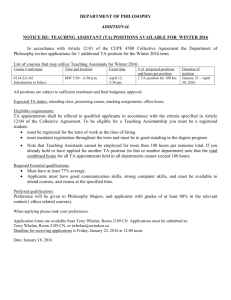
Body System Adverse Effects
advertisement

DRUGS AFFECTING THE CENTRAL NERVOUS SYSTEM Chap. 11, 13, 15, 16, 17 Winter 2013 3/19/2016 1 BRAIN AND SPINAL CORD PRIMARY FUNCTION – CONTROLS AND COORDINATES THE BODY AND BODY SYSTEMS DRUGS CAN: ALTER BEHAVIOR / CONSCIOUSNESS › BY STIMULATING OR DEPRESSING CNS – FOR DESIRED AFFECT Winter 2013 3/19/2016 2 A substance (norepinephrine, acetylcholine, dopamine, or hormone) that is released when the terminal axon of a presynaptic neuron is excited and acts by exciting or inhibiting a target cell. Winter 2013 3/19/2016 3 DEPRESS CNS STIMULATE CNS – DRUGS CAN ◦ DRUGS CAN CAUSE THE BRAIN TO BE CALM SLEEP ANESTHESIA COMA DEATH ◦ STIMULATE RESPIRATIONS ◦ KEEP A PATIENT AWAKE ◦ DEPRESS APPETITE Winter 2013 3/19/2016 4 ACUTE V. CHRONIC PAIN › ACUTE OCCURS QUICKLY, IS SHORT IN DURATION USUALLY CAN BE RESOLVED › CHRONIC – LONGER LASTING, USUALLY AT LEAST 3 MONTHS IN DURATION POSSIBLY WILL NOT GO AWAY PAIN IS THE SIXTH (6th) VITAL SIGN Winter 2013 3/19/2016 5 CAUSES OF PAIN / DISCOMFORT ◦ TRAUMA ◦ TISSUE DAMAGE ◦ PRESSURE ON TISSUE AND NERVES ◦ INFLAMMATION OF TISSUES AND NERVES Winter 2013 3/19/2016 6 Winter 2013 3/19/2016 7 ◦ MASSAGE ◦ POSITION CHANGE ◦ BIOFEEDBACK ◦ EXERCISE ◦ NON-OPOID ANALGESICS ◦ ANTIDEPRESSANTS ◦ Opioid ANALGESICS ◦ STEROIDS Winter 2013 3/19/2016 8 Pain relievers that contain opium, derived from the opium poppy or chemically related to opium Very strong pain relievers Very addicting Winter 2013 3/19/2016 9 codeine sulfate meperidine HCl (Demerol) methadone HCl (Dolophine) morphine sulfate propoxyphene HCl hydromorphone oxycodone fentanyl Many Others Winter 2013 3/19/2016 10 Bind to an Opioid receptor in the brain Cause an analgesic response (reduction of pain sensation) Winter 2013 3/19/2016 11 Main use: to alleviate moderate to severe pain Often given with adjuvant drugs to assist primary drugs with pain relief ◦ Muscle relaxant ◦ Sedative ◦ Alternate with non-narcotic analgesic Winter 2013 3/19/2016 12 Opioids’ are also used for: ◦ Cough center suppression ◦ Treatment of diarrhea ◦ Balanced anesthesia Winter 2013 3/19/2016 13 Known drug allergy Severe asthma Use with extreme caution if: Respiratory insufficiency Elevated intracranial pressure Morbid obesity Sleep apnea Paralytic ileus Winter 2013 3/19/2016 14 Euphoria CNS depression ◦ Leads to respiratory depression ◦ Most serious adverse effect Nausea and vomiting Urinary retention Diaphoresis and flushing Pupil constriction (miosis) Constipation Itching Winter 2013 3/19/2016 15 A common physiologic result of chronic Opioid treatment Result: larger dose is required to maintain the same level of analgesia Winter 2013 3/19/2016 16 Physiologic adaptation of the body to the presence of an Opioid Opioid tolerance and physical dependence are expected with long-term Opioid treatment and should not be confused with psychologic dependence (addiction) Winter 2013 3/19/2016 17 A pattern of compulsive drug use characterized by a continued craving for an Opioid and the need to use the Opioid for effects other than pain relief Winter 2013 3/19/2016 18 Misunderstanding of these terms leads to ineffective pain management and contributes to the problem of undertreatment Physical dependence is seen when the Opioid is abruptly discontinued or when an Opioid antagonist is administered Opioid withdrawal/Opioid abstinence syndrome Winter 2013 3/19/2016 19 Reverse the effects of these drugs on pain receptors Bind to a pain receptor and exert no response Also known as competitive antagonists Winter 2013 3/19/2016 20 ANALEPTICS naloxone (Narcan) naltrexone (Revia) These drugs bind to opiate receptors and prevent a response Used for complete or partial reversal of Opioid-induced respiratory depression Regardless of withdrawal symptoms, when a patient experiences severe respiratory depression, an Opioid antagonist should be given. Winter 2013 3/19/2016 21 ADMINISTER MEDICATION VERY SLOWLY ◦ ANTICIPATE PATIENT RESPONSE TO TREATMENT MONITOR PATIENT VERY CLOSELY ◦ VITAL SIGNS, RESPIRATORY