CBME - Department of Obstetrics and Gynaecology
advertisement

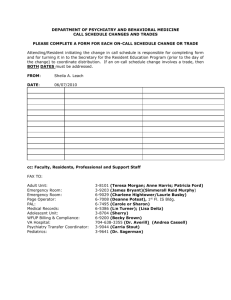
CBME – Department of OB/GYN Sue Chamberlain CBME workshop Sept 2015 CBME – Where we are at Transition to CBME occurring on 2 levels Development of EPA’s and identification of milestones Change in assessment practices EPA development Rounds 2013 – Introduction of EPA’s, Competency by Design to Department of Obstetrics and Gynecology Grand 2014 – development of preliminary working set of EPA’s while reviewing residency objectives Summer EPA development 2014 – Development of Scope of Practice EPA’s July 2015 – Development of Stage-Specific EPA’s with identification of relevant associated milestones January Transitions to discipline EPA’s 1. 2. 3. 4. 5. 6. Perform a history and physical in a pregnant patient. (Jr OB and Jr Clinics – Blocks 1-2) Perform a gynecologic history and physical examination. (Jr Clinics – Blocks 1-2) Demonstrate basic knowledge of obstetric and gynecologic presentations. (Jr OB and Jr clinics) Perform a basic assessment of a patient arriving to labour and delivery. (Jr OB) Perform a basic assessment of a patient arriving in the ER. (Jr OB) Assist in the operating room and write basic post-op orders for obstetric and gynecologic patients. (Jr OB) Curriculum/rotations – JR OB, JR clinics, Boot camp, attendance at clerkship seminars Assessment – Clerkship oral examinations, Direct observation with Patient encounter forms for clinics and L&D Foundations EPA’s Provide low-risk antenatal care in the outpatient setting. (Jr clinics ) Perform basic Obstetric USS. (Jr OB) Assess and triage patients arriving to Labour and Delivery.(Jr OB, on-call) Diagnose and manage common inpatient obstetric complications including preterm labour, pre-eclampsia and PPROM. (Jr OB, on-call) 5. Manage Normal Labour and Childbirth and post-partum. (Jr OB, on-call) 6. Manage gynecologic patients requiring family planning. (women’s clinic) 7. Diagnose and manage general gynaecologic presentations. (on-call, Jr clinics) 8. Provide surgical management of gynaecologic patients including surgical treatment (minor surgeries) and peri-operative care. (Jr gyne, Jr gyne onc) 9. Provide consultation on common and uncomplicated Obstetric and Gynecologic problems in the Emergency Department. (Jr OB, on-call, jr gyne ) 10. Resuscitate, stabilize, and triage patients in an emergency department, delivery room, or inpatient acute care setting and transfer to a higher level of care as required. (Jr OB. on-call, ER rotation, jr gyne) 11. Participate in handover. (Jr OB, on-call) 1. 2. 3. 4. Foundations EPA’s Rotations – PGY 1/2: clinics – 2 blocks Jr OB – 4 blocks ER – 1 block women’s clinic – 1 block Jr gyne – 4 blocks Jr gyne onc – 4 blocks on-call – through first 2 years Jr Foundations EPA’s 1. 2. Provide low-risk antenatal care in the outpatient setting. (Jr clinics ) Perform basic Obstetric USS. (Jr OB) 3. Assess and triage patients arriving to Labour and Delivery.(Jr OB, on-call) 4. Diagnose and manage common inpatient obstetric complications including preterm labour, pre-eclampsia and PPROM. (Jr OB, on-call) 5. Manage Normal Labour and Childbirth and post-partum. (Jr OB, on-call) Manage gynecologic patients requiring family planning. (women’s clinic) Diagnose and manage general gynaecologic presentations. (on-call, Jr clinics) Provide surgical management of gynaecologic patients including surgical treatment (minor surgeries) and peri-operative care. (Jr gyne, Jr gyne onc) 9. Provide consultation on common and uncomplicated Obstetric and Gynecologic problems in the Emergency Department. (Jr OB, on-call, jr gyne ) 10. Resuscitate, stabilize, and triage patients in an emergency department, delivery room, or inpatient acute care setting and transfer to a higher level of care as required. (Jr OB. on-call, ER rotation, jr gyne) 11. Participate in handover. (Jr OB, on-call) 6. 