Nervous system VIVA's
advertisement
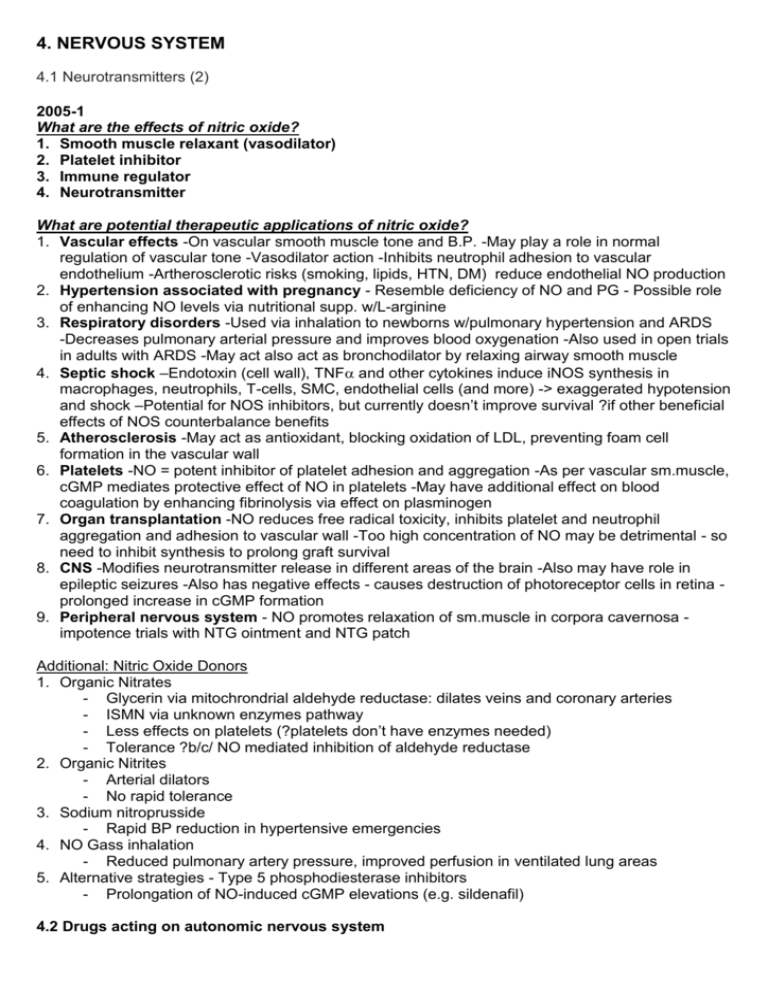
4. NERVOUS SYSTEM 4.1 Neurotransmitters (2) 2005-1 What are the effects of nitric oxide? 1. Smooth muscle relaxant (vasodilator) 2. Platelet inhibitor 3. Immune regulator 4. Neurotransmitter What are potential therapeutic applications of nitric oxide? 1. Vascular effects -On vascular smooth muscle tone and B.P. -May play a role in normal regulation of vascular tone -Vasodilator action -Inhibits neutrophil adhesion to vascular endothelium -Artherosclerotic risks (smoking, lipids, HTN, DM) reduce endothelial NO production 2. Hypertension associated with pregnancy - Resemble deficiency of NO and PG - Possible role of enhancing NO levels via nutritional supp. w/L-arginine 3. Respiratory disorders -Used via inhalation to newborns w/pulmonary hypertension and ARDS -Decreases pulmonary arterial pressure and improves blood oxygenation -Also used in open trials in adults with ARDS -May act also act as bronchodilator by relaxing airway smooth muscle 4. Septic shock –Endotoxin (cell wall), TNF and other cytokines induce iNOS synthesis in macrophages, neutrophils, T-cells, SMC, endothelial cells (and more) -> exaggerated hypotension and shock –Potential for NOS inhibitors, but currently doesn’t improve survival ?if other beneficial effects of NOS counterbalance benefits 5. Atherosclerosis -May act as antioxidant, blocking oxidation of LDL, preventing foam cell formation in the vascular wall 6. Platelets -NO = potent inhibitor of platelet adhesion and aggregation -As per vascular sm.muscle, cGMP mediates protective effect of NO in platelets -May have additional effect on blood coagulation by enhancing fibrinolysis via effect on plasminogen 7. Organ transplantation -NO reduces free radical toxicity, inhibits platelet and neutrophil aggregation and adhesion to vascular wall -Too high concentration of NO may be detrimental - so need to inhibit synthesis to prolong graft survival 8. CNS -Modifies neurotransmitter release in different areas of the brain -Also may have role in epileptic seizures -Also has negative effects - causes destruction of photoreceptor cells in retina prolonged increase in cGMP formation 9. Peripheral nervous system - NO promotes relaxation of sm.muscle in corpora cavernosa impotence trials with NTG ointment and NTG patch Additional: Nitric Oxide Donors 1. Organic Nitrates - Glycerin via mitochrondrial aldehyde reductase: dilates veins and coronary arteries - ISMN via unknown enzymes pathway - Less effects on platelets (?platelets don’t have enzymes needed) - Tolerance ?b/c/ NO mediated inhibition of aldehyde reductase 2. Organic Nitrites - Arterial dilators - No rapid tolerance 3. Sodium nitroprusside - Rapid BP reduction in hypertensive emergencies 4. NO Gass inhalation - Reduced pulmonary artery pressure, improved perfusion in ventilated lung areas 5. Alternative strategies - Type 5 phosphodiesterase inhibitors - Prolongation of NO-induced cGMP elevations (e.g. sildenafil) 4.2 Drugs acting on autonomic nervous system 4.2.1 Sympathetic (1) 2009-2 What is the mechanism of action of amphetamines? - Indirectly cause increased release of catecholamines at synapses - Competitively inhibits dopamine transport/re-uptake at pre-synaptic neurone (DAT), and intracellularly inhibits VMAT displacing DA from the vesicles -> causing non-vesicular release (reversal of DAT direction) of dopamine into synapse (& similarly for other catecholamines) Describe the effects of amphetamines? Catecholamines: (increased arousal & decreased sleep) elevated HR (dysrhythmias) and BP Dopamine release: addiction, euphoria, potentially abnormal movements & psychosis Serotonin: Appetite suppression, hallucinogenic & hyperthermia 2005-2 Describe the effects of an intravenous adrenaline infusion on the CARDIOVASCULAR system. Adrenaline is an (endogenous) agonist at both and receptors 1: Increased cardiac output (chronotropy + inotropy) 2: vasodilation with widened pulse pressure (2 – relaxation of skeletal SMC, also resp and uterine) Higher doses: > 1: vasoconstriction with narrowing of pulse pressure and increase in TPR What are the potential side-effects or complications of an adrenaline infusion 1. GENERAL: Anxiety, tremor, nausea, vomiting, pallor 2. HEART & CIRCULATION: Palpitations and/or arrhythmias, myocardial ischaemia, hypertension 3. METABOLIC ( effect): hyperglycaemia, metabolic (lactic) acidosis, hypokalemia How does the effect of adrenaline differ from noradrenaline? 1. Noradrenaline peripheral alpha effect- vasoconstriction, but 1>>2 2. Adrenaline mixed peripheral alpha and beta as above 3. Noradrenaline lesser cardiac effect 4. Slightly different side-effect profile (metabolic effects due predominantly to beta receptor activation) 2011-2 What is the adrenoreceptor selectivity of noradrenaline alpha1 = alpha2 alpha 1: post-synaptic effector cells, especially smooth muscle alpha 2: presynaptic nerve terminals, platelets, lipocytes, smooth muscle beta1 >> beta2 beta 1: post synaptic effector cells, especially heart, lipocytes, brain Describe the cardiovascular effects of infused noradrenaline 1. Increases peripheral vascular resistance 2. Increases SBP and DBP 3. Little chronotropy 4. Positive inotropy 2009-1 What are the effects of adrenaline on the blood vessels in different tissue What receptors mediate these effects Tissue Receptor(s) Tone Cutaneous, mucous membranes ++ Venous + , Renal + , D1 Splanchnic -/+* , Skeletal muscle -/+* 2, Total peripheral resistance -/+* *Low doses decrease (physiologic e.g. in exercise), high doses increase (e.g. in infusion) Describe the effects of adrenaline on other organs besides the heart System Receptor Effect Respiratory Bronchodilation 2 Eyes Pupillary dilation, IOP, aqueous humor GI Relaxation of gastric smooth muscle Genitourinary Uterine smooth muscle relaxation, Bladder relaxation, Bladder sphincter contraction, Ejaculation Apocrine Sweat glands - palm of hands Salivary Leading to dry mouth Lipocytes Lipolysis - increased fatty acids and glycerol in circulation 3 Metabolism Liver: Enhanced glycogenolysis Metabolic acidosis Potassium uptake into cells, decreased extracellular potassium 2 Hormones Insulin, glucagon (2) Renin 1 (2) Leucocytosis Demargination of white cells 2003-2 Regarding-agonists, by what cellular mechanism do they exert their effects? - Bind to specific receptor - G-protein activation - Stimulate adenyl cyclase - Increased cyclic AMP - Increased free intracellular Ca - Activate protein kinase Note: 1 receptors (phenylephrine) 2 receptors (clonidine) -> IP3 and DAG -> cAMP Compare the cardiovascular of adrenaline and dobutamine. Drug Receptor Notes agonists Phenylephrine Not a catechol derivative (nil COMT) so long duration of action 1>2>>> Mydriatic, decongestant, increases BP Clonidine Reduce BP via CNS (vasomotor area) 2>1>>> Mixed and Noradrenaline 1=2, 1>>2 Vasoconstricts, positive inotrope (minimal chronotropy) Adrenaline Vasoconstricts except skeletal m, positive inotrope/chronotrope 1=2, 1=2 agonists Dobutamine* 1>2>>> Positive inotrope > chronotrope (vasoconstricts) CO Isoproterenol 1=2>>> Positive chronotrope and inotrope, vasodilates (CO, MAP) Albuterol Asthma treatment (ritodrine – uterine relaxatn in prem labour) 2>>1>>> Dopamine agonists Dopamine Vasodilation of renal, coronary, cerebral (via D1) and D2 D1=D2>>>> suppresses noradrenaline release. High doses mimick adrenaline Fenoldopam D1>>D2 *Dobutamine is a selective 1 agonist. - Increases cardiac output with less reflex tachycardia as it has fewer 2 effects. Comes as racemic mixture of +ve and –ve isomers. One isomer has B agonist and alpha antagonist effects; the other has alpha agonist effects. Additional: Receptor regulation/Desensitisation - Repsonses mediated are not fixed and static but modulated by: a. Catecholamines themselves b. Hormones and drugs c. Age and disease - Adrenoceptors display desensitization after exposure to agonists - Mechanisms may occur slowly (hours-days) involving transcription at receptor protein level or migration to the cell surface - May occur quickly (minutes) involving covalent modification (phosphorylation, protein association, change to subcellular location) a. Homologous desensitization: Due to repeated/sustained stimulation by agonist (G-protein coupled receptor kinase (GRK) -> higher affinity for arrestins -> reduced G protein activation upon receptor stimulation) b. Heterologous desensitization: Desensitisation of one receptor results in desensitization of another receptor not directly activated by the agonist in question Second messenger feedback (cAMP or receptor activation -> increased protein kinase -> structurally similar receptor phosphorylation) 4.2.2 Parasympathetic (1) 2008-1, 2007-1, 2003-2 What is the mechanism of action of atropine? (2010-1) Reversible block of cholinergic muscarinic receptors, non-selective between the M1, M2 and M3 sub-types. Very selective for muscarinic (vs nicotinic or histamine c.f. synthetic antimuscarinics) What are the toxic effects of atropine? (2006-2 – benztropine) Dry as a bone: Dry mucous membranes, urinary retention, ileus Blind as a bat: Mydriasis (pupilary dilation), acute angle glaucoma Red as a beet: Hyperthermia, flushing, tachycardia Mad as a hatter: Central anticholinergic syndrome – delirium w/ visual hallucinations What are the therapeutic uses for atropine? 1. CNS disorders - Decrease tremor and rigidity in Parkinson’s disease - Scopolamine for motion sickness 2. Opthalmologic - Mydriasis and cycloplegia (but caution b/c toxicity, and agonists shorter acting) 3. Respiratory - Atropine was used to dry secretions pre-op with older irritant inhalants - Quaternary amine ipatropium (synthetic analogue of atropine) used in COPD 4. Cardiovasular - Symptomatic bradycardias, especially when vagally mediated - SA node: blocks vagal slowing -> reflex tachycardia - AV node: increases conduction -> shorten PR 5. Gastrointestinal - Rarely now, but low dose with opioid for diarrhoea (e.g. traveler’s) 6. Urinary - Was used for urinary urgency, but replaced by M3 selective oxybutinin 7. Cholinergic poisoning - OGP poisoning - Inocybe Mushroom poisoning 8. Others - Adjunct to reversal of non depolarising muscle relaxants and suxamethonium administration in young infants What is benztropine? (2006-2) Centrally acting anti-muscarinic. As a tertiary amine it is widely distributed in the body including the CNS (quaternary amines such as ipatropium poorly taken up by CNS). Used as an adjunct in the treatment of the tremor in Parkinson’s. Describe the pharmacokinetics of atropine (2010-1) - Well absorbed (even transdermal with suitable vehicle e.g. scopolamine patches) - Natural and tertiary forms widely distuburted incl CNS, vs quaternary low CNS uptake and effects - Quaternary (e.g. ipatropium) only 10-30% absorbed b/c decreased lipid