Oklahoma State PABI Plan Meeting
advertisement
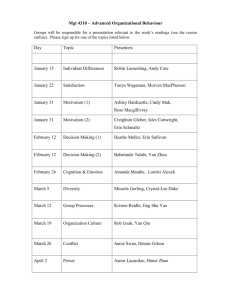
OKLAHOMA’S PABI PLAN OK.THEBRAINPROJECT.ORG: REINTEGRATION AND LONG-TERM CARE COMMITTEE JUNE 29, 2013 MEETING @ INTEGRIS JIM THORPE, OKC Our work: The Reintegration/Long-term Care Category focuses on the child/young adult with PABI from the time of referral from acute care, rehabilitation, or community agency to his/her transition to adulthood. This phase includes the process of reintegrating children and youth with PABI back into their homes, schools, and communities and ensuring that they and their families get the services needed to maximize their child’s potential following brain injury. The Reintegration/Long-term Care Category is designed to include a comprehensive and coordinated system of identification and service provision involving: Child/family services Policy development and education for hospital personnel Standard of care programs that explicitly link hospital experts with communitybased, school and medical personnel before the child/young adult is discharged from the hospital Capacity building for schools and other community agencies Integration of research and practice. The model includes four components: identification, assessment, tracking, and advocacy/support. Our guiding principles: 1. Children with brain injury should be raised in their homes with adequate support. This allows parents to remain parents above medical caretakers and all children in the home to develop into adults with their own pursuits and gifts. 2. Our committee work focuses on the family’s support in tandem with the child’s reintegration. Appropriate case management reflects whole family support and not just the child’s rehabilitation from brain injury. 3. Compassion, guidance and empowerment should begin at BI diagnosis and be present across all sectors of family support. “There is no systematic method for connecting children and their families with services within the school and community following a brain injury. Schools, families and communities are the real long-term providers of services -- not hospitals. “ Families need consistent support and pathways to resources. Committee Members as of June 2013 * indicates person is a self-advocate or has a family member with PABI Chairs: Erin Taylor *, Oklahoma Developmental Disabilities Council and the Malley & Henry Fund. Erin.Taylor@okddc.ok.gov www.OKDDC.ok.gov or www.MalleyandHenryFund.org Jennifer Lockhart *, Sooner SUCCESS Director at the OU Health Sciences Center. Jennifer-Lockhart@ouhsc.edu http://soonersuccess.ouhsc.edu/ Mirka Bullock *, parent & caregiver Mirka10208@gmail.com Lisa DeBolt *, Sooner SUCCESS, Tulsa County Lisa-DeBolt@OUHSC.edu http://soonersuccess.ouhsc.edu/ Karalee Hopkins *, RN, parent & caregiver Khopkins98@yahoo.com Sarah Kupiec, Preferred Pediatric Home Health Care Sbk1212@sbcglobal.net www.preferredhomehealthcare.com/ Tammy Lawson, OK State Dept of Education: Special Education Services Tammy.Lawson@sde.ok.gov http://www.ok.gov/sde/special-education Beth Stigler, Preferred Pediatric Home Health Care bstigler@preferredpediatric.com www.preferredhomehealthcare.com/ Sharon Vaz, OK State Dept of Health, Screening and Special Services sharonav@okhealth.ok.gov http://www.ok.gov/health/index.html Susan Wegrzynski, OK State Dept of Health, Screening and Special Services susanmw@health.ok.gov http://www.ok.gov/health/index.html If you would like to contribute or participate in this committee, please email Erin at: Erin.taylor@okddc.ok.gov TBI is not the only form of pediatric brain injury. Think also of: Genetic conditions, brain cancers and degenerative brain disease Fetal alcohol spectrum and other drug-related brain injuries Hypoxic and anoxic brain injuries Seizure disorders Cerebral palsy and perinatal injuries Lead poisoning and other environmental factors A growing list of people and agencies we need to include AND learn more from: Please add to this list by emailing Erin Self-Advocates (incurred BI before age of 25) School and child care professionals as well as higher ed and career techs OK Health Care Authority TEFRA, nurse case managers Dept of Human Services DDSD, Family Support Services, respite waivers Pediatricians, developmental pediatricians and peds neuropsychiatry OK Infant Transition Program and NICU specialists Long-term pediatric care facilities OK Commission on Children and Youth OK Family Network Social agencies such as the YMCA, Special Olympics, youth groups and Girl Scouts Attorneys versed in guardianship, SSI, MPA, etc. Attorneys and social workers versed in child abuse matters Educators from the mental health advocacy community Indian Health Services Observations from Committee Members @ June meeting: 1. In OK, there is a considerable disconnect between medical care for the child with BI and community supports. 2. New and established teachers (special ed and others) have little opportunity (notably learning time) to receive training about BI. 3. Other disability advocacy communities (autism, Down Syndrome, etc) can teach us a great deal on community outreach and advocacy. 4. Family members may be hesitant to share their stories and seek support because it is the “emotional return” to that moment when the BI occurred. As such, we must recognize that some families may have grief counseling needs. 