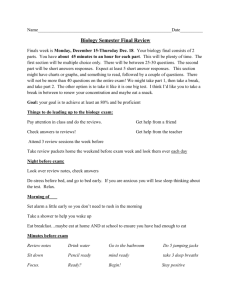
Top 5: waste of antibiotics.
advertisement
ANTIBIOTIC RESISTANCE; WHAT’S TO BE DONE? (TOP 5: WASTE OF ANTIBIOTICS) Dr SG Jones. EUROPEAN ANTIBIOTIC AWARENESS DAY 18 NOVEMBER What is antibiotic resistance? • when bacteria adapt and develop a way to protect themselves from being killed by antibiotics • bacteria are more likely to develop resistance when antibiotics are overused or not used as prescribed Why is it a problem? • infections caused by antibiotic resistant bacteria are more difficult to treat leading to increased levels of disease and death and longer hospital stays • operations like bone, heart or bowel surgery, and treatments like chemotherapy all require antibiotics to be successful; if our antibiotics do not work these procedures will become impossible without risk of infection What can I do? Developed by • become an Antibiotic Guardian by choosing a pledge to undertake a simple action that can help prevent the development and spread of antibiotic resistance YOUR ACTIONS PROTECT ANTIBIOTICS, RALLY TOGETHER AT ANTIBIOTICGUARDIAN.COM What is the problem. • Multiple Antibiotic resistance. • Particularly Gram Negatives: ESBLs CPEs- Carbapenemase producers; very few antibiotic classes left to treat. • Less so with gram positives – MRSA, GISA, VRE. • Poor incentives for industry to develop new classes of antibiotic, very few in pipeline. Increase in E.coli septicaemias by 12% Proportional prescribing: GPs 78% Hospitals 15% Other community prescribers 6% Overall increase by 6% - GP 4%, Hospitals 12%, Other community prescribers 32%. European Antibiotic prescribing data. Antibiotic Stewardship. ‘Right antibiotic, at right time, and for right duration’. Documentation important – on drug chart and patient notes (continuity of care). Allergies, Antibiotic, Indication, Duration, Review date. Review of prescription at 48 -72 hrs. Antibiotic Stewardship. • Does it work in reducing resistance? - Evidence base sparse. • Interactions with bacteria, host, environment and wider community are highly complex and incompletely understood. • All antibiotic use has potential to induce resistance, not just inappropriate use ( 5-20%). 22020%$% 0 Inappropriate Rx. 80% Necessary and justifiable Rx. In no particular order of wastefulness. 1.The chronic ulcer. • Swabbing chronic ulcers /pressure sores is a dangerous game. • Human agar plates – you practically always grow bacteria, sometimes polymicrobial. • What are you going to do with this lab report? Cycle of Antibiotic misuse. District nurse sees pressure ulcer 2 weeks later -no change in ulcers appearance No clinical assessment of pt. Prescribes Antibiotic x Swab is taken Lab reports: bacterial growth No examination of patient GP sees report thinks- ‘must treat’. 2. The phantom pneumonia. • Confusion with exacerbation of COPD/bronchitis, old pulmonary fibrosis, heart failure. • The poor quality Chest Xray, some pulmonary oedema in a generally frail and unwell patient. • Antibiotics started just in case. • Diagnosis not reviewed and patient receives full course of antibiotics for CAP ( usually TAZ +Claritho) 3. Asymptomatic bacteruria in elderly. • Common phenomenon, esp in elderly. • Bacteria (planktonic) enter bladder periodically and transiently – usually flushed away. • Does not constitute a UTI. • Patient does not have key symptoms of: 1. Dysuria. 2. Frequency/ urgency. • These patients should not be tested – dipstick MSU. Urine culture will often grow bacteria and a report will be sent from lab which induces clinician to treat. • These patients should not receive antibiotics. Without dysuria no urine testing and no antibiotic treatment 4. The colonised urinary catheter. • CSU taken lab results( WBC, bacteria cultured) patient treated with antibiotics. • In time, most urinary catheters become colonised with bacteria. • Long term catheters often develop biofilm. • Lower UTI in catheterised patient does not make sense as a pathophysiological concept Urinary catheter biofilm formation. 