solubility of charged molecule - t½ has 2 phases, rapid 2h and slow is 13h - 50% excreted unchanged (the rest hydrolysis and conjugates) - Effects on eye last longer >72 hours (rapid decline in other tissues) What are the effects of atropine on heart rate - Lower doses often an initial bradycardia (Blocks prejunctional M1 receptors) - Tachycardia 2003-2 What is the mechanism of action of indirectly acting cholinomimetics? Inhibition of the enzyme acetylcholinesterase thereby increasing the concentration of endogenous acetylcholine in the vicinity of cholinoreceptors What types of indirectly acting cholinomimetics are there? Please give examples. Type Alcohol Carbamates Organophosphates Name Edrophonium Neostigmine Physostigmine Pyridostigmine Echothiophate Uses Myaesthenia gravis, arrythmias, ileus Myaesthenia gravis, ileus Glaucoma Glaucoma Duration Minutes 0.5 – 2h 3 – 6h 0.5 – 2h 100hours What are the cardiovascular effects of these groups of drugs? 1. Cardiovascular - Action on both nicotinic and muscarinic receptors - Action on the neuromuscular end plate and autonomic ganglion cells - Both sympathetic and parasympathetic ganglia can be activated - Parasympathetic effects generally predominate - Bradycardia, decreased CO, decreases contractility, no change or modest decrease in BP - OD may cause tachycardia and hypotension 2. CNS - High conc -> convlusions, coma and respiratory arrest 3. Eye – miosis (pupilary contraction) and ciliary muscle contraction 4. Lung – bronchial contraction and secretions stimulation 5. GI – increased motility, sphincter relaxation and secretions 6. Urinary bladder – detrusor contraction and trigone and sphincter relaxation 7. Glands – sweat, saliva, lacrimal and nasopharyngeal secretions SLUDGE (OGP poisoning): salivation, lacrimation, urination, defecation, GI distress and emesis 4.3 Local anaesthetics (1) 2011-2, 2006-1, 2004-2 What classes of local anaesthetics are used in the ED? (Prompt for examples) Amides: lignocaine, prilocaine, bupivacaine, ropivicaine Esters: cocaine, procaine, benzocaine, tetracaine What factors affect the systemic absorption of lignocaine after local infiltration? Systemic absorption is an important cause of toxicity from local anaesthetics. 1. Dose 2. Site of injection - for blocks absorption intercostal > caudal > epidural > brachial plexus > sciatic 3. Drug-tissue binding 4. Tissue blood-flow - absorption will be higher from highly vascular tissues e..g tracheal mucosa vs tendons, or dermis. Blood flow can be altered e.g. an ischaemic arm block or vasoconstrictors 5. Vasoconstrictors – Reduce absorption by 30%, increased concentration at sire increases effect and decreases toxicity What are the toxic effects of lignocaine? 2007-1 (prilocaine), 1. CNS - Initially: Sleepiness, light-headed, visual, auditory disturbance, restlessness - Early toxicity: Circumoral/tongue numbness, metallic taste - Serious/higher: Twitching, nystagmus, seizures 2. Direct neurotoxicity - Radicular irritation with spinals 3. CVS - Direct: Na channel (depress abnormal pacemaker, excitability, conduction) v Ca channel effects at high doses – decrease myocardial contractility - Indirect: via autonomic nervous system cause arteriolar dilatation, hypotension - With bupivicaine can get idioventricular rhythm, broad QRS, EMD 4. Haematologic - Methaemoglobinemia due to accumulation of o-toluidine which oxidizes haemaglobin - If high enough conc. then can cause cyanosis and “chocolate coloured” blood - Important if pre-existing cardiac or pulmonary disease - Treat with reducing agent e.g. methylene blue or ascorbic acid 5. Allergy - Rare with amides as not metabolized to PABA 2009-2, 2007-1 (prilocaine), 2006-1 What is the mechanism of action of local anaesthetics? - Blockade of voltage-gated Na channels in neurones which interferes with AP propagation - Provide pain relief by blocking nociceptive fibers, although other fibers are affected as well - Block is both voltage and time-dependant: i.e. higher affinity for channels in open or inactivated state at more +ve membrane potentials (vs. resting) -> preferentially block rapidly firing neurons - Channels recover 10-1000 slower from inactivated state due to LA -> increased refractory period - Increasing doses lead to higher excitation threshold, slower impulse conduction, lower AP - Blocks conduction if 2-3 nodes of Ranvier in a myelinated nerve are affected Which local anaesthetics are used topically? EMLA (Eutectic Mixture of Local Anaesthetics): mixture of lignocaine and prilocaine Cocaine: ENT procedures (combines vasoconstriction) Eye Drops: Proxymetacaine, amethocaine, oxybuprocaine Benzalkonium: Oral gels 2007-1 How is prilocaine metabolized? - Amide link hydrolysed by P 450 in liver and then renal excretion Significant variation is rates between amides, prilocaine is the fastest (lidnocaine intermediate, bupivicaine is slow) Hepatic disease, reduced flow, competing P450 agents will reduce metabolism Note: Ester local anaesthetics are hydolysed rapidly in the blood by circulating pseudocholinesterase (very short t½ < 1min for procaine) 2006-1 Describe the ideal local anaesthetic for topical application? - Ease of application (Not messy, No dressing) - Well tolerated by kids (Not painful) - Rapid Onset of action - Low (nil) systemic toxicity eg MetHb with EMLA in neonates - High analgesic efficacy - Reasonable duration of action - Not allergenic - May be applied to the