7. 8. Manage Normal Labour and Childbirth Core Activities Key and Enabling Competencies Assess and triage Manage normal labour Manage normal vaginal birth ME 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 ME 2.1, 2.2, 2.3, 2.4 ME 5.1, 5.2, 5.3, ME 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 ME 2.1, 2.2, 2.3, 2.4 ME 3.1, 3.2, 3.3, 3.4, ME 5.1, 5.2, 5.3, CM 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 CM 2.1, 2.2, 2.3, 2.4, CM 3.1, 3.2, CM 4.1, 4.3, CM 5.1. 5.2 CL 1.1, 1.2, 1.3 CL 2.1,2.2, CL 3.2 L1.2 L2.1, 2.2 ME 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 ME 2.1, 2.2, 2.3, 2.4 ME 3.1, 3.2, 3.3, 3.4, ME 5.1, 5.2, 5.3 CM 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 CM 2.1, 2.2, 2.3, 2.4, CM 3.1, 3.2, CM 4.1, 4.3, CM 5.1. 5.2 CL 1.1, 1.2, 1.3 CL 2.1,2.2, P 1.1, 1.2 P 1.1, 1.2 CM 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 CM 2.1, 2.2, 2.3, 2.4, CM 3.1, CM 4.1, CM 5.1. 5.2 CL 1.1, 1.2, 1.3 CL 2.1, P 1.1, 1.2 L 1.2 L2.1, 2.2 Core of discipline EPA’s 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Provide high-risk antenatal care in the outpatient setting. (MFM) Perform Obstetric USS. (MFM) Manage Complicated Labour and Childbirth. (Sr OB) Manage complications in the post-partum patient.(Sr OB) Diagnose and manage gynaecologic presentations in the pediatric and adolescent population. (REI) Manage presentations in the menopausal population.( REI) Diagnose and manage general gynaecologic presentations. Diagnose and manage basic reproductive medicine presentations. (REI) Diagnose and manage basic gynaecologic oncology presentations with referral to subspecialty care as necessary. (Gyne onc) Assess and treat patients with Cervical dysplasia (Gyne Onc) Diagnose and manage basic urogynecologic presentations. (Urogyne) Provide surgical management of gynaecologic patients including surgical treatment and perioperative care. (Chief, Sr Gyne) Provide consultation on Obstetric and Gynecologic problems to other Health Care Providers. (Sr OB, Chief) Diagnose and manage sexual health concerns in women. (Sr Clinics, Chief) Provide care to multiple services and patients as an on-call physician. ( Sr on-call) Engage in self-regulated learning including, self-assessing, planning, and monitoring progress Support others’ learning including formal and bedside teaching and assessment Core of Discipline EPA’s Rotations: PGY 3-5 MFM – 4 blocks REI – 4 blocks Urogyne – 4 blocks Gyne Onc – 4 blocks Sr OB – 4 blocks Sr clinics – 2 blocks Chief – 4 blocks On-Call Core of discipline EPA’s 3. Provide high-risk antenatal care in the outpatient setting. (MFM) Perform Obstetric USS. (MFM) Manage Complicated Labour and Childbirth. (Sr OB) 4. Manage complications in the post-partum patient.(Sr OB) 5. Diagnose and manage gynaecologic presentations in the pediatric and adolescent population. (REI) Manage presentations in the menopausal population.