5. The effects of a BI may take years to manifest and families may not connect schooling struggles and behavior/communication/socializing issues to the BI. 6. At the Brain+CHILD conference, despite an intensive, statewide marketing campaign, we did not have many attendees – notably teachers, coaches, medical professionals, DHS, BI prevention and support groups as well as state government leadership. 7. Parent-to-parent mentoring should take into consideration age of child, region and type of BI. Committee Assignments for July 30 meeting (Jennifer to arrange): • Tammy find out which diagnosis categories a BI can fall under on an IEP. • Tammy determine how much time special education students receive instruction on brain injury. • Susan determine what Sooner Start employees likely know about BI • Susan/Sharon provide materials on lead poisoning and BI to committee • Erin get information about Dr. Kristin King at the U.Tenn Knoxville • Jennifer put us in touch with Ed Long and Paul Darden • Jennifer follow up on the professor in KS – name? • Karalee approach a rural pediatrician for insight on their needs • Erin contact one of the BRAIN+Child attorneys to provide some insight • Erin ask Stan about utilizing ONE Net access for videoconferencing • ALL: Provide family friendly internet-based resources to embed @ DIG: Disability Information Gateway to be hosted by the OK Developmental Disabilities Council • Jennifer approach CHF about medical personnel needs relating to BI. Make a presentation? • Erin ask that PABI be part of the Governor's Blue Ribbon Commission on Developmental Disabilities. • Before 2013 session starts, Erin will write an overview letter to state legislators K Walker, T Ivester, J Enns, J Echols, K Henke and D Cox…who else? • ALL speak to at least two people in their community who may be an asset to our work. Ongoing Questions –begin assigning in July?: Leaving the Hospital What does the recovery path typically look like and where are there gaps in providers and family support? Children with BI leaving the hospital or long-term care facilities may still need specialized medical care. How can we align the medical home model with OK-PABI? To learn more about the medical home model, see slide 16. As a family leaves their hospital/acute care setting, which resources should they immediately have access to? • Who can help them navigate this? • “Several factors may account for the failure to link children and families to community services following PABI. For example, the standardized assessments commonly used in hospitals and rehabilitation facilities are of questionable validity in predicting the child/young adult’s needs in returning to school and home.” (p. 72 http://thebrainproject.org/pabihome.php). The PABI Virtual Center will connect families to BI supports in the community (to occur as close to diagnosis as possible). What will these supports be? In cases of PABI, there are “down the road” medical conditions to consider and of which families need education: Post-Acute Medical Considerations: • Endocrine issues • Mental health • Poor growth/Failure to thrive • Disorders of consciousness (DOC) including those in coma, MCS (minimally conscious state) and VS (vegetative state) Thriving in Home, School & Community For a child with PABI, transitions from hospital to home/school/community tend to be fragmented and uncoordinated with little communication among families and hospital, school, and agency personnel. • What factors inhibit these communication pathways? How can we improve this? • Few measures have been developed to examine outcomes of these important transitions. What can we learn from family supports such as Person-Centered Planning/Families Planning Together (contact Jenifer Randle at the OK Developmental Disabilities Council: jenifer.randle@okddc.ok.gov or 405.521.4964). Where do families coping with BI go for family-to-family support now? Where are our caregiver support groups? Do they offer respite and child care? Where can we keep a list of these groups? Some brain injuries may have a delayed impact in the child’s life. How do we prepare families and educators? What are successful models? How do respite programs work with families who have a child with a BI? Educating our Community How do we wrap research and education around our Reintegration Committee work? • What research is lacking in our state? What do families need to know about coping with PABI? What do educators need to know about PABI? What do legislators and state agency leadership need to know about PABI? What do pediatricians need to know about PABI? Pediatric specialists? Others? How do we educate on different types of PABI? Learning from Others What states have a BI waiver and what can we learn from them? What can we learn from veterans? What can we learn from other states in how they hire and keep BI medical personnel? How can we best support families in rural settings? Limited English proficiency? Families already in crisis before the BI? As the child moves toward adulthood, how can we teach self-care and self-awareness issues appropriate for their needs? Personal/bodily safety, ability to convey important information, sexuality, social interactions, healthcare decisions, what else? What are the BI personnel shortages in our