skin, the eye, the ear, the nose and the mouth as well as other mucous membranes EMLA (Eutectic Mixture of Local Anaesthetics) - mixture of lignocaine and prilocaine - Eutectic mixture means solidifies at lower temp, both lidnocaine and prilocaine are solids at room temperature, but together form an oil - Provides surface anaesthesia of the skin (partic paeds) - Cutaneous contact (usually under an occlusive dressing) should be maintained for at least 60 min prior to venipuncture - Other LA agents may be absorbed in significant amounts particularly after topical application to the more vascular areas, fatalities have occurred after application of these agents to mucosal surfaces 2004-2 Explain tachyphylaxis associated with LA use - Most local anesthetics are weak bases, pKa 7.5-9.0 - Often marketed at hydrochoride salts (pH 4.0 – 6.0) to maximize aqueous solubility - log[cationic form/uncharged form] = pKa – pH (thus more cationic form at acidic pH) - Receptor site is intracellular, and the uncharged form is thus needed to obtain access through the lipid cell membrane -> the cationic form (“ion trapping”) -> then binds - With repeat injections the LA can deplete the buffering capacity of the tissue -> low pH -> more extracellular LA in cationic form that cannot diffuse though cell membrane - Common in tissues with poor buffering e.g. CSF Extra: Sensitivity depends on: 1. Fiber diameter/type - Smaller > larger b/c distance over which passive AP propagation can occur is smaller - Myelination – 2-3 nodes of Ranvier needed to block propagation (myelinated blocked before unmyelinated nerves of the same size, Type B preganglionic > Type C pain) 2. Firing frequency - Sensory (pain) fibres have a high firing rate and long AP duration, so more sensitive Sensory modalities are affected in the following order: pain, cold, warmth, touch, then pressure 4.4 General anaesthesia 4.4.1 Induction agents (1) Describe the distribution of thiopentone following an IV bolus 2011-1 - Rapidly crosses the BBB, may induce LoC in one circulation time The plasma:brain equilibrium occurs <1min because high lipid solubility Then rapidly redistributed to muscle and body fat Because of this rapid removal from brain tissue it only causes brief LoC Metabolised at about 15% per hour with <1% excreted unchanged by kidneys What are the potential adverse effects of thiopentone? Disadvantages: Hypotension, respiratory depression/transient apnoea, venous irritant, myocardial depression, minimal muscle relaxation and analgesia, hepatic metabolism (vs inhalational agents), reduces hepatic blood flow, can cause porphyric crisis in susceptible patients Advantages: Rapid, Controllable, Amnesic, Reduction of ICP (head trauma, brain tumours), anticonvulsant Describe the pharmacokinetics of propofol? 2009-2, 2003-1 - Intravenous administration (of emulsion) - Distribution t1/2 2-8 min, redistribution t1/2 30-60 min - Metabolised rapidly in liver (10x c.f. barbituates), and total body clearance is greater than hepatic blood flow, suggesting extrahepatic mechanisms also – advantageous in hepatic disease - Excretion in urine as glucuronides and sulphates w/ <1% unchanged What are the side effects of propofol? - Pain on injection is the most common (admixture with lidocaine may minimise) - Respiratory: dose-related depression of central ventilatory drive, apnoea, - Cardiac: Marked decrease in blood pressure through decreased peripheral arterial resistance and venodilatation, and direct negative inotropic effect - Soy/egg allergy - Prolonged administration: severe acidosis in critically ill children, elevated serum lipids, delayed arousal What type of anaesthesia does ketamine produce? 2006-2 - Dissociative anaesthetic state: analgesia, amnesia, catatonia +/- LoC (hypnosis) Which receptor action produces the anaesthesia? - Blockade of glutamic acid (excitatory neurotransmitter) at NMDA receptor subtype How does ketamine affect the cardiorespiratory system? 2009-2, 2006-2 Caridiovascular - HR, BP and cardiac output increase - Peak 2-4 minutes and last 10-20 minutes - Stimulates central sympathetic nervous system, and inhibits re-uptake of noradrenaline at sympathetic nerve terminals Respiratory: Decreased rate, airway reflexes remain intact, bronchodilator What are the side effects of ketamine? Decreased RR Hypersalivation Postoperative disorientation Sensory and perceptual illusions Emergence phenomenon Vomiting Raised ICP (cerebral blood flow, O2 consumption) Rash 4.4.2 Muscle relaxants (1) 2010-2 What is pancuronium - Non-depolarising neuromuscular blocking drug - Quaternary ammonium compound, structure like 2 acetylcholine fragments on a steroid nucleus - Potent competitive antagonist of acetylcholine at nicotinic receptors of skeletal muscle motor endplates Interruption of transmission requires > 70% occupancy Blockade requires > 95% occupancy Describe the pharmacokinetics of pancuronium? - Poorly absorbed after oral admin - Rapidly and widely distributed after iv - Highly ionized, does not readily cross cell membranes and not bound in tissues – Vd is small (~blood volume, 80-140ml/kg) - Rapid elimination (t½ 30min) by urinary excretion (80%) unchanged drug (highly water soluble) - Some hepatic metabolism with biliary excretion - Duration of action >35min What are the adverse effects of pancuronium? - Uncommon - Cardiac (slight block of cardiac muscarinic receptors): Minor tachycardia, hypertension, ↑ CO - Life-threatening anaphylaxis < 1:10,000 2009-2, 2006-1, 2003-1 Describe the mechanism of action of suxamethonium? - Depolarizing neuromuscular blocking drug - 2 molecules of acetylcholine linked via the acetate methyl groups - Acts like acetylcholine except not metabolised effectively at the synapse so much longer effect - Action is terminated by diffusion away from the end plate into the extracellular fluid, where it is hydrolysed by plasma cholinesterase to succinic acid and choline (in fact it is so rapidly metabolised that little of the injected drug reaches the motor end plate) - Very short half life, duration of action 4-8min Phase I (depolarising) - Reacts with nicotinic receptor and opens the channel -> depolarisation of the motor end plate - Not metabolised at the synapse so membranes remain unresponsive to subsequent impulses - Lack of “repriming” leads to flaccid paralysis - This phase I block is augmented by cholinesterase inhibitors (c.f. reversed with non-repol drugs) Phase II (desensitising) - Prolonged exposure -> repolarized but desensitized end-plate - Unclear, but channel block may be more important than agonist action - Behaves more like non-depolarizing block - Is reversed by cholinesterase inhibitors like with non-repol (i.e. neostigmine) What are the side effects of suxamethonium? - Bradycardia- negative inotropic and chronotropic effects (inc. second dose bradycardia) - Hyperkalaemia (esp burns, nerve damage, NM disease, closed head injury) - Increased intra-ocular pressure - Increased intragastric pressure (inc. aspiration) - Muscle pain (in up to 20%) - Malignant hyperthermia (when combined with volatiles) - Sux apnoea in susceptible patients 4.4.3 Volatile anaesthetics (3) 4.4.4 Nitrous oxide (1) 2006-1 What are the organ effects of nitrous oxide? CNS: Analgesic, amnesic, increased cerebral blood flow Renal: Decreased GFR, increased filtration fraction & increased renal vascular resistance CVS: Dose dependant myocardial depression Resp: Reduced respiratory response to CO2 & hypoxia Haematologic: Inactivates B12 -> B12 deficiency and pernicious/megaloblastic anaemia (prolonged exposure) What is the mechanism of action of nitrous oxide? - Directly activate GABA A receptors - GABA A receptor-chloride channel is a major mediator of inhibitory synaptic transmission - Also facilitates GABA mediated inhibition at GABA receptor sites - Leads to: Membrane hyperpolarisation Decreased duration of opening of nicotinic receptor activated channels Decreased excitatory effect of acetylcholine 4.5 Antipsychotic agents (2) 2009-1 What are the clinical uses of chlorpromazine - Typical phenothiazine antipsychotic especially for schizophrenia, also delerium - Sedative for agitation - Antiemetic - Migraine (and hiccups) What are the pharmacodynamic properties responsible for these effects - Antipsychotic: D2 blockade in mesolimbic & mesofrontal systems - Sedation 5-HT blockade - Antiemetic: dopamine receptor blockade in medullary chemoreceptor trigger zone & peripherally on receptors on stomach 2011-1, 2005-1, 2009-1 What are the major side effects of phenothiazine antipsychotics? (e.g. chlorpromazine) - Anti-cholinergic: Dry mouth, dry eyes, urinary retention, constipation - Extra-pyramidal: Dystonia, Parkinson-like effects, akinesia (can’t start), akathisia (can’t stop), tardive dyskinesia - Sedation - Weight gain - Hypotension - Hyperprolactinaemia - ammenorrhea - Occular corneal deposits - Neuroleptic malignant syndrome F – Fever A – Autonomic instability (labile BP and diaphoresis – “sweat shock”) L – Leukocytosis T – Tremor E – Elevated enzymes (elevated CK) R – Rigidity of muscles What mechanisms of drug action are responsible for these side effects? Prompt: What receptors are involved? - Muscurinic cholinoceptor blockade -> anticholinergic - Dopamine receptor blockade -> Extra-pyramidal and NMS - -Adrenoceptor blockade -> hypotension - 5-HT2A receptor blockade -> weight gain, sedation and hypotension - H1 antihistamine blockade -> weight gain, sedation and hypotension How could the extra-pyramidal side effects be managed? Prompt: What about acute EP side effects? What about chronic EP side effects? - Switch to an atypical drug (lower incidence of extra-pyramidal effects) - Administer benztropine or diazepam - No effective treatment for tardive dyskinesia: prevention vital; monitor for early signs and reduce or cease anti-psychotic asap Note: - Tardive dyskinesia is characterized by repetitive, involuntary, purposeless movements - Likely results primarily from neuroleptic-induced dopamine supersensitivity in the nigrostriatal pathway, with the D2 dopamine receptor being most affected 2010-2 Describe the general pharmacokinetic characteristics of antipsychotic drugs - Most are readily but incompletely absorbed - Many undergo significant first pass metabolism – less systemic availability - Most are lipid soluble (lipophilic) - Most have high PPB (92-99%) - Most are completely metabolised by hepatic enzymes (oxidation; demethylation) These are catalysed by liver enzymes. Define the term “atypical” antipsychotic and provide an example. - Newer antipsychotic agents with less propensity to cause extra- pyramidal side-effects - Better at treating negative features of schizophrenia - Greater ability to alter 5-HT2A receptor activity than to interfere with D2-receptor action Examples: olanzapine, clozapine, quetiapine, risperidone, loxapine