Types II and III: Antibody-Mediated and Antigen
advertisement
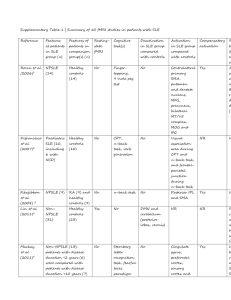
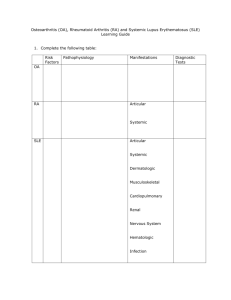
Types II and III Immediate Hypersensitivity: Antibody-Mediated and Antigen-Antibody Complex-Mediated Immediate Hypersensitivity Folder Title: AgAbHype(NoTP) Updated: December 03, 2015 Four Types of Hypersensitive (Allergic) Responses Type II Immediate Hypersensitivity: Antibody-Mediated Cytotoxic Attack on Host Cells Complement-Mediated or ADCC* - Mediated *ADCC = Antibody-dependent Cell-mediated Cytotoxicity Examples Shown: ABO Blood Group in Red Blood Cell Transfusions Rh Factor in Erythroblastosis Fetalis Auto-antibody to Acetyl Choline Receptors in Myasthenia Gravis If Red Cell Surface Antigens are not correctly matched in Red-Blood Cell Transfusion….. A, B, or AB Blood into O Recipient A Blood into B or O Recipient B Blood into A or O Recipient (Type O blood is tolerated by A, B, AB, or O Recipients) If there are RBC blood group incompatibilities between donor and recipient: Can get antibody attack on A or B antigens on RBC Complement Lysis of Red Cells with bound antibody Or ADCC (Cell Mediated Cytotoxicity) on Red Cells Baby with Hemolytic Disease of the New-Born (HDNB) Should be anti-ACR (Receptor) Auto-antibody to Acetyl Choline Receptor: Blockage of Acetyl-Choline Signalling in Myasthenia Gravis From Roitt, 4th Ed. Fig. 23.16 Complement-dependent attack on Ig-Fc labelled acetyl choline receptors and progressive damage to muscle cell end-plate and loss of acetyl-choline receptors. Myasthenia Gravis Definition Myasthenia gravis (MG) is an autoimmune disorder. The signal from the nerves to the muscles is blocked. As a result, the muscle cannot move and become increasingly weaker. Symptoms may grow more severe over time. This is a potentially serious condition. MG requires care from your doctor. If you suspect you have this condition, contact your doctor immediately. Causes The root cause of MG is unknown. It occurs when the body’s immune system attacks receptors in muscle. Normally, these receptors respond to the chemical acetylcholine (ACh). This chemical allows nerve signals to prompt the muscles to move. When the immune system prevents these receptors from working well, the muscles cannot respond to nerve signals. The thymus is thought to play a role in some cases of MG. The thymus is an organ behind the breastbone. Immune proteins called antibodies are produced there. It is these antibodies that may target the ACh receptors. It is still not clear why the thymus begins to produce these. helper T-cells that activate an auto-reactive B-cell antibody response to acetylcholine receptors. Please put away all desktop stuff and all electronic devices except your NXT Transmitter. "Frustrated Phagocytosis" as a Damage Mechanism in Types II and III Hypersensitivity From Roitt, 4th Ed., Fig. 23.4 Type III Immediate Hypersensitivity: Antigen-Antibody Complex Mediated Attack on Host Tissues Localized: Arthritis, Nephritis Systemic: Serum Sickness Complement-Mediated: • Complement Activation - General Response to AgAb Deposition • Complement Deficiency Failure to Clear Autoimmune AgAb Complexes e.g. Systemic Lupus Erythrematosis (SLE) Features of AgAb-Complex Disposition Contributing to Type III Immediate Hypersensitivity: Normal Removal of AgAb Complexes • By macrophages (Ab binds to Fc receptor) • By RBC binding of C3b Opsin to CR1 (C3b-receptor); • Transport to Spleen for removal. Site of Accumulation of AgAb Complexes • At local sites (e.g. joints, kidneys, lungs) • Systemically - "Serum Sickness" Persistence of Triggering Antigen Role of Complement • Keeps AgAb from precipitating in tissues • Marks AgAb for Removal by Reticuloendothelial System • Complement Deficiency leads to AgAb Accumulation Antigen-generation and Persistence in Type III Immediate Hypersensitivity Persistent Infection • • • • • • • Leprosy Malaria Viral hepatitis Dengue hemorrhagic fever Staphylococcal Endocarditis Streptococcal glomerulonephritis Mononucleosis Autoimmunity • Rheumatoid arthritis • Systemic Lupus Erythrematosis (Also autoreactive T-Cells) Persistent Exogenous Acquisition (Inhalation of Ag) • Extrinsic Allergic Alveolitis (e.g. Fungal antigens) Systemic