Frank (pitting) edema
advertisement

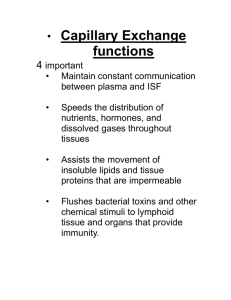
Isotonic overhydration(Edema) 1. Concept and classification 2. Causes and pathogenesis 3. Characteristics of edema 4. Effect on the body 5. Principles of treatment 1. Concept and classification (1) Concepts (synonyms) Edema is a pathologic process, edema is not a special disease. 1)The narrow sense of edema is the excessive fluid accumulated within the interstitial space. 2) The broad sense of edema is the excessive fluid accumulated within the interstitial space and cavity (includes hydrops). 3) Hydrops(积水) indicates specially the excessive fluid accumulated within the body cavities. ascites (peritoneal cavity), hydrothorax (pleural cavity) articular cavity (hydrarthrus) indicates specially excessive fluid accumulated within the cells 4) Cellular edema 5) Isotonic overhydration The edematous fluid is isotonic fluid. (2) Classification 1) According to the distribution of edematous fluid: (a) Local edema: Local edema occurs in one organ or a part of the body. (brain edema, pulmonary edema, etc). (b) Generalized edema: Generalized edema occurs in whole body (cardiac edema, renal edema, etc). 2) According to the causes of edema: cardiac edema renal edema hepatic edema idiopathic edema 3) According to the gravity of edema: recessive (non-pitting) edema; frank (pitting) edema. Frank (pitting) edema: By pressing finger firmly against the tissue for a few seconds, a dent can be produced. When the finger is withdrawn, the dent may persist for several minutes. 99% of interstitial fluid is fixed to collagen, mucopolysaccharide and hyaluronic acid (gel), (connective tissue), which called fixed water. 1% of interstitial fluid is free water (moving freely). 2. Causes and pathogenesis of edema Basic causes: (1) Imbalance of exchange between intra-vascular and extra-vascular fluid. (retention of water and sodium in the interstitial space) (2) Retention of fluid in the body. ( imbalance of exchange between intra- and extra-body fluid) (1) Imbalance of exchange between intra-vascular and extra-vascular fluid 1) Increased capillary hydrostatic pressure (CHP) 2) Decreased plasma colloidal OP 3) Increased permeability of the capillary wall 4) Obstruction of lymphatic return 5) Local factors against edema Basic concepts ① The capillary hydrostatic pressure (CHP) is the capillary blood pressure. CHP is the potential to drive the water from the vessel into interstitial space. CHP at the arterial end is 30 mmHg (hydrargyrum). CHP at venous end is 12mmHg. The mean CHP is 17mmHg. The interstitial hydrostatic pressure (-6.5 mmHg) is also called tissue tension, which is the potential to drive the water from interstitial compartment into the vessel. . The effective HP is the difference between capillary HP and interstitial HP. 30-(-6.5); 12-(-6.5); 17-(-6.5) The effective HP is the potential to drive the water out of the vessel. ② The colloid osmotic pressure (COP) is formed by the proteins in the solution. The serum COP (28 mmHg) is constituted by the proteins in the serum. The formation of COP depends on the number of protein particle. COP Albumin is the main factor for the serum COP. The albumin has the highest concentration and the lowest molecular weight, so albumin has the most particles in serum. ----------------------------------------------------------------------------------1g osmotic P. Content MW (mmHg) (g/100 ml serum) (KD) ----------------------------------------------------------------------------------albumin 5.5 3.5~4.5 <70 globulin 1.4 2.5~3.8 160(IgG) fibrinogen 1.0 0.2~0.4 >300 ----------------------------------------------------------------------------------- The interstitial COP (5mmHg) is formed by the proteins in the interstitial fluid. The effective COP is the difference between serum COP and interstitial COP. The net potential of effective COP is to maintain the water within the blood vessels. (285 mmHg) ③ The effective filtration pressure (EFP) is the difference between effective HP and effective COP. At the arterial end, the EFP is positive [30-(-6.5)23], which drives the water out. At the venous end, the EFP is negative [12-(-6.5)23] and