RATE, PULSE OX CONTINUE TO MONITOR CLOSELY ◦ ½ LIFE OF NARCAN = 60 – 90 MINUTES ◦ ½ LIFE OF MORPHINE = 2 – 4 HOURS Winter 2013 3/19/2016 22 Symptoms of “Abstinence Syndrome” Pulmonary edema Withdrawal symptoms Nausea Vomiting Agitation Anxiety Confusion Pain Winter 2013 3/19/2016 23 Oral forms should be taken with food to minimize gastric upset Ensure safety measures, such as keeping side rails up, to prevent injury Withhold dose and contact physician if there is a decline in the patient’s condition or if vital signs are abnormal, especially if respiratory rate is less than 10 to 12 breaths/min Winter 2013 3/19/2016 24 Check dosages carefully Follow proper administration guidelines for IM injections, including site rotation Follow proper guidelines for IV administration, including dilution and rate of administration Winter 2013 3/19/2016 25 Constipation is a common adverse effect and may be prevented with adequate fluid and fiber intake Instruct patients to follow directions for administration carefully and to keep a record of their pain experience and response to treatments Patients should be instructed to change positions slowly to prevent possible orthostatic hypotension Winter 2013 3/19/2016 26 Decreased complaints of pain Decreased severity of pain Increased periods of comfort Improved activities of daily living, appetite, and sense of well-being Decreased fever (acetaminophen) Winter 2013 3/19/2016 27 Contact physician immediately if vital signs change, patient’s condition declines, or pain continues Respiratory depression may be manifested by respiratory rate of less than 10 breaths/min, dyspnea, diminished breath sounds, or shallow breathing Winter 2013 3/19/2016 28 Opioid agonist Schedule II narcotic Pregnancy Category C Given orally or parenterally Half life 2 – 4 hours Used for severe pain (chronic or acute) Winter 2013 3/19/2016 29 Indications Relief of severe/acute/chronic pain, analgesia during labor. Morphine is the drug of choice for pain due to Myocardial Infarction, dyspnea from pulmonary edema not resulting from chemical respiratory irritant. Winter 2013 3/19/2016 30 Contraindications Severe respiratory depression, acute/severe asthma, severe hepatic/renal impairment. Used with extreme caution in COPD, hypoxia, head injury, increased intracranial pressure Winter 2013 3/19/2016 31 Drug-Drug Interactions ◦ Use with EXTREME CAUTION in patients taking MAOIs ◦ Increased CNS depression and hypotension with alcohol, sedatives, hypnotics, barbiturates, tricyclic antidepressants, antihistamines ◦ May INCREASE the anticoagulant effect of Warfarin (Coumadin) Winter 2013 3/19/2016 32 › CNS Impaired judgment Drowsiness (decrease in LOC) Decrease in respiratory effort Winter 2013 3/19/2016 33 Gastrointestinal ◦ Dry mouth ◦ Nausea, vomiting ◦ Decreased intestinal peristalsis Winter 2013 3/19/2016 34 CARDIOVASCULAR (CV) › Bradycardia › Vasodilation › Tachycardia › Flushing Winter 2013 3/19/2016 35 GENITOURINARY ◦ URINARY RETENTION ALLERGIC ◦ RASH ◦ ITCHING RESPIRATORY ◦ RESPIRATORY DEPRESSION Winter 2013 3/19/2016 36 Concurrent use of: Kava kave Valerian root Camomile ◦ Can result in increased CNS depression Winter 2013 3/19/2016 37 IV PO IM IN (intra-nasal) SC (SQ) TRANSDERMAL EPIDURAL RECTAL Winter 2013 3/19/2016 38 INTRAVENOUS › Effective within 5 – 10 min. Of administration › Most common route (in hospitalized patients) › Frequently administered as patient controlled analgesia (PCA) Winter 2013 3/19/2016 39 DOUBLE LOCK SYSTEM › TIME › AMOUNT NURSE MUST DOCUMENT: › AMOUNT USED › EFFECTIVENESS › VITAL SIGNS INCLUDING RESPIRATIONS › ANY UNTOWARD EFFECTS › TEACH FAMILY ABOUT USE AND ABUSE Winter 2013 3/19/2016 40 Winter 2013 3/19/2016 41 Winter 2013 3/19/2016 42 Catheter is placed into the epidural space to inject a narcotic or anesthetic drug ◦ Obstetrics ◦ Surgical procedures ◦ Pain management Catheter may be left in for follow up injections by physician or patient controlled analgesia Winter 2013 3/19/2016 43 SEVERE PAIN – CHRONIC PAIN › FENTANYL PATCH (DURAGESIC) MOST COMMON Slower onset but more consistent