Introduction to Psychology - Warren Wilson Inside Page
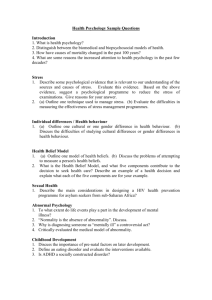
advertisement
Health Psychology What Do Health Psychologists Do? Teachers, research scientists, clinicians Applied health psychologists: licensed practitioners who focus on health-promoting interventions and helping people cope with illnesses Goals in Health Psych • Pinpoint Psychological, Behavioral, and Social Factors in Disease and Health • Promote and Maintain Health • Prevent and Treat Illness • Improve the Health Care System and Health Care Policy Where Do Health Psychologists Work? Training to become a Health Psychologist General psychology training at the undergraduate level Special training at the doctoral (Ph.D.) level Four- to six-year program 65 Ph.D. programs in health psychology in the United States Issues Issues and historical trends that have shaped the development of Health Psychology I. Increased Life Expectancy Average life expectancy — Increased by more than 30 years since 1900 In the U.S. in 21st century • Women: around 80 • Men: around 75 • Why is this increase important? II. Changes over the last 100 years The 10 Leading Causes of Death in The U.S. in 1900 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Pneumonia Tuberculosis Diarrhea and enteritis Heart disease Stroke Liver disease Injuries Cancer Senility Diphtheria Source: Centers for Disease Control and Prevention Leading causes of death (today) 1. 2. 3. 4. Heart disease Cancer Stroke Lung disease (COPD) 5. Accidents 6. Diabetes These top six account for 80% of deaths They are mostly lifestyle diseases with preventable causes They are mostly chronic disorders (rather than acute disorders) Source: U.S. National Center for Health Statistics Behavior and health Actual Causes of Death in the U.S. 1. Tobacco 2. Diet /activity patterns 3. Alcohol 4. Microbial agents 5. Toxic agents 6. Firearms 7. Sexual behavior 8. Motor vehicles 9. Illicit use of drugs Source: Journal of the American Medical Association III. Rising Health Care Costs IV. Trends in how illness has been viewed Western view (traditional) Biomedical model — illness is caused by physical phenomena (e.g., germs, cell abnormalities) -- reductionistic Biopsychosocial Perspective The view that health is determined by the interaction of biological mechanisms, psychological processes, and social influences Biological mechanisms: genes, evolutionary history, anatomical/biological makeup, nutrition Psychological processes: coping mechanisms, attitudes toward treatment, personality/outlook on life Social context: SES, social network, societal and cultural norms (e.g., pervasive consumption of soda) A Biopsychosocial Model of Depression The Biopsychosocial Model in practice Somatic presentations of psychological dysfunction Chest pain in panic attack Hypochondriasis Psychological conditions secondary to illness Post M.I. Depression Psychological sequelae of stroke Stress disorders associated with traumatic injuries The Biopsychosocial Model in practice Physical symptoms responsive to behavioral interventions anticipatory nausea enuresis tension & migraine headache early labor (clip from “The New Medicine”) The Biopsychosocial Model in practice Psychological presentations of organic problems hypothyroidism presenting as depression steroid-induced psychosis Somatic complications associated with behavioral factors mismanagement of diabetes noncompliance to medications The Biopsychosocial Model in practice Behavioral risk factors for disease or disability smoking excessive weight risk taking sedentary lifestyle Problems of health care providers and health care systems Physician-patient relationships Lack of access to health care The Biopsychosocial Model in practice (case studies) Small group exercise – using the BPS (then discuss assessment targets using the BPS – next slide) Biological Review current status of illness / background of illness (usually found in the medical history chart) medications pain family history lifestyle habits (e.g., nutrition and exercise) Psychological Review Affective/emotional Cognitive (e.g., thinking, beliefs, memory, attention, learning, interpreting, problemsolving) Motivation Social Review Patient’s interaction with health care staff Family / friends support Socioeconomic status (SES) Environment to which patient will return (job?) Cultural factors