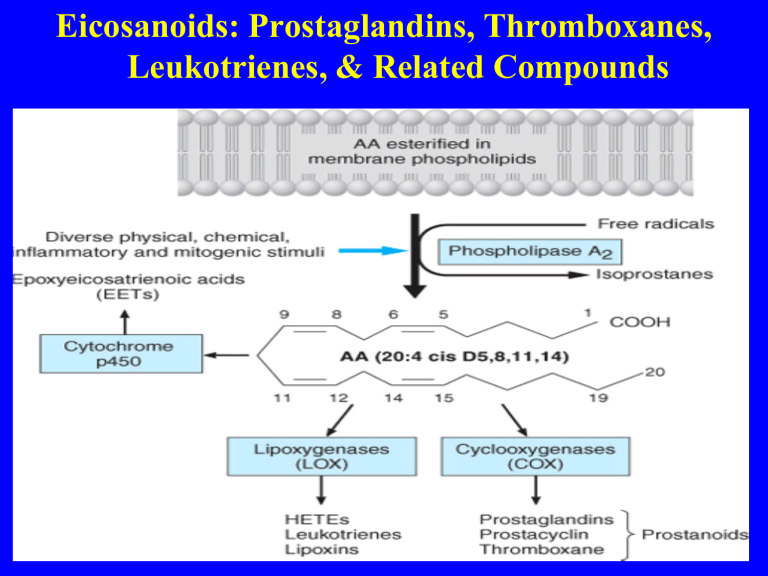
Eicosanoids: Prostaglandins, Thromboxanes,
Leukotrienes, & Related Compounds
Eicosanoids: Prostaglandins, Thromboxanes,
SYNTHESIS OF EICOSANOIDS
Products of Prostaglandin Endoperoxide
Synthases (Cyclooxygenases)
Two unique COX isozymes convert arachidonic acid into prostaglandin endoperoxide.
PGH synthase-1 (COX-1) is expressed constitutively in most cells.
Eicosanoids: Prostaglandins, Thromboxanes,
In contrast, PGH synthase-2 (COX-2) is inducible
its expression varies markedly depending on the stimulus.
COX-2 is an immediate early-response gene product that is
markedly up-regulated by shear stress, growth factors, tumor promoters, and cytokines
Eicosanoids: Prostaglandins, Thromboxanes,
Physiological role
COX-1 generates prostanoids
such as gastric epithelial cytoprotection
whereas COX-2 is the major source of prostanoids in inflammation and cancer.
For example, endothelial COX-2 is the primary source of vascular prostacyclin
whereas renal COX-2-derived prostanoids are important for normal renal development and maintenance of function. (maintain blood flow)
Eicosanoids: Prostaglandins, Thromboxanes,
Physiological role
COX-3
Mainly centrally FEVER AND PAIN and can be inhibited by
PARACETAMOL
prostaglandins and prostaglandin analogs currently in clinical use.
PHARMACOLOGY OF EICOSANOIDS
Effects of Prostaglandins & Thromboxanes
The prostaglandins and thromboxanes have major effects on four types of smooth muscle:
1- vascular
2- gastrointestinal
3- airway
4- eye ( smooth muscle)
5- reproductive
PHARMACOLOGY OF EICOSANOIDS
Effects of Prostaglandins & Thromboxanes
1- platelets and monocytes
2- kidneys
3- the central nervous system, autonomic presynaptic nerve terminals
4- sensory nerve endings
5- endocrine organs
PHARMACOLOGY OF EICOSANOIDS
A. SMOOTH MUSCLE
1. Vascular TXA2 is a potent vasoconstrictor
TXA2 is a smooth muscle cell mitogen
The mitogenic effect is potentiated by exposure of smooth muscle cells to testosterone
PHARMACOLOGY OF EICOSANOIDS
INTESTINE
Lubiprostone: Amitiza
®
USES
Lubiprostone is a PGE1 derivative used for the
Tretament of chronic idiopathic constipation and irritable bowel syndrome with constipation.