pain relief Patch usually changed every 72h Treated just as any other narcotic – must account for every patch Patch must be dated, timed and signed when placed Old patch must be removed when the new one is placed Winter 2013 3/19/2016 44 Winter 2013 3/19/2016 45 Assess effectiveness of medication ◦ Use the 0 – 10 scale to measure intensity of pain Assess for adverse effects ◦ Assess rate, depth, and rhythm of RESPIRATIONS Provide for patient safety Winter 2013 3/19/2016 46 Blocks acetylcholine at the neuro-muscular junction Produces paralysis Does NOT effect LOC Drugs include: ◦ Pancuronium ◦ Succinycholine ◦ Vecuronium Winter 2013 3/19/2016 47 Used for uncomfortable procedures such as: ◦ ◦ ◦ ◦ Colonoscopy Endoscopy X-ray procedures Minor surgery Patient is unconscious but still able to protect their airway Amnesia is common midazolam (Versed) lorazepam (Ativan) Winter 2013 3/19/2016 48 Chapter 13 CNS depressants and muscle relaxants Winter 2013 3/19/2016 49 Sedative effect: ◦ Given during waking hours May cause drowsiness Hypnotic effect: ◦ Given at bedtime with the purpose of inducing sleep MAY BE THE SAME DRUG GIVEN AT DIFFERENT DOSAGES Winter 2013 3/19/2016 50 Prototype › Diazepam (Valium) Antianxiety, anticonvulsant, sedative/hypnotic, skeletal muscle relaxant Schedule IV drugs – Moderate potential for abuse Pregnancy category D Half-life 20-50 hours (metabolites also cause sedation up to 100 hours) Drug of choice to treat status epilepticus (sustained seizures) Winter 2013 3/19/2016 51 alprazolam (Xanax) chlordiazepoxide (Librium) flurazepam (Dalmane) lorazepam (Ativan) midazolam (Versed) triazolam (Halcion) Winter 2013 3/19/2016 52 MECHANISM OF ACTION ◦ Binds with benzodiazepine receptors in nerve cells of the brain; these cells also have binding sites for GABA (gamma-aminobutyric acid) which is an inhibitory neurotransmitter. Excitatory v. Inhibitory transmitters ◦ Excitatory – Norepinephrine ◦ Inhibitory - GABA Winter 2013 3/19/2016 53 Benzodiazapines and barbiturates work by increasing the action of gaba in the brain Gaba is an amino acid that inhibits nerve transmissions in the brain Winter 2013 3/19/2016 54 Indications – Not all drugs are appropriate for all uses ◦ Antianxiety ◦ Hypnotic ◦ Anticonvulsant ◦ Preoperative sedation ◦ Prevent DTs in alcohol withdrawal Winter 2013 3/19/2016 55 Contraindications ◦ Respiratory depression ◦ Liver disorder ◦ Kidney disorder ◦ History of alcohol or drug abuse ◦ Used cautiously with other CNS depressants Winter 2013 3/19/2016 56 Drug-Drug interactions ◦ Cimetidine, hormonal contraceptives, disulfiram, fluoxetine, isoniazid, ketoconazole, metoprolol, propoxyohene, propranolol, and valproic acid may enhance the effects of sedatives by decreasing their metabolism. ◦ May decrease the efficacy of levodopa ◦ Rifampin, barbiturates may increase the metabolism of benzodiazepines, decreasing their effectiveness. Winter 2013 3/19/2016 57 Herbal products to avoid when using benzodiazepines ◦ Kava kava ◦ Valerian root ◦ Camomile CAN INCREASE SEDATION THIS APPLIES TO ALL CNS DEPRESSANTS Winter 2013 3/19/2016 58 Adverse Effects ◦ CNS depression – drowsiness, lightheadedness ◦ Paradoxical effects – insomnia, excitation ◦ Respiratory depression ◦ Hypotension ◦ Constipation/diarrhea ◦ Nausea, vomiting ◦ Rash Winter 2013 3/19/2016 59 REVERSAL AGENT FOR OVERDOSE OF BENZODIAZEPINES: FLUMAZENIL ◦ INDICATED FOR THE REVERSAL OF MODERATE SEDATION OR GENERAL ANESTHIA Winter 2013 3/19/2016 60 ASSESS PATIENT WITH FOCUS ON REASON FOR GIVING SEDATION › ANXIETY › NERVOUSNESS REASSESS PATIENT FOR RESPONSE TO DRUG › SEDATIVE Q 4-6 H › HYPNOTIC AT BEDTIME MONITOR VS AND POTENTIAL FOR DEPRESSION Winter 2013 3/19/2016 61 Patient with a history or current use of recreational drugs or alcohol abuse Respiratory compromise Pregnancy or lactation Winter 2013 3/19/2016 62 Administer accurately ◦ Teach patient about expected effects and possible side effects ◦ Provide for patient safety Observe for therapeutic effects ◦ Decrease in anxiety ◦ Positive signs of sleep Winter 2013 3/19/2016 63 Observe