droves the water in The mean EFP is 17-(-6.5)-23=0.5 mmHg and drives the water out of the vessel. There is a “net” force ( net flow) across the capillary wall. ④ Lymphatic return is another way for interstitial fluid to return back to venous circulation. The lymphatic return counteracts the net effect of EFP. pressure(mmHg) artery part (mean) vein part -----------------------------------------------------------------------------------capillary hydrostatic P. 30 (17) 12 tissue hydrostatic P. –6.5 (–6.5) -6.5 effective H.P. 36.5 (23.5) 18.5 - plasma colloidal O.P. tissue colloidal O.P. effective C.O.P. 28 5 23 effective filtration P. 13.5 0.5 -4.5 ------------------------------------------------------------------------------------- 1) Increased capillary hydrostatic pressure (CHP) (a)Causes ①Venous obstruction: Venous obstruction can be caused by venous congestion (thrombophlebitis, etc). ② Arteriolar dilation Arteriolar dilation can be seen in acute inflammation and allergic responses. More blood volume will increase CHP. ③ Increased vascular volume Increased vascular volume can occur in heart failure and pregnancy. Over-infusion. ④ Effect of gravity such as prolonged standing. (b)Mechanism of edema caused by increased CHP capillary hydrostatic pressure(CHP)↑ effect hydrostatic pressure(EHP)↑ effective filtration pressure(EFP)↑ interstitial fluid ↑. The increase of effective filtration pressure should overtakes the compensation of increased lymphatic return before edema occur. 2) Decreased plasma colloidal OP (a) Causes: ① Increased loss of plasma albumin, such as in extensive burn, nephrotic syndrome (10g protein/day), etc. ② Increased protein consumption in malignant tumors, chronic inflammation. ③ Decreased synthesis of plasma albumin, such as in hepatic dysfunction and starvation. ④ Dilution of serum protein due to over-infusion of water and sodium. (b) Mechanism of decreased COP leading to edema plasma colloidal OP↓ effective COP↓ Effective filtration pressure ↑ Interstitial fluid ↑ The increase of effective filtration pressure should overtakes the compensation of increased lymphatic return before edema occur. 3) Increased permeability of the capillary wall (a) Causes: ① In infection, the hyaluronidase released by bacteria can damage (hydrolyze the connective tissue) the capillary wall.. ② Hypoxia, acidosis, radiation damage, trauma and burn may lead to the degeneration of basement membrane of capillary. ③ Inflammatory media such as histamine(HA), kinins and 5-hydroxytryptamine(5-TH) may cause the contraction of microfilament in endothelial cells and the formation of “gap” between endothelial cells. ④Many irritant gases (chlorine, nitrogen peroxide, ozone) and high concentration of oxygen may damage the alveolar-capillary membrane and increase the permeability of the pulmonary capillaries. 氯气: 作用机理是溶于水后产生具有杀菌 能力的次氯酸,后者能释放出活性氯和新 生态氧而呈现强烈的氧化作用. 氧自由基作用. (b) Mechanism of leading to edema The increase of permeability of capillary wall ↑ effective filtration protein and fluid leak to interstitial pressure should space overtakes the tissue COP↑ plasma COP ↓ compensation of increased lymphatic effective COP↓ return before edema occur. effective filtration pressure↑ interstitial fluid ↑ (4) Obstruction of lymphatic return (a) Causes ① In the patients with mammary cancer, the subaxillary lymph nodes may be removed in the radical operation. ② The parasite enters into the lymphatic vessels in elephantiasis (丝虫性象 皮病)infestation. The edema caused by lymph obstruction is called lymph edema. (b) mechanism of lymph edema obstructed lymphatic vessels backflow of protein in interstitial fluid is blocked, the interstitial COP will increase effective COP decrease effective FP increase more fluid accumulates in interstitial space. 5) Local factors against edema ① The lymphatic return is increased rapidly, when the interstitial pressure begins to increase. The maximal potential of lymphatic return is to increase by 20 times.(7mmHg) ② When the lymphatic return is increased, more protein is washed back to venous circulation with lymph, the interstitial COP will reduce. The effective COP will increase, the EFP will decrease.