5.Stasis dermatits – chronic cellulitis • No such thing as chronic cellulitis. • Chronic skin changes on top of chronically oedematous legs; sometimes ulcerate. • Often bilateral – cellulitis very rarely erupts in two places simultaneously • Multiple courses of antibiotics given, over several months/years, with little response. Stasis dermatitis / venous stasis ulceration. Over-reliance on inflammatory markers • Indicators of inflammation not specifically infection. • Not as responsive as we think – especially on downward trend. • Should not be used as lone indicators – need to be tied in with clinical signs of infection. • Treat the patient and not just the numbers. Some wider concerns. • Antibiotics used for non infection indications: as prokinetics, anti-encephalopathy, control of pruritus in cholestasis. • Long term prophylaxis: recurrent urinary tract infections COPD/Bronchiectasis, SBP. • Over extension of peri-operative prophylaxis from 1-2 doses extended to 2-4 days. Extension of prescribing rights to non medical HCWs. • Everyone wants to be an independent prescriber. • Proliferation of PGDs, driven by cost and medical availability. Evidence of poor oversight and lack of audit. • Specialist nurses in community e.g. COPD nurses, ulcer specialists. • Over the counter medicine creep. Psychology of prescribing – who can say no? • 1940s to 1980s: Paternalistic view of medicine – ‘doctor knows best’. • 1990s to 2000s: Patients charter – government as protector and promise of good care – • 2000s to present day: ‘Patient experts’, ‘partnership medicine’, ‘internet self diagnosis’• Patient satisfaction surveys – net promoters/detractors etc. Cycle of global factors influencing generation of antibiotic resistance. Developed world. Lack of effective antibiotics. Greater sophistication of modern medicine – increased age and fragility of patients, more immunocompromised, ever more invasive techniques. Developing world. Poor national healthcare systems Unlicensed / criminal pharmaceutical production – ‘fake’ antibiotic market. Spread of multi-resistant bacteria in hospitals / community (UK, Europe, USA etc) – increased use of broader spectrum antibiotics. Inadequate national and international surveillance systems both in scope and sophistication. Global movement of resistant organisms and resistance genes Low incentive for pharmaceutical companies to innovate and develop new antibiotic molecules. Inadequate state regulation of prescribed drugs. Inadequate local enforcement. Poor provision of primary medical care. Lack of microbiology laboratory facilities at local /national level. Over the counter purchase of antibiotics: pharmacies, corner shops, street markets. High burden of infective diseases, poor sanitation, poor standard of dwellings. Increased international travel / migration. Globalisation, human trafficking. Mass worldwide use of antibiotics as growth promoters in livestock. Poverty, inadequate access to basic healthcare – need to pay for access. SGJ. Nov 2013. Global issues. • Unregulated antibiotic market – corner shop, open air • • • • markets, large drug stores. Extensive, and growing, illegal/ fake antibiotic industry. Doctors contracted/ induced to prescribe certain pharmaceuticals ( Japan). Expansion of global air travel. Inadequate microbial/ Ab resistance screening infrastructure. Fake pharmaceuticals. Facilities range from crude to hi tech. £18 billion industry (WHO 2011) accounting for 10% of all pharmaceutical sales worldwide. Bottom left- raid on warehouse East midlands 2010. Unregulated pharmaceutical market. Movement of bacteria and viruses around the globe. So what’s being done. Recognition – WHO, EU, Infectious disease soc of America, UK Gov, World Economic Forum. Longitude Prize £10M – universal infection detector. US Gov. Barack Obama has directed NSC to develop a national action plan. Partnership. • Public private partnership: Bill and Melinda Gates Foundation –accelerated anti TB drug programme. • EU Federation of Pharmaceutical Industries –antibiotic discovery programme. • Return of several smaller pharma companies into market – money to be made. Decoupling reward from sales. • Need to understand that antibiotics are a world asset. • Drug company may spend £xbillion and 15 years of development to bring a new antibiotic to market. • Then may be used for only 100 patients /year. • Health care systems need to pay for innovation not units sold. Prioritisation and conservation. • Global charter. • Access through health care systems. • Conservation through clinical prioritisation tailored to diagnosis. • Most antibiotic tonnage used as growth promoters in animal feed – need worldwide treaty. Thank you - Any Questions?