PHARMACOLOGY OF EICOSANOIDS
INTESTINE
Lubiprostone: Amitiza
®
Mechanism of action:
Lubiprostone stimulates chloride channels
(ClC-2) in the luminal cells of the intestinal epithelium, thereby
increasing intestinal fluid secretion.
The increased chloride concentration within the intestinal lumen softens the stool and increases intestinal motility.
PHARMACOLOGY OF EICOSANOIDS
INTESTINE
Lubiprostone: Amitiza
®
b. Side eff ects:
Nausea is the most common side eff ect of lubiprostone which can be decreased if taken with food.
diarrhea is the second most reported adverse
reaction, followed by headache and abdominal pain.
PHARMACOLOGY OF EICOSANOIDS
INTESTINE
Lubiprostone: Amitiza
®
Pharmacokinetics
Absorption: Minimal absorption, action is primarily in GI tract.
Distribution: Minimal systemic distribution.
Contraindicated :
Mechanical gastrointestinal obstruction
PHARMACOLOGY OF EICOSANOIDS
INTESTINE
Lubiprostone: Amitiza
®
Pharmacokinetics
Absorption: Minimal absorption, action is primarily in GI tract.
Distribution: Minimal systemic distribution.
Contraindicated :
Mechanical gastrointestinal obstruction
PHARMACOLOGY OF EICOSANOIDS
A. SMOOTH MUSCLE
2. PGF2a is also a vasoconstrictor but is not a mitogen for smooth muscle cells.
the isoprostane 8iso -PGF2a (iPF2aIII) which is also a vasoconstrictor may act via the TP receptor.
In patients with cirrhosis
8-iso-PGF2a is produced in large amounts in the liver
and is thought to play a pathophysiologic role as an important vasoconstrictor substance in the hepatorenal syndrome.
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
1- PGI2 and PGE2, promote vasodilation by increasing cAMP and decreasing smooth muscle intracellular calcium
2- Vascular prostacyclin is synthesized by both smooth muscle and endothelial cells,
3- In the microcirculation, PGE2 is a vasodilator produced by endothelial cells.
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS)
ILOPROST , a synthetic analog of prostacyclin
(PGI
2
), is a vasodilating agent and a plateletaggregation inhibitor.
Indications
Pulmonary arterial hypertension leading to
Improved exercise capacity
USE BY INHALATION
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS)
MECHANISM OG ACTION
Dilates pulmonary and arterial vasculature.
These actions are mediated through activation of the IP receptors (prostacyclin receptors)
Leading to an increase in the production of intracellular cyclic adenosine monophosphate
(cAMP).
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS)
TXA2 production is also inhibited
Contraindicated in:
Hypersensitivity
Systolic BP <85 mm Hg
Lactation: Lactation.
Use Cautiously in:
•
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS)
Contraindicated in:
Systolic BP <85 mm Hg
lactation
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS)
Use Cautiously in:
Concurrent use of drugs or coexisting medical conditions that may risk of syncope
COPD, asthma, or acute pulmonary infection (may risk of bronchospasm)
Hepatic impairment (may need to dosing interval)
OB: Use only if maternal benefit outweighs fetal risk.
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS) •.
Common Adverse Effects
Cough
headache
vasodilation (flushing)
Hypotension, syncope and palpitations
hemoptysis due to thrombaxe-A2 inhibition
PHARMACOLOGY OF EICOSANOIDS
Vasodilator prostaglandins
ILOPROST (VENTAVIS) •..
Interactions
risk of hypotension with other vasodilators or diuretics
Risk of bleeding may be by anticoagulant
PHARMACOLOGY OF EICOSANOIDS
2. . Airways Respiratory smooth muscle
The cysteinyl leukotrienes are bronchoconstrictors.
They act principally on smooth muscle in peripheral airways and are a thousand times more potent than histamine both in vitro and in vivo.
They also stimulate bronchial mucus secretion and cause mucosal edema.
