Presentation at the fight against cholera and diarrheic diseases in
advertisement
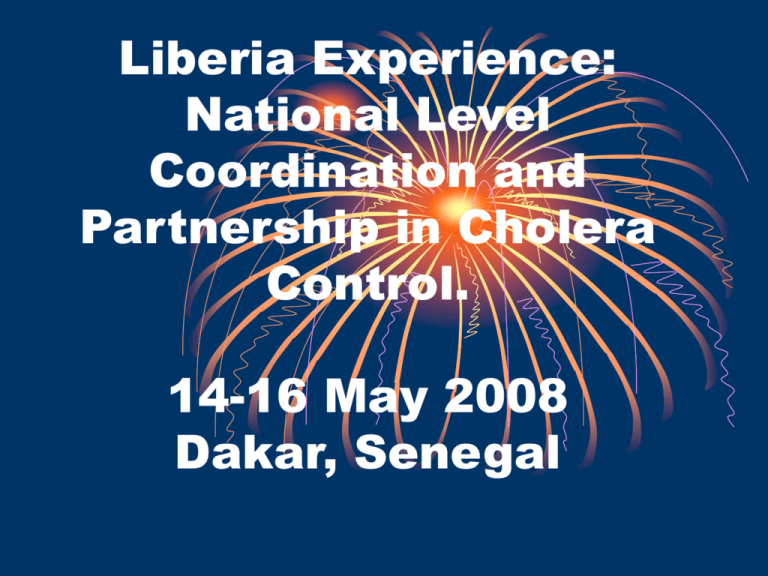
Liberia Experience: National Level Coordination and Partnership in Cholera Control. 14-16 May 2008 Dakar, Senegal Background Situation • 15 counties and 88 districts • Estimated 3 million people - Sparse Pop - density, 84 per sq mile except Monrovia (1 million people) - Infrastructures destroyed by war - Access to safe water - 24% (UNDP 2006), sanitation nationwide - 26% - (UNICEF, 2006) - Low households incomes. ¾ pop on less than US$1 a day (iPRS, 2007) - Infant mortality rate, 102/1000 & crude morality estimate 1.1/10,000/day (CFSN, 2006). - Diarrhea 2nd cause in morbidity/mortality - Seasons– Wet –April – Oct, Dry Nov-March. Cholera hot spot areas • Occurrence (slides line graph) Trends :2005 -2007 1400 1200 1000 800 2005 2006 2007 600 400 200 0 jan feb mar april may jun jul aug sept oct nov dec Liberia cholera trend in 2008 Cases and Deaths 250 231 200 150 Cases 107 100 Deaths 80 50 2 0 0 0 Januar y Febr uar y Months M ar ch LIBERIA MAP SHOWING CHOLERA HOT SPOTS COUNTIES Lofa Gbarpolu Grand Cape Mount Bong Nimba Bomi Margibi Montserrado Grand Bassa Grand Gedeh River Cess River Gee Sinoe Grand Kru Maryland National Strategy • • • • Coordination Partnership Surveillance / EWARNS Institutional capacity Coordination • Multisectoral approach • Decentralized epidemic task force • Standardized case management, surveillance & monitoring • Partners mapping & up dates. • Leadership – MOH/CHT • Annual integrated plans. • Pooled contingency plans / stocks Partnerships • Relevant GOL Ministries / Depts • CBOs Hygiene behaviors promotion • UN agencies: UNICEF, WHO, UNMIL - Tech. asst; Finance; Resources; logistics. • Health/WATSAN NGOs and WATSAN CONSORTIUM • Communities Surveillance • Standardized data collection tools & analysis at county levels. • Pre-positioned investigation & case detection teams. Institutional capacity • INGO – (9), LNGO) (26) & CBOs in 4 counties • UN agencies –(WHO, UNICEF, UNHCR) • Community – ORT corners / Treatment centers, trained • Trained staffs & community own resource persons (volunteers). Successes • Consistent reduction in attack rates • Sustained multisectoral & integrated approach to cholera control • Availability of trained local resources at community level. • Sustained partners support. • Decentralized chlorine stocks • Response within 24hrs-48hrs • Coherence approaches &Team work. • Functional surveillance systems OUR UNIQUE WAYS OF WORKING. • Merged GOL coordination & WASH cluster. • Innovations - Pooled funding (DFID/ECHO) -WASH consortium – 5 INGOs – services delivery & capacity building through GOL. - Pool funding from partners Limitations/Challenges • Deplorable infrastructure states • High Poverty level • Meager resources skewed towards curative services. • Low WASH coverage. • Insufficient resources – human & materials • Weak national systems / policies enforcement. • Inadequate mid-level skilled health personnel to manage cholera control • Transition from humanitarian to development. • Low access to health services • Unreliable data for planning LESSONS LEARNT • • • • Pre positioning of stocks - chlorine Routine Well chlorination. HH water chlorination practice Pre-mapping and identification of resources at county levels. • Community based hygiene education • ORT corners / Treatment centers • Sustained partnership & coordination Our Needs • Long-term funding from donors, targeting AWD/Cholera / WASH. • Support for Skill training on cholera management. • Expansion of decentralized cholera confirmation laboratories - Counties • Research on cholera to establish evidences for intervention. • Support for sustainable WASH activities.