for adverse effects ◦ Excessive sedation ◦ Hypotension Observe for drug interactions ◦ Concurrent use of other cns depressants Winter 2013 3/19/2016 64 ALCOHOL Winter 2013 3/19/2016 65 Stimulant and depressant ◦ Stimulates the adrenal gland ◦ Depresses the CNS Physical manifestations ◦ ◦ ◦ ◦ ◦ Acts as a diuretic Increases gastric acidity Cardiomyopathy Peripheral vasodilation Electrolyte imbalance Winter 2013 3/19/2016 66 Delirium tremens – Latin for “shaking frenzy” Abrupt alcohol (ETOH) withdrawal Mismatch between excitatory (norepinephrine) and inhibitory (GABA) receptors in the brain Winter 2013 3/19/2016 67 ◦ Confusion ◦ Diarrhea ◦ Insomnia ◦ Disorientation ◦ Agitation ◦ Fever ◦ Tachycardia ◦ Hypertension ◦ Visions of insects ◦ Severe anxiety ◦ Fear of death Winter 2013 3/19/2016 68 Many safety issues Do not mix with other CNS depressants Monitor patients’ liver function Patient may have altered clotting factors Patient may have withdrawal symptoms Winter 2013 3/19/2016 69 PSYCHOTHERAPEUTIC MEDICATIONS Winter 2013 3/19/2016 70 A group of mental disorders characterized by a vague uneasy feeling of discomfort or dread. The symptoms of anxiety prevent the individual from normal functioning . can be an exaggerated response to an actual event or anxiety unrelated to an identifiable event or condition. Winter 2013 3/19/2016 71 ◦ Panic disorder ◦ Generalized anxiety disorder ◦ Obsessive-compulsive disorder ◦ Post-traumatic stress disorder ◦ Simple phobia ◦ Social phobia Winter 2013 3/19/2016 72 Tricyclic antidepressants Benzodiazepines MAOIs Buspirone SSRIs Winter 2013 3/19/2016 73 Mechanism of action – unknown ◦ Interacts with serotonin and dopamine in the brain ◦ No muscle relaxant effects ◦ No anticonvulsant effects ◦ Does not cause sedation Winter 2013 3/19/2016 74 Uses / indications ◦ Short term management of anxiety disorders ◦ Not appropriate for immediate relief – may take several weeks to see effects Winter 2013 3/19/2016 75 Side effects ◦ Dizziness, nausea, headache, anxiety, fatigue, insomnia Contraindications ◦ Renal/hepatic failure ◦ Use of MAOIs Winter 2013 3/19/2016 76 ANTIDEPRESSANTS AND MOOD STABILIZERS DRUGS Winter 2013 3/19/2016 77 Monoamine neurotransmitter dysfunction ◦ Deficiency of norepinephrine and/or serotonin. ◦ Balance, integration and interactions among norepinephrine, serotonin, and other neurotransmission systems is an important etiological factors. Winter 2013 3/19/2016 78 Neuroendocrine factors ◦ AN INCREASE IN CRF (corticotropin releasing factor/hormone) HAS BEEN NOTED IN PATIENTS WITH DEPRESSION. Winter 2013 3/19/2016 79 Tricyclic antidepressants Monoamine oxidase inhibitors Selective serotonin reuptake inhibitors Unclassified drugs Winter 2013 3/19/2016 80 imipramine (Tofranil) prototype nortriptyline (Pamelor) amitryptyline (Elavil) desipramine (Norpramin) Winter 2013 3/19/2016 81 Winter 2013 3/19/2016 82 First generation of antidepressant therapy Mechanism of action › Corrects the imbalance in the neurotransmitter concentrations of serotonin and norepinephrine at the nerve endings in the CNS. This is done by blocking the reuptake of the neurotransmitters and thus causing these neurotransmitters to accumulate at the nerve endings. › Also have nonselective receptor antagonism causing many side effects. Winter 2013 3/19/2016 83 Indications ◦ Depression ◦ Childhood enuresis(bed wetting) Imipramine ◦ Obsessive compulsive disorder Clomipramine ◦ Chronic pain syndromes Neuropathic pain (trigeminal neuralgia) Winter 2013 3/19/2016 84 Adverse effects ◦ Sedation ◦ Impotence ◦ Orthostatic hypotension ◦ Disturbs cardiac conduction ◦ Delayed micturation ◦ Edema ◦ Muscle tremors Winter 2013 3/19/2016 85 Interactions ◦ WHEN TAKEN WITH MAOIs MAY RESULT IN INCREASED THERAPEUTIC LEADING TO TOXIC EFFECTS (HYPERPYRETIC CRISIS) ◦ TCAs can inhibit the metabolism of warfarin, resulting in an increase in anticoagulation Winter 2013 3/19/2016 86 Toxicity and management of overdose ◦ TCA overdoses are fatal 70% - 80% of the time ◦ Death usually results from seizures or dysrhythmias ◦ THERE IS NO