Bronchospasm occurs in about 10% of people taking
NSAIDs, probably because of a shift in arachidonate metabolism from COX-1 metabolism
to leukotriene formation
PHARMACOLOGY OF EICOSANOIDS
PLATELETS
Both PGD2 and PGI2 inhibit aggregation.
TXA2 is the major product of platelet COX-1 , is a platelet aggregator
and amplifies the effects of other more potent platelet agonists such as thrombin.
The platelet actions of TXA2 are restrained in vivo by PGI2
which inhibits platelet aggregation by all recognized agonists.
PHARMACOLOGY OF EICOSANOIDS
PLATELETS
Platelets release TXA2 during activation and aggregation.
Urinary metabolites of TXA2 increase in patients experiencing a myocardial infarction
this Platelet COX-1-derived thromboxane synthesis is irreversibly inhibited by chronic dosing with aspirin in low doses.
Macrophage COX-2 appears to contribute roughly 10% of the increment in TX biosynthesis observed in smokers , while the rest is derived from platelets.
PHARMACOLOGY OF EICOSANOIDS
KIDNEY
Both the medulla and the cortex of the kidney synthesize prostaglandins
the medulla substantially more than the cortex.
The kidney also synthesizes several hydroxyeicosatetraenoic acids, leukotrienes, cytochrome
P450 products, and epoxides.
These compounds play important autoregulatory roles in renal function
PHARMACOLOGY OF EICOSANOIDS
KIDNEY by modifying renal hemodynamics and glomerular and tubular function.
This regulatory role is especially important in marginally functioning kidneys, as shown by the decline in kidney function caused by COX inhibitors
in elderly patients and those with renal disease.
The major eicosanoid products of the renal cortex are
PGE2
and
PGI2
PHARMACOLOGY OF EICOSANOIDS
KIDNEY
PGE2 and PGI2 increase glomerular filtration through their vasodilating effects.
These prostaglandins also increase water and sodium excretion.
PHARMACOLOGY OF EICOSANOIDS
KIDNEY
Loop diuretics, eg, furosemide, produce some of their effect by stimulating COX activity.
In the normal kidney, this increases the synthesis of the vasodilator prostaglandins.
Therefore, patient response to a loop diuretic is diminished if a COX inhibitor is administered concurrently
PHARMACOLOGY OF EICOSANOIDS
KIDNEY
The normal kidney synthesizes only small amounts of
TXA2.
However, in renal conditions involving inflammatory cell infiltration (such as glomerulonephritis and renal transplant rejection)
the inflammatory cells (monocytemacrophages) release substantial amounts of TXA2
PHARMACOLOGY OF EICOSANOIDS
REPRODUCTIVE ORGANS
1. Female reproductive organs
PGF2-alpha, together with oxytocin, is essential for the onset of parturition
- Uterine muscle is contracted by PGF2a, TXA2
PHARMACOLOGY OF EICOSANOIDS
CENTRAL AND PERIPHERAL NERVOUS SYSTEMS
1. Fever
PGE2 increases body temperature
Exogenous PGF2a and PGI2 induce fever
pyrogens release interleukin-1, which in turn promotes the synthesis and release of PGE2 . This synthesis is blocked by paracetamol and other antipyretic compounds
EYE
PHARMACOLOGY OF EICOSANOIDS
PGE and PGF derivatives lower intraocular pressure. (eye drops in glaucoma)
The mechanism of this action is unclear but probably involves increased outflow of aqueous humor from the anterior chamber via the uveoscleral pathway
PHARMACOLOGY OF EICOSANOIDS
Glaucoma
Latanoprost
bimatoprost, travaprost , and unoprostone
1- a stable long-acting PGF2a derivatives
2- first prostanoid used for glaucoma
4- administered as drops into the conjunctival sac once or twice daily.
