C. roseus
advertisement

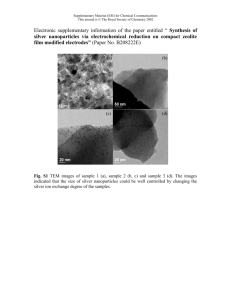
Cytotoxicity of Silver Nanoparticles Synthesized by Catharanthus roseus Aqueous Extract on Jurkat and HT29 Cancer Cell Lines Nor Hazwani Ahmad, PhD Nanotechnology Congress & Expo August 11-13, 2015 Frankfurt, Germany Research background 2008-2012 2013-now Effects of Catharanthus roseus Aqueous Extract on Jurkat Cells and Normal Peripheral Blood Mononuclear Cells Biosynthesis and Characterization of Silver Nanoparticles Using Catharanthus roseus Plant Extracts and Analysis of Cytotoxic Activities Supervisor: Prof. Ishak Mat Co-supervisor: Assoc. Prof. Mustaffa Fadzil Farid Wajidi Siti Zulaikha Ghozali Postgraduate stu dent (Master of Science (Medical Research)) Ira Maya Sophia Undergraduate stu (Bachelor of Science (Biology)) Nur Jalilahtul Mahfuzah Postgraduate stu dent (Master of Science (Medical Research)) Gene expression profiling of C. roseus-treated Jurkat cells The mechanism of apoptosis regulated by genes in C.roseus-treated Jurkat cells. Adapted from “The role of the Bcl-2 protein family in cancer” by L. Coultas and A. Strasser, 2003. Seminars in Cancer Biology, 13, p. 116. = Pro-apoptosis genes = Inhibition = Activation = Upregulated genes = Downregulated genes Gene expression profiling of C. roseus-treated Jurkat cells The differentially expressed genes associated with the progression of cell cycle induced by C.roseus extract in Jurkat cells. Adapted from “The molecular biology of head and neck cancer” by C. R. Leemans, B. J. M. Braakhuis and R. H. Brakenhoff, 2011, Nature Reviews in Cancer, 11, p. 12. = S-phase arrest-induced genes = Upregulated genes = Downregulated genes Introduction Detection, target & treatment of CA [1] Nanoscale Tx is advantageous [2, 3] Nano oncology Overcome limitation of conventional CA therapy [4] NP-derived drugs in different phase of clinical development [5] Silver nanoparticles (AgNPs) • • • Definition: nanoscale metals sized within 1 to 100 nm [6] Unique properties: good in conductivity, stability, catalytic & antibacterial [7] Biomedical application: anti-inflammatory, antioxidant, antimicrobial, medical devices [8,9 • However, potential application as anticancer agents are still new and remain to be investigated ] • Biocompatible to healthy cells and has inhibitory effects on various human CA cell lines: glioblastoma cells [10], Dalton’s lymphoma ascites [11], cervical carcinoma [12], breast carcinoma MCF-7 cells [13], HeLa cells [14], lung cancer A549 cells [15]. • Method of synthesis • Physical (thermal and laser ablation, sputtering, milling) [16] • Chemical (sodium borohydride, potassium bitartrate, methoxypolyethelene glycol, hydrazine). Hazardous Substance Fact Sheet: sodium borohydride cause irritation and burn, shortness of breath etc [17] • Biological (Plants, microorganism) [18] Problem statement 1: Limitation of conventional anticancer therapy Problem statement 2: Hazardous chemicals used for AgNPs synthesis Main objective To evaluate the anticancer activity of C. roseus-AgNPs on Jurkat and HT29 cells Specific objectives 1) To examine the effects of C. roseus-AgNPs on the proliferation of Jurkat and HT29 cells 2) To evaluate early detection of apoptosis in Jurkat and HT29 cells treated with C. roseus-AgNPs 3) To analyze the cell cycle of Jurkat and HT29 cells treated with C. roseus-AgNPs Methodology Preparation Characterization of C. roseus -AgNPs Preparation of cell lines C. roseus-AgNPs Surface plasmon nm 10% of C. roseus aqueous extract in 5 mM of AgNO500 3 (uv-vis spectroscopy) Transmission electron microscopy (TEM) MTS X-ray diffraction (XRD) Concentrations: 1.96 to 1000 µg/ml (double dilution manner) Incubation times: 24, 48 and 72 h ELISA microplate reader Jurkat cells (4 × 105 cells/ml) HT29 cells (1 × 105 cells/ml) Shape: Spherical & uniform Size: 20 to 50 nm Annexin-FITC/PI Cell cycle Average of diameter: 30 nm Spectrum 2θ values: 38.12°, 44.31, 64.45 & Concentration: 10 µg/ml Concentrations: 77.41 