( REI) Diagnose and manage general gynaecologic presentations. Diagnose and manage basic reproductive medicine presentations. (REI) Diagnose and manage basic gynaecologic oncology presentations with referral to subspecialty care as necessary. (Gyne onc) Assess and treat patients with Cervical dysplasia (Gyne Onc) Diagnose and manage basic urogynecologic presentations. (Urogyne) Provide surgical management of gynaecologic patients including surgical treatment and perioperative care. (Chief, Sr Gyne) Provide consultation on Obstetric and Gynecologic problems to other Health Care Providers. (Sr OB, Chief) Diagnose and manage sexual health concerns in women. (Sr Clinics, Chief) Provide care to multiple services and patients as an on-call physician. ( Sr on-call) Engage in self-regulated learning including, self-assessing, planning, and monitoring progress Support others’ learning including formal and bedside teaching and assessment 1. 2. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Manage complications in the postpartum patient Core Activities Inpatient postpartum care Outpatient postpartum care – clinic encounter/on-call Key and Enabling ME 1.1, 1.2, 13, 1.4, 1.5, 1.6 ME 2.1, 2.2, 2.3, 2.4 ME 3.1, 3.2, 3.3, 3.4 ME 4.1 ME 5.2 CM 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 CM 2.1, 2.2, 2.3, 2.4 CM 3.1, 3.2 CM 4.1, 4.3 CM 5.1, 5.2 CL 1.1, 1.2, 1.3 CL 2.1, 2.2, CL 3.1, 3.2 L 1.2, L 2.2 A 1.1, 1.2., 1.3 P 1.1, 1.3 P 3.1 P 4.3 ME 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 ME 2.1, 2.2, 2.3, 2.4 ME 3.1, 3.2, 3.3, 3.4, ME 4.1, ME 5.1, 5.2, 5.3, CM 1.1, 1.2, 1.3, 1.4, 1.5, 1.6 CM 2.1, 2.2, 2.3, 2.4, CM 3.1, 3.2, CM 4.1, 4.2, 4.3, CM 5.1. 5.2 CL 1.1, 1.2, 1.3 CL 2.1,2.2, CL 3.1, 3.2 L1.2 L2.1, 2.2 L3.1 A 1.1, 1.2, 1.3, S 2.1, 2.3, P 1.1, 1.2, 1.3, 1.4, 1.5 Competencies Assessment Based on observation of clinical activities Mid-rotation feedback forms Online ITERs – One45 Quarterly reviews of all residents by all department members Assessment OB/GYN Goal to replace current forms with systematic observation of resident performance CARS Skills observation Assessment – Steps/progress to date Review of Rotation Objectives PGY1-5 (spring 2014) Is it assessable? Is it currently assessed? Identification of means of assessment for all objectives Identification of objectives that do not currently have documented assessment (beyond ITER) Assessment – Steps/progress to date Revision of Rotation Objectives for PGY 1 rotations – JR OB, Ambulatory clinics (summer 2014) Identified Core Clinical Activities that encompassed the rotation objectives Developed rubrics for – SVD, Patient triage, Postpartum care and discharge, Buddy Call, Informed Consent, MSF and other core activities (Thank-you to Surgery, Peds, Family Med and others!) Skills checklist – to ensure that residents were observed and deemed competent in procedural skills before these were entrusted Assessment – Steps/progress to date Introduction to Faculty and residents – Sept 2014 Grand Rounds Reviews of EPA’s, Milestones, Competency by Design Description of rubrics Clarification of expectations for completion of rubrics and checklist Circulation for revisions/feedback prior to implementation Piloting with PG1’s: Sept 2014 – June 2015 Assessment – Steps/progress to date Implementation with PG1’s: July 2015 Fall 2015 – introduction of new rubrics for piloting Journal Club Senior resident On-call PGY-2 rotation assessment Assessment – Challenges! Document completion Fast-paced service Resident hesitancy – don’t want to bother staff, discomfort with face-to-face feedback Communication/understanding of expectations (residents and faculty) Assessment – Steps/progress to date Revision of Rotation Objectives for PGY 1 rotations – JR OB, Ambulatory clinics (summer 2014)