5- Adverse effects include irreversible brown pigmentation of the iris and eyelashes, drying of the eyes, and conjunctivitis
PHARMACOLOGY OF EICOSANOIDS
AGENTS THAT ENHANCE MUCOSAL DEFENSE
Misoprostol
Misoprostol (15-deoxy-16-hydroxy-16-methyl-PGE1; CYTOTEC ) is a synthetic analog of prostaglandin E1.
The degree of inhibition of gastric acid secretion by misoprostol is directly related to dose; oral doses of 100 to 200 mg significantly inhibit basal acid secretion (up to 85% to 95% inhibition) or foodstimulated acid secretion (up to 75% to 85% inhibition).
The usual recommended dose for ulcer prophylaxis is 200 mg four times a day.
PHARMACOLOGY OF EICOSANOIDS
AGENTS THAT ENHANCE gastric MUCOSAL
DEFENSE
Mechanism of Action; Pharmacology.
Prostaglandin E2
(PGE2) and prostacyclin (PGI2) are the major prostaglandins synthesized by the gastric mucosa.
- PGE2 also can prevent gastric injury by cytoprotective effects that include stimulation of mucin and bicarbonate secretion and increased mucosal blood flow.
Since NSAIDs diminish prostaglandin formation by inhibiting cyclooxygenase, synthetic prostaglandin analogs offer a logical approach to reducing NSAID-induced mucosal damage
PHARMACOLOGY OF EICOSANOIDS
AGENTS THAT ENHANCE GASTRIC MUCOSAL DEFENSE
Analog of prostaglandin E1
Misoprostol
Misoprostol (15-deoxy-16-hydroxy-16-methyl-PGE1; CYTOTEC) is a synthetic analog of prostaglandin E1.
The degree of inhibition of gastric acid secretion by misoprostol is directly related to dose; oral doses of 100 to 200 mg significantly inhibit basal acid secretion (up to 85% to 95% inhibition) or foodstimulated acid secretion (up to 75% to 85% inhibition).
The usual recommended dose for ulcer prophylaxis is 200 mg four times a day.
CLINICAL OF EICOSANOIDS analogues
1-
Dinoprostone, a synthetic preparation of PGE2
is administered vaginally for oxytocic use.
it is approved for inducing abortion in the second trimester of pregnancy
for missed abortion,
and for ripening of the cervix for induction of labor in patients at or near term
CLINICAL OF EICOSANOIDS analogues
Dinoprostone also directly affects the collagenase of the cervix, resulting in softening
For abortifacient purposes, the recommended dosage is a 20-mg dinoprostone vaginal suppository repeated at 3- to 5-hour intervals depending on the response of the uterus.
For softening of the cervix at term, the preparations used are either a single vaginal insert containing 10 mg PGE2
or a vaginal gel containing 0.5 mg PGE2 administered every 6 hours. The softening of the cervix for induction of labor substantially shortens the time to onset of labor and the delivery time.
CLINICAL OF EICOSANOIDS analogues
PGF2alpha
1- This drug, carboprost tromethamine
(15-methyl-PGF2a; the 15-methyl group prolongs the duration of action)
2-used to induce second-trimester abortions and to control postpartum hemorrhage that is not responding to conventional methods of management.
3Vomiting and diarrhea occur commonly, probably because of gastrointestinal smooth muscle stimulation.
Transient elevations in temperature are seen in approximately one eighth of patients .
Modulators of the pathways
NSAID’s and
Corticosteroids (COX
Inhibitors)
Lipoxygenase Inhibitors (Zileuton )
TXA
2
Synthase Inhibitors
LTD
4
Receptor Antagonist ( Montelukast-
SINGULAIR )
Pharmacological/Physiological
Effects
2. Platelets
ARACHIDONIC ACID
COX -1 _
Platelet
TXA
2
ASPIRIN
_ COX -2
Endothelial
PGI
2
Vasoconstriction
Platelet Aggregation
Vasodilation
Anti-Platelet Aggregation
Therapeutic Uses of
Modulators
NSAID’s
Corticosteroids: anti-inflammatory
analgesic, antipyretic.