5, 10, 15 µg/ml111, 200, 220 & 311 Plane: Incubation times: 24, 48 Structure: Crystals in nature and 72 h Incubation times: 6, 24, 48 and 72 h FACS Calibur flow cytometer (Cell Quest Pro software) Statistical analysis One-way ANOVA, post-hoc Tukey’s test Significance: p < 0.05 FACS Calibur flow cytometer (Cell Quest Pro & ModFit softwares) Results and Discussion Proliferative effects of C. roseus-AgNPs on Jurkat cells Median IC50 value: 5.87 µg/ml Figure 1: Proliferative effects were evaluated by MTS assay. Jurkat cells were treated with C. roseus-AgNPs at double dilution manner. Untreated cells were used as negative control while camptothecin was used as positive control. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Proliferative effects of C. roseus aqueous extract on Jurkat cells Median IC50 value: 361.72 µg/ml Figure 2: Proliferative effects were evaluated by MTS assay. Jurkat cells were treated with C. roseus aqueous extract at double dilution manner. Untreated cells were used as negative control while camptothecin was used as positive control. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Proliferative effects of C. roseus-AgNPs on HT29 cells Median IC50 value: 13.19 µg/ml Figure 3: Proliferative effects were evaluated by MTS assay. HT29 cells were treated with C. roseus-AgNPs at double dilution manner. Untreated cells were used as negative control while camptothecin was used as positive control. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Proliferative effects of C. roseus aqueous extract on HT29 cells Median IC50 value: 419.26 µg/ml Figure 4: Proliferative effects were evaluated by MTS assay. HT29 cells were treated with C. roseus aqueous at double dilution manner. Untreated cells were used as negative control while camptothecin was used as positive control. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. • C. roseus-AgNPs on Jurkat cells C. roseus-AgNPs on HT29 cells C. roseus aqueous extract on Jurkat cells C. roseus aqueous extract on HT29 cells Med: 5.87 µg/ml Med: 13.19 µg/ml Med: 361.72 µg/ml Med: 419.26 µg/ml C. roseus-AgNPs produced higher cytotoxicity effects than C. roseus aqueous extract • Different phytochemicals responsible in the AgNP synthesis have contributed to the cytotoxic effects on cells (fatty acids, esters & alkaloids) [19] • Unique features of AgNPs (small size, high surface area to volume ratio, surface functionalization) biokinetics of AgNPs & increase cytotoxicity [20] • Higher number of AgNPs were observed in mouse fibroblasts compared to silver microparticles induce ROS DNA damage apoptosis [21] • Jurkat cells were more sensitive than HT29 cells, either in response to C. roseus-AgNPs or C. roseus aqueous extract • Anticancer vinca alkaloids present in C. roseus are commercial anticancer chemotherapeutic drugs to combat acute lymphoblastic leukemia [20, 22] • Other possible anticancer alkaloids include vindesine, vinepedine and vinsrosidine antitubulin properties inhibit formation of mitotic spindles by damaging microtubules cell cycle arrest [23] C. roseus-AgNPs on Jurkat cells Induction: 1.96 µg/ml (72 h) • C. roseus-AgNPs on HT29 cells Induction: 3.91 & 7.82 µg/ml (48 h), 1.96 & 3.91 µg/ml (72 h) C. roseus aqueous extract on Jurkat cells C. roseus aqueous extract on HT29 cells No induction of cell proliferation No induction of cell proliferation Induction of cell proliferation at low concentrations of C. roseus-AgNPs on Jurkat and HT29 cells • Differential effects may occur where high dose increases cytotoxicity while low dose induces cell proliferation. Hormesis = potentially toxic agents cause stimulation in lower doses [24] • Crude plant extract used in AgNPs synthesis contains numerous active compounds that interacting to one another [24] • Apart from anticancer compounds, non-enzymatic antioxidant molecules (ascorbic acid, αtocopherol, reduced glutathione and antioxidation enzymes) scavenge the ROS [25] Expression of externalized phosphatidylserine on Jurkat cells treated with C. roseus-AgNPs Figure 5: Histograms of the detection of phosphatidylserine by annexin V-FITC/PI staining. Quantitative percentages of viable cells (Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Expression of externalized phosphatidylserine on Jurkat cells treated with C. roseus aqueous extract Figure 6: Histograms represent quantitative percentages of viable cells (annexin-/PI-), early apoptotic cells (annexin+/PI-), late apoptotic cells (annexin+/PI+) and necrotic cells (annexin-/PI+). Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Expression of externalized phosphatidylserine on HT29 cells treated with C. roseus-AgNPs * * Figure 7: Histograms represent quantitative percentages of viable cells (annexin-/PI-), early apoptotic cells (annexin+/PI-), late apoptotic cells (annexin+/PI+) and necrotic cells (annexin-/PI+). Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Expression of externalized phosphatidylserine on HT29 cells treated with C. roseus aqueous extract Figure 8: Histograms represent quantitative percentages of viable cells (annexin-/PI-), early apoptotic cells (annexin+/PI-), late apoptotic cells (annexin+/PI+) and necrotic cells (annexin-/PI+). Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. • At 6 h, C. roseus aqueous extract produced higher percentages of early apoptotic cells while C. roseus-AgNPs produced higher percentages of late apoptotic cells • Indicates that C. roseus aqueous extract started to induce apoptosis after 6 h and C. roseus-AgNPs induced apoptosis earlier than 6 h C. roseus-AgNPs on Jurkat cells • C. roseus aqueous extract on Jurkat cells C. roseus aqueous extract on HT29 cells At 24 h, total percentages of early and late apoptotic cells for each treatment correlate with MTS assay C. roseus-AgNPs on Jurkat cells • C. roseus-AgNPs on HT29 cells C. roseus aqueous extract on Jurkat cells C. roseus-AgNPs on HT29 cells C. roseus aqueous extract on HT29 cells At 48 and 72 h, total percentages of early and late apoptotic cells of HT29 treated by C. roseus-AgNPs were higher compared to aqueous extract • MTS assay - Induction of cell proliferation was observed at low concentrations, 3.91 & 7.82µg/ml (48 h) and 1.96 and 3.91 µg/ml (72 h) • These concentrations are within the ranges of concentrations used for annexin/PI staining Effects of C. roseus-AgNPs and C. roseus aqueous extract on the cell cycle of Jurkat cells Figure 9: Histograms of cell cycle of Jurkat cells that indicate percentages of cells in G0/G1, S, and G2/M phases. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. Effects of C. roseus-AgNPs and C. roseus aqueous extract on the cell cycle of HT29 cells Figure 10: Histograms of cell cycle of HT29 cells that indicate percentages of cells in G0/G1, S, and G2/M phases. Each value was expressed as mean ± SD of three replicates. * indicates significant differences (p < o.o5) with respect to untreated group. • C. roseus-AgNPs on Jurkat cells C. roseus-AgNPs on HT29 cells C. roseus aqueous extract on Jurkat cells C. roseus aqueous extract on HT29 cells Arrest: S-phase (all incubations) Arrest: G0/G1 phase (24, 48h), S phase(72h) Arrest: S-phase (all incubations) Arrest: G0/G1 phase (24h), S phase(48, 72h) The DNA damage may arrest or suspend the cells in either G1, S or G2 before undergoing apoptosis, in case the damage cannot be fixed [26] • Oxidative stress activates p38 MAPK & inflammation of the transcription factors [27] • Affect mitochondrial dependent jun-N terminal kinase pathway disruption of mitochondrial respiratory chain increase ROS & interferes ATP synthesis damage cellular DNA [26] • Phytochemicals in C. roseus plant responsible for the cell cycle arrest • Vinca alkaloids have anti-tubulin properties disrupt and interfere microtubules M-phase arrest [28] • Vincristine G2/M phase arrest [29] • Arrest was due to other active compounds in C. roseus • • Camptothecin arrested S and G2/M phases [30, 31] AgNO3 arrested G0/G1 phase (48, 72 