(4mmHg) Recessive (non-pitting) edema will occur. ③ The normal negative interstitial fluid pressure must be lost before the frank edema can occur. The frank edema occurs after the interstitial pressure increasing from -6.5 to 0 mmHg with the emergence of free water. (2) Retention of fluid in the body Under normal circumstances, the intake and excretion of fluid is in dynamic balance, in which the kidneys play important role. Normally the filtrate from glomeruli is 180 liter/day. 60~70% of filtrate is reabsorbed at proximal tubules, finally 99%~99.5% of filtrate is reabsorbed by renal tubules, which is called glomerular-tubular balance. 1) Decreased glomerular filtration rate (GFR) GFR depends on: (a) filtration pressure (b) permeability of glomerular membrane (c) surface area of filtration The GFR is decreased, but the reabsorption of renal tubules is not reduced correspondingly. (a) Decreased filtration pressure, ① Decrease of glomerular blood flow: Decreased glomerular blood flow can be seen in decreased effective blood volume due to heart failure. •② Constriction of afferent arterioles: • • Constriction of afferent arterioles can be caused by increased sympathetic excitability. (b) Reduction of permeability of glomerular membrane: Reduction of permeability of glomerular membrane can be seen in chronic glomeronephritis with proliferative changes mesangium and progressive thickening of capillary wall. The GFR will reduce. The urine volume will reduce, if the reabsorption is not reduced. (c) Decreased filtration area In chronic glomerulonephritis, the number of functional glomeruli is reduced, the filtration area is reduced. The GFR will reduce. The urine volume will reduce. 2) Increased reabsorption of water and sodium in renal tubules (a) More reabsorption in proximal tubules (increased filtration fraction). GFR (103ml/min)(numerator) Normal FF=-------------------------------------------- = 0.174 RPF (603ml/min)(denominator) When the sympathetic excitability is increased, 75 (54~105) FF=---------------------- = 0.323 190 (19~313) • The contraction of efferent arteriole is greater than the afferent arteriole, so the filtration pressure is relatively increased, then the GFR is relative increased and FF is increased. More filtrate passes through the filtration membrane, the non-filtered blood through the glomeruli is concentrated, which means the higher COP, the lower CHP occur in the blood around the proximal tubules. Hence, the reabsorption of water and sodium is increased. (b) More reabsorption in loop of Henle There are two kinds of nephrons: ①cortical nephron with short loop (in cortex) and less absorption of water and sodium; ② juxtamedullary nephron with long loop and stronger capability of absorption because the loop goes into the hypertonic medullary. • Normally more than 90% of renal blood flow supplies to cortical nephrons, only about 10% of renal blood flow goes to the juxtamedullary nephrons. Under some pathological conditions (increased sympathetic excitability), the cortical artery contracts , large amount of blood flow shifts from cortical nephrons to juxtameddulary nephrons, so the reabsorption of water and sodium is increased. (c) Increased secretion of aldosterone decreased effective circulating volume activation of reninangiotensin system, secretion of aldosterone. increased Na+ reabsorption increased ADH release retention of water and sodium increased [K+] decreased [Na+] in ECF (d) Increased secretion of antidiuretic hormone (ADH) (e) Suppressed activities of prostaglandins (PGs) and kinin system in kidneys Renal medulla produces the PGA2 and PGE2. Renal cortex produces the kallidin 胰 激 肽 and bradykinin. All four media can dilate the renal blood vessels and promote the excretion of water and sodium from kidneys. In chronic renal diseases, the production of PGs and kinins is reduced. 