Montelukast (LTD4 BLOCKER) in asthma
Mean % of Days 19%
33% 32%
Placebo Montelukast Beclometh.
Montelukast in
Asthma
Mean % days patients experienced sustained asthma control
% of patients without asthma attacks
Beclomethasone
NS
Montelukast
Placebo
Time after randomization (days)
Time to first asthma attack
BIOGENIC PEPTIDES
ANGIOTENSIN
Synthesis & metabolism
Angiotensinogen (plasma substrate) to angiotensin I, by renin that is released during renal ischemia.
Angiotensin I to II by angiotensin converting enzyme (ACE, Kinase II) in the pulmonary endothelium.
Renin inhibited by propranolol
Angiotensin II metabolized by angiotensinases in plasma and tissues.
BIOGENIC PEPTIDES
ANGIOTENSIN
Effects
Causes profound vasoconstriction
Increases peripheral vascular resistance
Increases blood pressure
Directly stimulates heart
Facilitates epinephrine and aldosterone release
Increases Na reabsorption in kidney tubules
Releases ADH (vasopressin) to restore blood volume
Losartan and valsartan blocks angiotensin (AT
1
) receptors
Captopril & enalapril inhibit ACE (congest. heart fail.).
BIOGENIC PEPTIDES
BRADYKININ
Actions
Comes under the group “kinins”
This mediates nociception (pain)
Regulates BP (vasodilator)
Increases capillary permeability
Balances electrolytes and fluid,
Contracts gut slowly and stimulates prostaglandin synthesis
Produced by tissue damage, viral infection, allergic reaction & inflammation
Contracts various other smooth muscles
BIOGENIC PEPTIDE
BRADYKININ
Synthesis
Prekallikrein Kallikrein
(Plasma) Hagman factor
(activated by collagen)
(plasma & tissues)
1.
Kininogen Bradykinin, Kallidin
(alpha-2 globulins Kallikrein (nonapeptide)(decapeptide)
High and low m.w. (Activated by peptidases)
Kallidin, a decapeptide, with same actions is also produced along with bradykinin. Both are metabolized to inactive agents by kinases II and ACE
BIOGENIC PEPTIDES
BRADYKININ & KALLIDIN
Receptors
B
1 mediates vasoconstriction, sensitive to metabolites.
B
2 mediates vasodilatation, permeability, smooth muscle contraction, pain
B
3 mediates guinea pig tracheal contraction, not antagonized by B
1 or B
2 antagonists.
SMALL PROTEINS
CYTOKINES (TNFa, IL-1,IL-6)
1. TNF
(Tumor Necrosis Factor
)
A mediator of endotoxic shock
Released by macrophages when exposed to endotoxin
Triggers wide endotoxemic symptoms
Elicits production of other cytokines, eicosanoids & humoral factors
Stimulates degradation and adherence of neutrophils to endothelium
Symptoms of septicemia at high concentration
Can be neutralized by TNF
antiserum
Chronic exposure leads to cachexia (TNF formerly known as cachectin ) was
SMALL PROTEINS
CYTOKINES
2. Interleukin-1 (IL-1)
Known as lymphocyte activating factor (
T-cell responses)
Activates endogenous pyrogen (induces fever)
Interacts synergestically with TNF
synthesis & release of IL-2 by interacting with antigen stimulated T-cells
Activates B-cells and antibody synthesis
arachidonic acid metabolism,
inflammatory proteins
neutrophil chemoattraction & fibroblast proliferation
PGI
2 synthesis in endothelial cells
SMALL PROTEINS
CYTOKINES
3. Interleukin-6 (IL-6)
A phosphoglycoprotein
Produced and secreted by macrophates, monocytes, fibroblasts
Inflammatory stimuli causes production by endothelium, T lymphocytes, mast cells
IL-6 induces production of hepatic fibrinogen for protection against microorganisms
Endotoxin, TNF alpha and IL-1 increase the levels of IL-6
Does not cause tissue injury or vascular thrombosis
Platelet Activating Factor (PAF)
General Information
•
Hanson (1971) identified a platelet aggregating agent
•
Same substance (
BP) was found in adrenal medulla
•
Phospholipase A
2 releases AA
& lysoPAF
from membrane
•
LysoPAF is acetylated by acetyl coenzyme A to PAF
(catalyzed by acetyl transferase)
•
Antigen-antibody reaction, chemotactic peptides, thrombin, collagen and other autacoids
synthesis.