h) in HT29 cells • Requires further investigation since it did not inhibit the proliferative activity Conclusion Proliferative activity • Induction of apoptosis Cell cycle arrest Jurkat and HT29 cells have undergone AgNPs-induced stress • Further analysis on the detailed mechanism of cytotoxicity and cellular uptake for better understanding on the cellular interaction • Major drawback associated with new drug development include lack of specificity and uncertainty with its cytotoxicity on normal cells should be further evaluated • In vivo studies are necessary to address the formulation of biogenic AgNPs as an alternative to conventional anticancer drugs • Experimental evidence indicating C. roseus-AgNPs have been shown to induce higher cytotoxic effects compared to C. roseus aqueous extract • Small-sized AgNPs have increased its effectiveness to penetrate cells cell death • Expand the knowledge on the comparison cytotoxic effects between C. roseus-AgNPs and C. roseus aqueous extract on Jurkat and HT29 cells • Foundation to develop better strategy of cancer therapeutic agents References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. ANTHONY, J. J., SITHIKA, M. A. A., JOSEPH, T. A., SURIYAKALAA, U., SANKARGANESH, A., SIVA, D., KALAISELVI, S. & ACHIRAMAN, S. 2013. In vivo antitumor activity of biosynthesized silver nanoparticles using Ficus religiosa as a nanofactory in DAL induced mice model. Colloids and Surfaces B: Biointerfaces, 108, 185-190. AHAMED, M., ALSALHI, M. S. & SIDDIQUI, M. K. J. 2010. Silver nanoparticle applications and human health. Clinica Chimica Acta, 411, 1841-1848. SINGH, R. & JR., J. W. L. 2009. Nanoparticles-based targeted drug delivery. Experimental and Molecular Pathology, 86, 215-223. SATAPATHY, S. R., MOHAPATRA, P., PREET, R., DAS, D., SARKAR, B., CHOUDHURI, T., WYATT, M. D. & KUNDU, C. N. 2013. Silver-based nanoparticles induce apoptosis in human colon cancer cells mediated through p53. Nanomedicine, 8, 1307-1322. BHATTACHRYYA, S., KUDGUS, R. A., BHATTACHRYYA, R. & MUKHERJEE, P. 2011. Inorganic nanoparticles in cancer therapy. Pharmaceutical Research, 28, 237-259. PRABHU, S. & POULOSE, E. K. 2012. Silver nanoparticles: mechaanism of antimicrobial action, synthesis, medical applicatios, and toxicity effects. International Nano Letters, 2. JEYARAJ, M., SATHISKUMAR, G., SIVANANDHAN, G., MUBARAKALI, D., RAJESH, M., ARUN, R., KAPILDEV, G., MANICKAVASAGAM, M., THAJUDDIN, N., PREMKUMAR, K. & GANAPATHI, A. 2013. Biogenic silver nanoparticles for cancer treatment: An experimental report. Colloids and Surfaces B: Biointerfaces, 106, 86-92. SARANYAADEVI, K., SUBHA, V., RAVINDRAN, R. S. E. & RENGANATHAN, S. 2014. Green synthesis and characterization of silver nanoparticle using leaf extract of Capparis zeylanica. Asian Journal of Pharmaceutical and Clinical Research, 7. GURUNATHAN, S., RAMAN, J., MALEK, S. N. A., JOHN, P. A. & VIKINESWARY, S. 2013b. Green synthesis of silver nanoparticles using Ganoderma neo-japonicum Imazeki: a potential cytotoxic agent against breast cancer cells. International Journal of Nanomedicine, 8, 4399-4413. RANI, P. V. A., HANDE, M. P. & VALIYAVEETTIL, S. 2009. Anti proliferative activity of silver nanoparticles. BMC Cell Biology, 10. SRIRAM, M. I., KANTH, S. B. M., KALISHWARALAL, K. & GURUNATHAN, S. 2010. Antitumor activity of silver nanoparticles in Dalton's lymphoma ascites tumor model. International Journal of Medicine, 5, 753-762. VASANTH, K., ILANGO, K., KUMAR, R. M., AGRAWAL, A. & DUBEY, G. P. 2014. Anticancer activity of Moringa oleifera mediated silver nanoparticles on human cervical carcinoma cells by apoptosis induction. Colloids and Surfaces B: Biointerfaces, 117, 354-359. YEHIA, R. S. & AL-SHEIKH, H. 2014. Biosynthesis and characterization of silver nanoparticles produced by Pleurotus ostreatus and their anticandidal and anticancer activities. World J Microbiol Biotechnol, 30, 2797-2803. MANIVASAGAN, P., VENKATESAN, J., SENTHILKUMAR, K., SIVAKUMAR, K. & KIM, S.