SPECIFIC ANTIDOTE FOR TCAs Winter 2013 3/19/2016 87 First generation of antidepressant drugs ◦ Highly effective ◦ Many side effects and drug/drug, drug/food interactions ◦ Disadvantage: potential to cause hypertensive crisis when taken with tyramine Winter 2013 3/19/2016 88 phenelzine (Nardil) tranylcypromine (Parnate) Winter 2013 3/19/2016 89 Winter 2013 3/19/2016 90 Inhibit the MAO enzyme system in the CNS Amines (dopamine, serotonin, norepinephrine) are not broken down, resulting in higher levels in the brain Result: alleviation of symptoms of depression Winter 2013 3/19/2016 91 Depression, especially types characterized by symptoms such as increased sleep and appetite depression that does not respond to other drugs such as tricyclics Winter 2013 3/19/2016 92 Tachycardia Dizziness Insomnia Anorexia Blurred vision Palpitations Drowsiness Headache Nausea Impotence Winter 2013 3/19/2016 93 Symptoms appear 12 hours after ingestion Tachycardia, circulatory collapse, seizures, coma Treatment: protect brain and heart, eliminate toxin Winter 2013 3/19/2016 94 Ingestion of foods and/or drinks with the amino acid tyramine leads to hypertensive crisis, which may lead to cerebral hemorrhage, stroke, coma, or death Winter 2013 3/19/2016 95 Avoid foods that contain tyramine! Aged, mature cheeses (cheddar, blue, Swiss) Smoked/pickled or aged meats, fish, poultry (herring, sausage, corned beef, salami, pepperoni, pâté) Yeast extracts Red wines (Chianti, burgundy, sherry, vermouth) Italian broad beans (fava beans) Winter 2013 3/19/2016 96 Concurrent use of MAOIs and SSRIs may lead to serotonin syndrome If the decision is made to switch to an SSRI, there must be a 2- to 5-week “washout” period between MAOI therapy and SSRI therapy Winter 2013 3/19/2016 97 Delirium Tachycardia Hyper-reflexia Shivering Agitation Sweating Muscle spasms Coarse tremors More severe cases Hyperthermia Renal failure Rhabdomyolysis Dysrhythmias Seizures DIC Winter 2013 3/19/2016 98 fluoxetine (Prozac) paroxetine (Paxil) sertraline (Zoloft) fluvoxamine (Luvox) citalopram (Celexa) escitalopram (Lexapro) Winter 2013 3/19/2016 99 Fewer adverse effects than tricyclics and MAOIs Very few drug-drug or drug-food interactions Still takes about 4 to 6 weeks to reach maximum clinical effectiveness Winter 2013 3/19/2016 10 0 Mechanism of action Selectively inhibits serotonin reuptake Little or no effect on norepinephrine or dopamine reuptake Result in increased serotonin concentrations at nerve endings Advantage over tricyclics and MAOIs: little or no effect on cardiovascular system Winter 2013 3/19/2016 10 1 INDICATIONS ◦ Depression ◦ Bipolar disorder ◦ Obesity ◦ Eating disorders ◦ Obsessive-compulsive disorder Winter 2013 3/19/2016 102 Winter 2013 3/19/2016 10 3 Body System Effects CNS Headache, dizziness, tremor, nervousness, insomnia,* fatigue Nausea, diarrhea, constipation, dry mouth Sexual dysfunction, * weight gain,* weight loss, sweating GI Other * Most common and bothersome Winter 2013 3/19/2016 10 4 Duloxetine (Cymbalta) Venlafaxine (Effexor) Winter 2013 3/19/2016 105 Indicated ◦ For depression and general anxiety disorder ◦ Also pain associated with diabetic peripheral neuropathy Contraindicated ◦ CONCURRENT USE OF MAOIs ◦ Angle closure glaucoma Winter 2013 3/19/2016 106 Drug Interactions ◦ Highly bound to plasma proteins ◦ Compete with other protein-binding drugs, resulting in more free, unbound drug to cause a more pronounced drug effect ◦ Inhibition of cytochrome P-450 system Winter 2013 3/19/2016 107 bupropion ◦ Wellbutrin, zyban Commonly prescribed for smoking cessation maprotiline ◦ Similar to TCAs Mirtazapine ◦ Remeron Often prescribed to enhance appetite Winter 2013 3/19/2016 108 Comprehensive patient history Complete medication history Monitor patient for therapeutic effects Monitor patients for adverse effects Education of patient on drug expectations and adverse effects Educate patient regarding drug-drug, drug-food and drug-herbal interactions Winter 2013 3/19/2016 109 lithium carbonate Eskalith, lithobid ◦ MOA – not completely understood