•
Platelets, neutrophils, monocytes, mast cells, eosinophils, renal medullary cells and endothelium synthesize
PAF
PLATELET ACTIVATING FACTOR
Physiological functions
•
PAF in amniotic fluid derived from fetal lung.
•
It is a potent bronchoconstrictor (long lasting) & causes pulmonary edema
•
Simulates G proteins that are on the cell surface
•
This activates phospholipase C & A
2
•
Forms inositol phosphate, diacylglycerol and arachidonates
•
Thus,
PAF leads to the formation of PGs, LT and TXA
PAF
Pharmacological actions
•
Increases platelet aggregation
•
Potent vasodilator ,
PVR and
BP
•
Constricts pulmonary vessels
•
Microvascular permeability
•
Releases eicosanoids, generates superoxides
•
Contracts nonvascular smooth muscles ,
•
Increases respiratory secretions, forms pulmonary edema
•
Decreases renal flow
Nitric Oxide (NO)
Known as endothelium derived relaxing factor
(EDRF)
•
Organic nitrates (amyl nitrate, nitroglycerin, nitroprusside) release NO
•
Nitric Oxide Synthase (NOS) antagonists counteracts vascular relaxation
EFFECTS OF NO
•
Physiological vasodilator
• eNOS blockers increase BP by vasoconstriction
•
Macrophages kill microorganisms by NO
It causes: involved in penile erection
PHARMACOLOGIC MANIPULATION OF
NITRIC OXIDE
Inhibitors of Nitric Oxide Synthesis
•
In many disorders, such as inflammation and sepsis
• inhibition of the iNOS isoform is NEEDED
SEPTIC SHOCK increased urinary excretion of nitrate, the oxidative product of NO, is a feature of gramnegative bacterial infection.
•
Lipopolysaccharide components from the bacterial wall induce synthesis of iNOS, resulting in exaggerated hypotension, shock, and, in some cases, death.
•
This hypotension is reversed by NOS inhibitors such as L-NMMA in humans
•
A similar reversal of hypotension is produced by compounds that prevent the action of
NO (such as methylene blue
)
• as well as by scavengers of NO (such as hemoglobin
).
Nitric Oxide Donors
1. Organic nitrates Nitroglycerin
• metabolized to NO by mitochondrial aldehyde reductase, an enzyme enriched in venous smooth muscle,
.
2. Sodium nitroprusside generates NO in response to light as well as chemical or enzymatic mechanisms in cell membranes.
3. Hybrid NO donors
A new strategy involves the incorporation of NO-donating moieties onto currently available cardiovascular drugs. captopril. SNOCap, which incorporates a nitrosothiol moiety on captopril, is currently being examined for its efficacy in cardiovascular disorders
•
Nitric Oxide Donors
6. Alternate strategies
Sildenafil (VIAGRA)
- inhibitor of type 5 phosphodiesterase
- results in prolongation of the duration of NOinduced cGMP elevations in a variety of tissues
Endothelin
potent vasoconstrictor peptides that were first isolated from aortic endothelial cells.
Receptors:
ET
B causes transient drop in BP
ET
A causes prolonged increases in BP
endothelin receptor antagonists
Bosentan is a nonselective antagonist
Endothelin ANTAGONIST
Bosentan
is currently approved for use in pulmonary hypertension
ADVERSE EFFECTS OF Bosentan
1-Bosentan has been associated with fatal hepatotoxicity patients taking this drug must have monthly liver function tests.
2- Negative pregnancy test results are required for women of childbearing age to take this drug