Describe the adverse drug reactions to olanzapine. - Weight gain (increased lipis, risk of diabetes mellitus) - Sedation (but less than typical antipsychotics) - Minor orthostatic hypotension - Minor anticholinergic effects (dry mouth, urine retention etc) - Extrapyramidal effects less prominent than with typical antipsychotics 2007-1, 2006-1 What the pharmacological characteristics of olanzepine? - Atypical antipsychotic - Thienobenzodiazepine - Most 5-HT2A and D4 receptor effects, also alpha-1 and H1 effect - High potency - Very low extrapyramidal effects - Medium sedative - Low hypotensive effects - Causes weight gain long term (may precipitate diabetes) How does it differ from haloperidol? - Typical antipsychotic - Butyrophenone - Most D2 receptor effects - High potency - Very high extrapyramidal effects - Low sedative - Low hypotensive effects - Cheap What are the clinical conditions Olanzapine is prescribed for? 2006-1 Wide Spectrum of use: - Schizophrenia - Acute treatment of mania - Behavioural emergencies - Autism spectrum disorders - Delirium: mood and behavioural disturbances, palliative care, AIDS - Dementia: General, Sleep disorder in patients with dementia (palliative care) 4.6 Antidepressives 2008-1 How do anti-depressants exert their action? Thought to enhance amine-dependent synaptic transmission (serotonin and noradrenalin) by: 1. Inhibition of metabolism within nerve terminal (MAOIs) 2. Inhibition of reuptake from synapse (TCAs, SSRIs) 3. Increased release due to antagonism of specific serotonin and 2 NA receptors (Mirtazapine) What are the relative advantages of different classes of antidepressants? (Adverse effects?) Drug Adverse effects Overdose risk Interactions SSRI GI, libido, insomnia, headaches Low CYP2D6 inhibition -> TCA Serotonin syndrome w/ MAOIs SNRI Same as SSRIs + noradrenergic: Low but Fewer interactions c.f. SSRIs Venlafaxine –> BP, HR, insomnia, agitation cardiotoxic TCA Anticholinergic (antimuscurinic) Lethal arrhythmias, Increased TCA levels w/ hypotension, CYP2D6 inhibition and slow -blocking -> BP metabolisers, interactions w/ H1 block -> weight and sedation seizures BP meds -> hypotension Class 1A -> arrhythmogenic MAOI Orthostatic hypotension Autonomic instability, Serotonin syndrome Weight gain hyperadrenergic, Dietary tyramine, SNS drugs -> Sexual dysfunction psychosis, seizures BP, CVA, MI (via NA effects) Sample viva, 2006-2 What are the medical uses for St Johns Wort? - St John's wort is widely known as an herbal treatment for depression - Cochrane review states: a) Superior to placebo in patients with major depression b) Similarly effective as standard antidepressants c) Fewer side-effects than standard antidepressants - However poor repeatability and effects greater in German trials What are its important drug interactions? - Kinetic as a CYP inducer (decrease drug effect) Subtherapeutic digoxin Birth control pill -> pregnancy Warfarin Anticonvulsants - Dynamic b/c inhibits catecholamine reuptake (potentiates some drug effects) Serotonin syndrome or MAO crisis Additional: Serotonin syndrome - Life-threatening serotonin poisoning - Classically a clinical triad 1. Cognitive effects: headache, agitation, hypomania, confusion, hallucinations, coma 2. Autonomic effects: shivering, sweating, hyperthermia, hypertension, tachycardia, nausea, diarrhoea 3. Somatic effect: myoclonus, hypereflexia, tremor 4.6.1 Tricyclics (1) 2011-2 What are the pharmacokinetics of tricyclic anti-depressants? - Oral, well-absorbed - High first pass metabolism so bioavailability ~50% - Long half-time (once daily dosing, usually nocte b/c sedating) - High tissue protein binding - High lipid solubility - Large Vd - Metabolised in liver by CYP2D6, active metabolites - Only 5% unchanged in urine What are the toxic effects of tricyclics in overdose? 2011-2, 2008-2 - Anticholinergic (antimuscurinic) -> Dry mouth, blurred vision, constipation, urinary retention, confusion, tachycardia - -blocking -> Hypotension - H1 block -> Sedation - Class 1A -> Arrhythmogenic sodium channel blockade w/ QT prolongation, reduced contractility - Seizures, psychosis, agitation - Sympathomemetic -> tremor, insomnia What drugs could be used in the treatment of tricyclic toxicity in overdose? - Supportive: dopamine/NA for hypotension - Cardiac toxicity: sodium bicarbonate 50-100 mEq IV (unblocking drug from Na channels) - Intralipid: binding of drug due to lipophilic profile, decreased available drug 2008-2 What is the mechanism of action of the tricyclic antidepressants? Prompt: Name one amine? - Block amine (noradrenaline and serotonin) reuptake pumps at presynaptic nerve endings - Prolongs duration of action of neurotransmitters at postsynaptic receptors - Most non selective 4.6.2 Serotonin re-uptake inhibitors (2) 2008-2 What is the mechanism of action of the SSRI drugs - Monoamine hypothesis of depression: that depression is caused by deficiency or imbalances in the monoamine neurotransmitters (5-HT, NE and DA) - Selective binding to serotonin transporter (SERT) leading to 80% reduction in activity and reuptake inhibition - High synaptic serotonin levels leads to downregulation of autoreceptors (presynaptic), downregulation of postsynaptic 5-HT2A receptors - Depressed and suicidal patients have shown higher levels of 5-HT2A, suggesting overactivity - These (slowly proceeding) neurophysiological adaptations of the brain tissue are the reason why usually