3. Characteristics of edema (1) Properties of edematous fluid -----------------------------------------------------------------------------------------Edematous causes protein appearance specific fluid concentration gravity -----------------------------------------------------------------------------------------transudate ↑effective filtration 1~2g % clear low pressure exudates ↑permeability of vascular wall lymph 4g % muddy high obstruction of 4~5 % chyliform higher lymphatic vessel ----------------------------------------------------------------------------------------- (2) Cardiac edema 1) Manifestation: Cardiac edema is caused by right heart failure. Right heart failure means: (1) the output of right ventricle is reduced, (2) the end-diastolic volume in right ventricle in increased. Total venous pressure is increased. When the patient is ambulant, the legs are firstly involved, the swelling of ankles is often the first sign. Liver engorgement Distention of jugular vein 2) Mechanism of cardiac edema (a)Decreased cardiac output ↓myocardial contraction ↓ volume of blood pumped to the aorta ↓ renal blood supply ↑renin -angiotensin II -aldosterone system ↑reabsorption of sodium ↑ADH release ↑water reabsorption the extracellular volume expanse ↓myocardial contraction ↓ volume of blood pumped to the aorta via baroreceptor ↑ sympathetic excitability ↑ contraction of afferent arteriole increased FF blood redistribution in kidneys ↓glomerular blood flow ↓ filtration pressure ↓ GFR ↑ reabsorption in proximal tubules ↑ reabsorption in loop of Henle (b)Increased venous pressure ↓myocardial contraction of right ventricle ↑hydrostatic pressure of venule ↑effective filtration pressure stagnant hypoxia ↑vascular permeability ↑ formation of edematous fluid (3) Pulmonary edema Pulmonary edema is an abnormal accumulation of fluid in pulmonary interstitial space (interstitial pulmonary edema) and alveoli (alveolar pulmonary edema). Pulmonary edema caused by left heart failure Mechanism: The output of left ventricle is reduced, the end-diastolic volume in left ventricle in increased. Pressure of left atrium is increased. The pulmonary venous pressure is increased. CHP is increased. Effective HP is increased. Effective FP is increased. The formation of interstitial fluid is increased. Pulmonary edema caused by other diseases (a) Increased pulmonary vascular permeability Many irritant gases (chlorine, nitrogen peroxide, ozone) and high concentration of oxygen may damage the alveolarcapillary membrane and increase the permeability of the pulmonary capillaries. (b) Decreased plasma COP The plasma protein is decreased in cirrhosis, nephropathy and severe malnutrition. The COP is decreased. Effective COP is decreased. Effective FP is decreased. The formation of interstitial fluid is increased. Pulmonary edema causes the diffusion disorder of oxygen, hypoxia and dyspnea. (1)What kind of edema can be caused by myocardial infarction of left ventricle? Why? (2)What kind of edema can be caused by right heart failure? Why? (3)What type of edema can be caused by chlorine inhalation? Why? (4)Is edema a bad thing or a good thing? Why? Normal CV Cirrhosis PT (4)肝性腹水 (Hepatic ascites) 正常腹腔内液 50ml 腹腔内液超过 200ml 腹水 1)portal hypertension 2)reduced synthesis of albumin 3) reduced inactivation of ADH and aldosterone 4) reduced effective circulating volume 4. Effects of edema on the body (1) Beneficial effects (2) Harmful effects (1) Beneficial effect 1) Protective effects in inflammatory edema (a) Dilute and neutralize the toxin by the edematous fluid. (b) Promote transportation of antibody and drugs to the inflammatory area due to the increased permeability of vascular wall. (c) Form the fibrin net to prevent bacteria from spreading to the peripheral area. . 2) ‘Safety valve’ of circulatory system When the volume of plasma is rapidly expanded (venous infusion), large amount of fluid may transfer to the interstitial space. It is an important way to regulate the blood volume. (2) Harmful effects 1) Increase the distance between capillary and cells. The supplies of nutrients and oxygen will be reduced. The edematous tissue will be dystrophic. The potential of anti-infection is reduced. The wound will be not easy to heal. 2) Dysfunction of edematous organs and tissue Dysfunction of edematous organs and tissue depends on the rate and extent of development of edema. Edema of vital organs (lungs, brain, larynx) will be dangerous for the life. Laryngeal edema (asphyxia)