Lupus Erythematosus Patient (Systemic autoimmune Disease). Mediated by auto-reactive T-cell clones. Attacks DNA and blood cells and other. Shut down T-cell response with anti-CD4 Monoclonal attacking activated T-cells. See Figure 16 -07, p. 530, Kuby 7th Edition A.D.A.M. Medical Encyclopedia. Systemic lupus erythematosus Disseminated lupus erythematosus; SLE; Lupus; Lupus erythematosus; Discoid lupus Last reviewed: February 14, 2011. Systemic lupus erythematosus (SLE) is a long-term autoimmune disorder that may affect the skin, joints, kidneys, brain, and other organs. Causes, incidence, and risk factors Systemic lupus erythematosus (SLE) is an autoimmune disease, which means the body's immune system mistakenly attacks healthy tissue. This leads to long-term (chronic) inflammation. The underlying cause of autoimmune diseases is not fully known. SLE is much more common in women than men. It may occur at any age, but appears most often in people between the ages of 10 and 50. African Americans and Asians are affected more often than people from other races. SLE may also be caused by certain drugs. For information on this cause, see Drug-induced lupus erythematosus Stop here: Thursday Dec. 3, 2015 Initial: Antigen-Antibody Complex Activation of Complement 1. Complement break-down product activation of Type 1 mast cell degranulation with histamine release. Extravasation of neutrophils. 2. Neutrophil activation by complement break-down products. Tissue damage by constant inflammation Autoantibodies to basement membrane proteins. Kidney failure A.D.A.M. Medical Encyclopedia. Goodpasture syndrome Anti-glomerular basement membrane antibody disease; Rapidly progressive glomerulonephritis with pulmonary hemorrhage; Pulmonary renal syndrome; Glomerulonephritis - pulmonary hemorrhage. Last reviewed: August 13, 2009. Goodpasture syndrome is a rare disease that can involve rapidly progressive kidney failure along with lung disease. However, some forms of the disease involve just the lung or kidney, not both. Causes, incidence, and risk factors Goodpasture syndrome is an autoimmune disorder, a condition that occurs when the immune system mistakenly attacks and destroys healthy body tissue. Persons with this syndrome develop substances that attack a protein called collagen in the tiny air sacs in the lungs and the filtering units (glomureli) of the kidney. These substances are called anti-glomerular basement membrane antibodies. Glomerular basement membrane is a part of the kidneys that helps filter waste and extra fluid from the blood. Anti-glomerular basement membrane are antibodies against this membrane. They can lead to kidney damage. Sometimes the disorder is triggered by a viral respiratory infection or by breathing in hydrocarbon solvents. In such cases, the immune system may attack organs or tissues because it mistakes them for these viruses or foreign chemicals. The immune system's faulty response causes bleeding in the air sacs and inflammation in the kidney's filtering units. Men are eight times more likely to be affected than women. The disease most commonly occurs in early adulthood. Features of Rheumatoid Arthritis Auto-IgM-antibody attack (“Rheumatoid Factor” ) on the Fc region of IgG antibodies. Chronic antigen-antibody deposition in joint. Activation of complement and induction of Type III hypersensitivity with chronic inflammation of joints. Effects also on cardiovascular, respiratory, and hematological systems. Elevated occurrence in women ages 40 to 60. Please put away all desktop stuff and all electronic devices except your NXT Transmitter. Which of the following can lead to Type-III Hypersensitivity: Immune-complex Disease? (Enter all correct responses. Set them up as a string of numbers (e.g. 123678) then press enter when you have all of the correct numbers in the string 1. 2. 3. 4. 5. 6. 7. 8. Failure to resolve an inflammatory disease. Failure of an antibody to recognize and antigen Auto-immune response to a self-antigen. Severe chronic immunodeficiency. High dose persistent exposure to an immunogen. Defect in complement response. Systemic treatment with a therapeutic immunogen. Over-production of IgE antibody Response Counter 0% 0% 1. 2. 0% 0% 0% 0% 0% 0% 3. 4. 5. 6. 7. 8.