-K. 2013. Biosynthesis, antimicrobial and cytotoxic effect of silver nanoparticle using a novel Nocardiopsis sp. MBRC-1. BioMed Research International. SANKAR, R., KARTHIK, A., PRABU, A., KARTHIK, S., SHIVASHANGARI, K. S. & RAVIKUMAR, V. 2013. Origanum vulgare mediated biosynthesis of silver nanoparticles for its antibacterial and anticancer activity. Colloids and Surfaces B: Biointerfaces, 108, 80-84. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. MITTAL, A. K., CHISTI, Y., BANARJEE, U. C. 2013. Synthesis of metallic nanoparticles using plant extracts. Biotechnology Advances. 31: 346-356. DURAI, P., CHINNASAMY, A., GAJENDRAN, B., RAMAR, M., PAPPU, S., KASIVELU, G. & THIRUNAVUKKARASU, A. 2014. Synthesis and characterization of silver nanoparticles using crystal compound of sodium para-hydroxybenzoate tetrahydrate isolated from Vitex negundo. L leaves and its apoptotic effect on human colon cancer cell lines. European Journal of Medicinal Chemistry, 84. SULAIMAN, G. M., MOHAMMED, W. H., MARZOOG, T. R., AL-AMIERY, A. A. A., KADHUM, A. K. H. & MOHAMAD, A. B. 2013. Green synthesis, antimicrobial and cytotoxic effects of silver nanoparticles using Eucalyptus chapmaniana leaves extract. Asian Pacific Journal of Tropical Biomedicine, 3, 58-63. SOTTOMAYOR, M., CARDOSO, I. L., PEREIRA, L. & BARCELÓ, A. R. 2004. Peroxidase and the biosynthesis of terpenoid indole alkaloids in the medicinal plant Catharanthus roseus (L.) G. Don. Phytochemistry Reviews, 3, 159-171. ASHARANI, P., LOW KAH MUN, G., HANDE, M. P. & VALIYAVEETTIL, S. 2008a. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS nano, 3, 279-290. WEI, L., TANG, J., ZHANG, Z., CHEN, Y., ZHOU, G. & XI, T. 2010. Investigation of the cytotoxicity mechanism of silver nanoparticles in vitro. Biomedical Materials, 5, 044103. DANIELLE, M., PARESH, C. R. & YU, H. 2014. Molecular Toxicity Mechanism of Nanosilver. Journal of Food and Drug Analysis, 22, 116-127. CHUN-HUA WANG, GUO-CAI WANG, YIN WANG, XIAO-QI ZHANG, XIAO-JUN HUANG, DONG-MEI ZHANG, MIN-FENG CHEN & WEN-CAI YE 2012. Cytotoxic dimeric indole alkaloids from Catharantus roseus. Fitoterapia, 83, 765-769. ASMAH, R., ZETI NADIA, M. Z., ABDAH, M. A. & FADZELLY, A. B. M. 2005. Effects of Catharanthus roseus, Kalanchoe laciniata and Piper longum Extracts on the Proliferation of Hormone-dependent Breast Cancer (MCF-7) and Colon Cancer (Cac02) Cell Lines. Malaysian Journal of Medicine and Health Sciences, 1, 105-110. NEJAT, N., VALDIANI, A., CAHILL, D., TAN, Y.-H., MAZIAH, M. & ABIRI, R. 2015. Ornamental Exterior versus Therapeutic Interior of Madagascar Periwinkle (Catharanthus roseus): The Two Faces of a Versatile Herb. The Scientific World Journal, 2015, 982412. ASHARANI, P. V., LOW KAH MUN, G., HANDE, M. P. & VALIYAVEETTIL, S. 2008b. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS nano, 3, 279-290. EOM, H.-J. & CHOI, J. 2010. p38 MAPK Activation, DNA Damage, Cell Cycle Arrest and Apoptosis As Mechanisms of Toxicity of Silver Nanoparticles in Jurkat T Cells. Environmental Science & Technology, 44, 8337-8342. SHEN, Y., LIU, Q., SUN, H., LI, X., WANG, N. & GUO, H. 2013. Protective effect of augmenter of liver regeneration on vincristine-induced cell death in Jurkat T leukemia cells. International Immunopharmacology, 17, 162-167. SHAO, R. G., CAO, C. X., NIEVES-NEIRA, W., DIMANCHE-BOITREL, M. T., SOLARY, E. & POMMIER, Y. 2001. Activation of the Fas pathway independently of Fas ligand during apoptosis induced by camptothecin in p53 mutant human colon carcinoma cells. Oncogene, 20, 1852-1859. DONG, Y. B., YANG, H. L. & MCMASTERS, K. M. 2003. E2F-1 overexpression sensitizes colorectal cancer cells to camptothecin. Cancer Gene Ther, 10, 168-178. Acknowledgement • • • Scienfund Grant, AMDI Research Fund Prof. Ishak Mat, Dr. Syed Atif Ali for the cell lines provided Co-researchers: Nor Jalilahtul Mahfuzah Noordin Ira Maya Sophia Nordin Shahrul Bariyah Sahul Hamid Terima Kasih Mentransformasikan Pengajian Tinggi Untuk Kelestarian Hari Esok