state and in distinct regions? Can we create a map of PABI medical expertise and allied health providers? In June, we briefly discussed how we could evaluate current BI programs meeting family needs. This 5A Model may be helpful: AVAILABLE: Our services are at the disposal of every family in the communities in which we serve. Supports are currently operational and families do not need to wait extended periods. Staff is trained and timely in meeting families’ requests. ACCESSIBLE: Families can access our program – both in terms of geography and hours of operation. Our websites are consumer-friendly including functional literacy and ADA compliance. Our intake staff (over the phone and in person) knows how to appropriately route requests. We can manage non-English speakers’ requests. Our programs are physically accessible to those with special mobility and communication needs. AFFORDABLE: Our programs operate not solely on a poverty formula threshold. Families who are financially able to support most of their children’s needs are not prohibited from accessing our services. Our programs do not require people take extended time from work to access them. Our programs can reimburse families for travel costs and child/respite care. APPROACHABLE: Our leadership models and expects all staff to practice welcoming and inclusion. This means we always remember that consumers may be missing some fundamental information about how our program works or more appropriate resources. We are friendly and respectful to those who come with requests. As an agency or organization, our mission statement, training and policies address appropriate interaction with consumers. We support one another as staff so that our colleagues do not become overwhelmed by their work. We demonstrate an eagerness to help and accurately refer families to better suited resources when necessary. APPROPRIATE: Our program needs the expressed needs of families. We regularly take opportunities to listen to families. We value person-centered/family-centered program development vs. a “menu of options” service delivery. We employ qualified persons who have lived experience in the issue upon which we work. We are always willing to look at ourselves as an agency or organization and implement improvements. Medical Home Model from: http://www.pcpcc.net/about/medical-home The medical home is best described as a model or philosophy of primary care that is patient-centered, comprehensive, team-based, coordinated, accessible, and focused on quality and safety. It has become a widely accepted model for how primary care should be organized and delivered throughout the health care system. While the term 'home' can often leave room for misinterpretation or confusion, we often emphasize that the "medical home" is not a place, but a philosophy of health and health care that encourages us to meet patients where they are, from the most simple to the most complex conditions. It is a place that should "feel like home" - where you are treated with respect, dignity, and compassion, and you have a strong and trusting relationship with providers and staff. It calls for a team care model that promotes accessibility, compassion, transparency, and is built on trust and communication. Its success is enhanced by health information technology and incentivized by smarter ways to pay for care. Above all: the medical home is not a final destination. It is a framework for achieving primary care excellence so that care is received in the right place, at the right time, and the manner that best suits a patient's needs. The medical home is an approach to the delivery of primary care that is: Patient-centered: A partnership among practitioners, patients, and their families ensures that decisions respect patients’ wants, needs, and preferences, and that patients have the education and support they need to make decisions and participate in their own care. Comprehensive: A team of care providers is wholly accountable for a patient’s physical and mental health care needs, including prevention and wellness, acute care, and chronic care. Coordinated: Care is organized across all elements of the broader health care system, including specialty care, hospitals, home health care, community services and supports. Accessible: Patients are able to access services with shorter waiting times, "after hours" care, 24/7 electronic or telephone access, and strong communication through health IT innovations. Committed to quality and safety: Clinicians and staff enhance quality improvement through the use of health IT and other tools to ensure that patients and families make informed decisions about their health. Thank you to our outstanding committee members! We will speak on July 30th ~ please have completed some work on your assignments (see slide 9). This presentation will be loaded up at ok.thebrainproject.org where you will have access to the slide show from the Sarah Jane Brain Project made by Patrick Donohue. Please share these resources in your community. For questions about OK PABI’s plan, please contact Dr. Stanley Grogg at: Stanley.Grogg@okstate.edu. For questions about the national PABI, please contact Ted Molloy at: ted@thebrainproject.org. You can reach Erin at 405.226.0790 (cell/text) or at my office 405.521.4967. Erin.Taylor@okddc.ok.gov.