Managed using serum levels ◦ Indications – mania, bipolar disorder ◦ Adverse effects vomiting, diarrhea, drowsiness, difficult coordination, hand tremors, muscle twitching, mental confusion Winter 2013 3/19/2016 110 Monitor serum lithium levels ◦ Therapeutic levels are 1.0 – 1.5 meq/L Lithium is eliminated intact by the kidneys. Encourage fluids to completely eliminate the drug Monitor for therapeutic and adverse effects Winter 2013 3/19/2016 111 A severe mental disorder characterized by disordered thought process and often bizarre thinking. Hypoactivity or hyperactivity Agitation Aggressiveness Hostility Social withdrawal Winter 2013 3/19/2016 112 Antipsychotic AKA Neuroleptic: ◦ Any drug that modifies or treats psychotic behaviors usually by blocking dopamine receptors in the brain Winter 2013 3/19/2016 113 Thioxanthenes thiothixene (Navane) Phenylbutylpiperidines haloperidol (Haldol) Dihydroindolones molindone (Moban) Dibenzodiazepines loxapine (Loxitane) Benisoxazoles Risperidone Quinolinine Aripiprazole (Abilify) Phenothiazines Chlorpromazine (Thorazine) Winter 2013 3/19/2016 114 Schizophrenia ◦ Long half-life facilitates better compliance by patients Long-term treatment of psychosis Can be given either IV or po Winter 2013 3/19/2016 116 Seizures Extrapyramidal reactions Blurred vision, dry eyes Neuroleptic malignant syndrome Tartive dyskinesia Winter 2013 3/19/2016 117 A potentially fatal syndrome with symptoms: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Hyperthermia Catatonic rigidity Altered mental status Profuse sweating Rhabdomyolysis Renal failure Seizures Death Winter 2013 3/19/2016 11 8 ◦ Involuntary contractions of oral and facial muscles ◦ Choreoathetosis (wavelike movements of extremities) ◦ Occurs with continuous long-term antipsychotic therapy (esp. phenothiazines) Winter 2013 3/19/2016 119 ◦ Involuntary muscle symptoms similar to those of Parkinson’s disease ◦ Akathisia (distressing muscle restlessness) ◦ Acute dystonia (painful muscle spasms) ◦ Treated with benztropine (Cogentin) and trihexyphenidyl (Artane) Winter 2013 3/19/2016 120 Recognizing extrapyramidal symptoms http://www.youtube.com/watch?v=WAg2iLEWVh0 &playnext=1&list=PLFA09E8C6FCF4EC70&featur e=results_main Winter 2013 3/19/2016 121 clozapine (Clozaril) risperidone (Risperdal) olanzapine (Zyprexa) quetiapine (Seroquel) ziprasidone (Geodon) aripiprazole (Abilify) Winter 2013 3/19/2016 122 Block dopamine receptors in the brain (limbic system, basal ganglia)—areas associated with emotion, cognitive function, motor function Dopamine levels in the CNS are decreased Result: tranquilizing effect in psychotic patients Winter 2013 3/19/2016 123 ◦ Reduced effect on Prolactin levels Stimulates mammary glands to produce milk ◦ Lower risk of Neuroleptic malignant syndrome Extrapyramidal adverse effects Tartive dyskinesia Winter 2013 3/19/2016 124 Treatment of serious mental illnesses ◦ ◦ ◦ ◦ Bipolar affective disorder Depressive and drug-induced psychoses Schizophrenia Autism Movement disorders (such as Tourette’s syndrome) Some medical conditions ◦ Nausea, intractable hiccups Winter 2013 3/19/2016 125 Body System CNS Cardiovascular Dermatologic Adverse Effects Sedation, delirium Orthostatic hypotension, syncope, dizziness, EKG changes Photosensitivity, skin rash, hyper-pigmentation, pruritus Winter 2013 3/19/2016 126 Body System Adverse Effects GI Dry mouth, constipation GU Urinary hesitancy or retention, impaired erection Hematologic Leukopenia and agranulocytosis Winter 2013 3/19/2016 127 Body System Metabolic/endocrine Adverse Effects Galactorrhea, irregular menses, increased appetite, polydipsia Winter 2013 3/19/2016 128 Before beginning therapy, assess both the physical and emotional status of patients Obtain baseline vital signs, including postural BP readings Obtain liver and renal function tests Winter 2013 3/19/2016 129 Assess for possible contraindications to therapy, cautious use, and potential drug interactions Assess LOC, mental alertness, potential for injury to self and others Check the patient’s mouth to make sure oral doses are swallowed Winter 2013 3/19/2016 130 Provide simple explanations about the drug, its effects, and the length of time before therapeutic effects can be expected Abrupt withdrawal should be avoided Advise patients to change positions slowly to avoid postural hypotension and possible injury Winter 2013 3/19/2016 131 The combination of drug therapy and psychotherapy is emphasized because patients need to learn and acquire more effective coping skills Only small amounts of medications should be dispensed at a time to minimize the risk of suicide attempts Simultaneous use of these drugs with alcohol or other CNS depressants can be fatal Winter 2013 3/19/2016 132 Skeletal muscle relaxants are used to decrease muscle spasm or spasticity that occurs in certain neurologic and musculoskeletal disorders. Winter 2013 3/19/2016 133 Indications › Relief of painful musculoskeletal conditions Muscle spasms Management of spasticity of severe chronic disorders Multiple sclerosis, cerebral palsy › Work best when used along with physical therapy Winter 2013 3/19/2016 134 Muscle spasms ◦ Sudden involuntary muscle contraction ◦ Can occur secondary to trauma, inflammation, sprains, strains, arthritis, spinal disorders Winter 2013 3/19/2016 135 MECHANISM OF ACTION Act to relieve pain associated with skeletal muscle spasms Majority are central acting ◦ CNS is the site of action ◦ Similar in structure and action to other CNS depressants Direct acting ◦ Acts directly on skeletal muscle ◦ Closely resembles GABA (an inhibitory neurotransmitter) Winter 2013 3/19/2016 136 baclofen (Lioresal) cyclobenzaprine (Flexeril) carisoprodol (Soma) metaxalone (Skelaxin) methocarbamol (Robaxin) tizanidine (Zanaflex) DIRECT ACTING dantrolene (Dantrium) Winter 2013 3/19/2016 137 Muscle spasticity ◦ Spasticity involves increased muscle tone or contraction ◦ Can occur secondary to spinal cord injury, multiple sclerosis, cerebral palsy, muscular dystrophy Winter 2013 3/19/2016 138 Extension of effects on CNS and skeletal muscles ◦ Euphoria ◦ Lightheadedness ◦ Dizziness ◦ Drowsiness ◦ Fatigue ◦ Muscle weakness, others Winter 2013 3/19/2016 139 Nursing implications ◦ Monitor therapeutic response to medication ◦ Monitor for adverse reactions ◦ Nursing diagnosis appropriate to specific patient Winter 2013 3/19/2016 140 Anticonvulsants Antiseizure drugs Antiepileptic drugs (AEDs) Chapter 15 MEDICATION TO CONTROL SEIZURES Winter 2013 3/19/2016 141 A brief episode of abnormal electrical activity of nerve cells in the brain Winter 2013 3/19/2016 142 Winter 2013 3/19/2016 143 Winter 2013 3/19/2016 14 4 GOAL OF TREATMENT ◦ Control seizures without causing undue sedation and experiencing minimal adverse reactions Winter 2013 3/19/2016 14 5 DRUGS TO CONTROL SEIZURES CARBAMAZAPINE TEGRETOL CLONAZEPAM KLONOPIN FOSPHENYTOIN CEREBYX GABAPENTIN NEURONTIN CHLORAZEPATE LORAZEPAM DIAZEPAM VALIUM PHENYTOIN (PROTOTYPE) LUMINAL VALPROIC ACID TRANXENE PHENOBARBITAL ATIVAN DILANTIN DEPAKENE Winter 2013 3/19/2016 146 FIRST USED IN 1903 › PHENOBARBITAL MOST COMMONLY PRESCRIBED FOR STATUS EPILEPTICUS MORE OFTEN USED IN NONINDUSTRIALIZED COUNTRIES BECAUSE OF LOW COST CLINICAL CLASSIFICATION – ANTICONVULSANT, HYPNOTIC LONG HALF-LIFE Winter 2013 3/19/2016 147 Classification ◦ Anticonvulsant ◦ Antiarrhythmic MOA ◦ Stabilize neuronal membranes in the motor cortex of the brain. Limits the spread of seizure activity Winter 2013 3/19/2016 148 Contraindications › Seizures caused by hypoglycemia or high fever Side effects › Drowsiness, lethargy, confusion, slurred speech › Gingival hyperplasia › Fever, rash, lymphadenopathy Monitor serum dilantin levels › 10 -20 mcg/ml IS THERAPEUTIC Monitor liver function Decreases many drug levels including oral contraceptives Winter 2013 3/19/2016 149 Winter 2013 3/19/2016 15 0 NURSING CONSIDERATIONS ◦ REVIEW HISTORY OF SEIZURES ◦ INITIATE SEIZURE PRECAUTIONS ◦ PATIENT EDUCATION WHAT TO EXPECT FROM MEDICATION DO NOT EVER OMIT A DOSE MUST MAINTAIN THERAPEUTIC BLOOD LEVELS OR SEIZURES WILL RECUR ◦ SEE “NURSING PROCESS – ASSESSMENT” P.238 ◦ DOCUMENT TYPE AND CHARACTER OF SEIZURE Winter 2013 3/19/2016 151 Classification: ◦ Anticonvulsant ◦ Vascular headache suppressant Mechanism of action ◦ Increases levels of gaba in the CNS Adverse reactions Winter 2013 3/19/2016 152 Adverse reactions Agitation Dizziness Headache Insomnia Sedation Visual disturbances Tremor Ataxia Winter 2013 3/19/2016 153 Classification – anticonvulsant Mechanism of action ◦ Alters ion transport in the CNS Indicated for short term management of generalized seizures, status epilepticus Parenteral administration only Winter 2013 3/19/2016 154 Indications – treatment of clonic-tonic, mixed and complex seizures Mechanism of action – decreases synaptic transmission in the CNS by affecting sodium channels in the neurons Winter 2013 3/19/2016 155 Adverse reactions Ataxia Drowsiness Drug-drug interactions ◦ Many Drug food interactions ◦ Grapefruit juice increases serum levels and increases the drug effects (toxicity?) THERAPEUTIC SERUM DRUG LEVELS – 4-12mcg/ml Winter 2013 3/19/2016 156 Winter 2013 3/19/2016 15 7 DRUGS FOR PARKINSON’S DISEASE Winter 2013 3/19/2016 158 Progressive, degenerative neurologic disorder caused by a imbalance between acetylcholine and dopamine in the brain Winter 2013 3/19/2016 159 Winter 2013 3/19/2016 160 Winter 2013 3/19/2016 161 Signs and symptoms › Shuffling gait › Fine tremors › Muscle rigidity › Slurred speech › Emotionless facial expression (mask-like) › Difficulty chewing and swallowing Winter 2013 3/19/2016 162 Anticholinergic drugs Antihistamines Dopaminergic’s ◦ Direct acting dopamine receptor agonists ◦ Indirect acting dopamine receptor agonists Winter 2013 3/19/2016 163 benztropine, procyclidine, trihexyphenidyl ◦ Drugs that block the effects of acetylcholine As dopamine decreases, acetylcholine increases causing muscle tremors and rigidity (more pronounced at rest) Pill rolling Winter 2013 3/19/2016 164 Anticholinergic effects DECREASE: ◦ Salivation ◦ Tearing of the eyes, ◦ Urination ◦ Diarrhea ◦ Increased GI motility ◦ Emesis (vomiting) Winter 2013 3/19/2016 165 Contraindications ◦ Known drug allergy ◦ GI or bladder obstruction ◦ Cardiac disease ◦ Glaucoma ◦ Myasthenia gravis Winter 2013 3/19/2016 166 Used for their anticholinergic effects ◦ diphenhydramine (Benadryl) Winter 2013 3/19/2016 167 Direct acting medication increase the levels of dopamine at the synapse. › bromocriptine – dopamine agonist › pergolide – dopamine agonist › pramipexole - dopamine agonist › levodopa – dopamine replacement Winter 2013 3/19/2016 168 Indirect acting increase dopamine levels by inhibiting enzymes that break down dopamine › Carbidopa – inhibits enzyme AADC › Entacapone – COMT inhibitor › Tolcapone – COMT inhibitor › Selegiline – MAOI Others › Amantadine – synthetic antiviral Winter 2013 3/19/2016 169 Levodopa (prototype) ◦ Precursor to dopamine Dopamine does not cross the blood-brain barrier. Can cross as levodopa and is then converted to dopamine Carbidopa ◦ Prevents the conversion of levodopa to dopamine in the peripheral tissues ◦ Does not cross the blood brain barrier Winter 2013 3/19/2016 170 ACTION OF MAO ◦ Primary roll is the catabolism or breakdown of catecholamines such as dopamine, norepinephrine and epinephrine. Also breaks down serotonin. Rasagiline (azilect) Winter 2013 3/19/2016 171 Catechol-o-methytransferase ◦ A naturally occurring enzyme in the body that breaks down dopamine molecules ◦ By inhibiting this enzyme, the action of levodopa is prolonged ◦ Medications: tolcapone (Tasmar) entacapone (Comtan) Winter 2013 3/19/2016 172 Drowsiness Confusion Orthostatic hypotension Dystonia Dyskinesia Winter 2013 3/19/2016 173 Risk for injury due to postural hypotension ◦ Rise slowly from sitting or lying position Difficulty with communication Safety issues r/t unsteady, shuffling gait Never stop meds abruptly Take meds on time Watch for adverse reactions Winter 2013 3/19/2016 174 ON – OFF: Disease is worsening, too little dopamine is present WEARING OFF: Gradual worsening of Parkinson’s symptoms as the drugs lose their effectiveness Winter 2013 3/19/2016 17 5