several weeks of continuous SSRI use is necessary for the antidepressant effect to become fully manifested and why increased anxiety is a common side effect in the first few days or weeks of use What receptor/channel effects lead to the SSRI side effect profile. Prompt why are SSRIs safer than TCAs? - SSRIs very SERT specific - Serotonin syndrome/ restlessness/ GI upset - Minimal autonomic effects ( adrenoceptors, noradrenaline reuptake transporter/NET) - Only mild muscarinic / Na channel, H1 block effects - Well tolerated and low risk in overdose 4.6.3 Newer agents (2) 4.6.4 Lithium (1) 2010-2, 2005-2 Describe the pharmacokinetics of lithium - Absorption: Complete in 6-8 hours, peak concentration 0.5-2h, 100% bioavailability - Metabolism: none - Protein binding: none - Vd: In total body water w/ slow entry to intracellular compartment and some into bone – 55L/70kg - Excretion: 95% in urine w/ clearance 20% of Cr - t½ about 20 hours - Steady state plasma concentration takes 5-7 days What are the adverse effects of Lithium at therapeutic levels? - May be associated with therapy or toxicity: 1. Neurologic: Tremor (common), motor hyperactivity, ataxia, dysarthria, aphasia 2. Psychiatric: Confusion, withdrawal 3. Thyroid: Hypothyroidism 4. Renal: Polydipsia and Polyuria (common), nephrogenic diabetes insipidus (inhibits the effect of ADH on the DT cells) 5. Oedema (Na retention) and weight gain 6. Acne and psoriasis 7. Leukocytosis (may be beneficial) What are the signs/symptoms of lithium toxicity? - CNS: Tremors, confusion, slurred speech, ataxia, drowsiness, blurred vision, seizures - GIT: Vomiting Note: Therapeutic overdoses are more common than intentional, often caused by a change in the patient’s status e.g. diuretic use, decreased serum sodium, fluctuating renal function 2005-2 What factors may influence lithium excretion? 1. Renal function (Glomerular filtration rate) 2. Water and sodium status (increased lithium reabsorption in proximal tubule in sodium or water depleted states) 3. Drugs: thiazide diuretics and NSAIDs reduce clearance 4. Lithium serum concentration Additional: Pharmacodynamics of lithium - Used as a mood stabiliser in bipolar affective disorder, and sometimes as an adjunct in depression and schizophrenia - Poorly understood mechanism - Closely related to sodium, inhibiting it’s transport across cell membranes - Effects on second messengers, notably inhibiting inositol monophosphatase (IMPase) and other enzymes, reducing IP2 -> IP1 -> inositol and ultimately PIP2 (the precursor of IP3 and DAG) 4.7 Anticonvulsants 4.7.1 Phenytoin (1) 2010-2, 2008-2 Describe the pharmacokinetics of phenytoin. - Weak acid pKa 8.3 - Oral absorption almost complete 90%, but slow and variable with peak serum conc. 3- 12hrs - IMI: unpredictable and incomplete absorption with drug precipitation in the muscle - Highly plasma protein bound - Vd 45L/70kg - Saturable hepatic metabolism leading to dose dependant (zero order) kinetics (metabolised to inactive metabolities) - Variable t½ of 7-42hrs (average 24 hours) - Takes 5-7 days to reach steady state with low dosage, 4-6weeks with high - Urinary excretion, < 2% unchanged in urine - Drug interactions via plasma protein binding or via enzyme induction (CYP2C19 & CYP2C9) - Therapeutic level 10-20mg/L Describe the pharmacodynamics of phenytoin? 2008-2 1. Blocks sodium channels - Inhibits the generation of repetitive APs - Preferential binding to & prolongation of the inactivated state of the Na channel (use-dependant effect on Na conductance) 2. Other electrolyte effects - Alters K+ conductance - Alters Ca2+ conductance and decreases Ca2+ permeability, inhibits Ca2+ influx therefore affecting neurotransmitter and hormone release - Interacts with membrane lipids ?stabilising membranes - Paradoxical excitation in some neurones - Alters membrane potentials and the conc. of amino acids - Affects neurotransmitters NA, Ach & GABA - High conc inhibits serotonin and NA release, promotes uptake of DA & inhibits MAO activity What are the adverse effects of phenytoin? 2010-2, 2010-1 - Dose related neurotoxic effects: Diplopia and ataxia (most common), nystagmus, drowsiness, hallucinations, slurred speech, confusion - Long term: Hirsuitism, gingival hyperplasia & overgrowth with bleeding, acne, facial coarsening - Idiosyncratic: Skin rash, SJ syndrome, lymphadenopathy, agranulocytosis - Rapid IV administration associated with CV collapse (hypotension and arrhythmias) - Alters TFT results (binding to thyroid globulins, TSH is still useful test) - Drug interactions (plasma binding), also reduced Cl and binding in neonates - Teratogenic -> foetal hydantoin syndrome (IUGR, microcephaly, developmental delay) Describe how phenytoin is administered in status epilepticus 2010-1 - IV load 13-20mg/kg - Given diluted in saline (precipitates in glucose) - Max rate in adults of 50mg/min - Continued 100mg Q6-8hrly 4.7.2 Carbamazepine (1) 2009-1, 2005-1 Describe the mechanism of action of carbamazepine - Tricyclic compound with structural similarities to phenytoin and anticonvulsant properties: - Like phenytoin blocks Na+ channels -> inhibits high-frequency repetitive firing of neurones - Also presynaptic blocker of synaptic transmission - Inhibits uptake and release of noradrenaline from brain synapses - Does not influence GABA uptake Additional: Pharmacokinetics of carbamazepine - Well absorbed - Peak levels 6-8 hours - 70% protein bound (but does not displace other drugs) - Vd 100L/70kg - Half life 36hr after single dose, 15h on continuous therapy - Induces liver enzymes and dose has to increase markedly over first few weeks How is carbamazepine metabolised and what is the effect of the metabolism of other drugs - Metabolised by microsomal enzymes -> active metabolites (clinical significance uncertain) - Enzyme induction increases rate of metabolism of other drugs e.g. phenytoin, valproate, clonazepam - Some of these drugs also can inhibit carbamazepine metabolism (valproate) - Phenytoin and phenobarbital may induce the metabolism and decrease levels of carbamazepine What are the clinical indications for its use? - Partial tonic-clonic seizures - With phenytoin if difficult to control tonic-clonic seizures - Trigeminal neuralgia and other pain syndromes - Some patients with bipolar What are its potential adverse effects? - Commonly: diplopia, ataxia - Dose-related: GIT upset, ataxia, drowsiness, hyponatraemia - Idiosyncratic: Blood dyscrasias - aplastic anaemia, agranulocytosis (needs monitoring) - Skin rash - Alters clearance of other drugs w/ drug reactions due to induction of liver enzymes 4.7.3 Sodium valproate (1) 2011-2, 2005-1 What are the proposed mechanisms of action of valproate? 1. Blocks Na+ channels thereby blocking sustained high frequency firing of neurones 2. Blockade of NMDA receptor mediated excitation 3. Increases GABA levels Describe the toxic effects of valproate? - Commonly: GI upset w/ nausea and vomiting (dose related, start gradually) - Idiosyncratic hepatotoxicity: Mostly within 4 months of initiation of treatment, treat with intravenous L-carnitine, requires monitoring of LFTs - Others: Tremor, weight gain, appetite, sedation, allergy - Teratogenic: Increased malformations (spina bifida, cardiac) in pregnancy What interactions does valproate have with other anti-seizure drugs? - Phenytoin: inhibits metabolism and displaces from plasma proteins - Phenobarbitore & carbamazapine induce metabolism - Lamotrigine decreases clearance 4.7.4 Newer agents (3) 4.8 Hypnotics / sedatives 4.8.1 Benzodiazepines (1) 2011-2 What benzodiazepines are commonly used in the ED? - Diazepam, lorazepam, midazolam, clonazepam, temazepam, 2011-2, 2005-2, 2007-2 (clonazepam), 2007-1 & 2004-2 (midazolam) What is the mechanism of action of benzodiazepines? - Facilitates GABA binding at GABAA receptor (ligand-gated chloride channel) - Thus GABA inhibition enhanced through hyperpolarisation - Acts throughout brain but the distribution in CNS of the different GABAA receptor isoforms varies - Binding between 1 & 2 subunit (modulatory BZ site) – more selective than barbituates - Low affinity for GABAB What are the clinical effects of benzodiazepines? 1. Sedation and anxiolysis 2. Hypnosis (sleep inducing) - Reduced sleep latency (time to fall asleep) - Increase stage 2 NREM - Decrease REM and stage 4 NREM 3. Anaesthesia (adjunct) 4. Anticonvulsant (potentiates inhibitory interneurones) 5. Muscle relaxation 6. Cardiorespiratory depression - Especially if respiratory or cardiovascular disease - Decreased contractility and vasomotor tone in toxic doses -> cardiovascular collapse 2010-2 What are the indications for benzodiazepine use? - Anxiety disorders - Preoperative medication - Insomnia and sleep disturbances - Seizure disorders - Panic disorder - Alcohol withdrawal - Muscle spasm - Induce amnesia during cardioversion/endoscopic procedures Explain the rationale for use of benzodiazepines in alcohol withdrawal - Down-regulation of neuro-inhibitory GABA receptors in alcohol dependent individual leads to symptoms of GABA deficiency in withdrawal (anxiety -> seizures) - BZD act at a modulatory site on the GABAA receptor to facilitate GABA binding to the GABAA receptors, enhance chloride channel opening, and overcome neuroexcitatory symptoms of GABA deficiency 2007-2 What properties make clonazepam an effective anticonvulsant? - Lipid soluble so croses the blood brain barrier - Acts on alpha I GABA receptor isoform -> potentiates inhibitory interneurones 2007-1 What are the pharmacokinetics of Midazolam? - Water soluble hence oral/IM/intranasal but crosses BB barrier easily at body pH - Short elimination half-life 2-4 hours - 56% renal excretion 2010-2 What is the mechanism of action of flumazenil? - Competitive antagonist at the BZD binding site on the GABAA receptor - Decreases the binding of GABA - Blocks GABA-induced increase in Cl- permeability and influx of Cl- into the cell causing hyperpolarisation and decreased excitability of the neuron What are the indications for flumazenil use - Avoid intubation or ICU admission in BZD overdose - Reverse BZD sedation after procedures - Diagnostic role 2007-1 2005-2, 2004-2 What potential problems should be anticipated when using flumazenil? - Precipitate seizures in mixed overdoses with BZD and proconvulsants (TCAs) - Precipitate seizures in patients taking BZD to control epilepsy - Precipitate withdrawal symptoms and seizures in BDZ-dependence - Duration of action is only 1-3hrs thus repeated administration may be necessary - Reversal of BZD-induced respiratory depression has not been demonstrated, so respiratory and cardiovascular support may be required - Adverse Effects: headache, visual disturbance, increased anxiety, nausea, light-headedness 4.8.2 Barbiturates (1) 4.8.3 Newer agents (3) 4.9 Ethanol (1) Pharmacokinetics - Small water soluble molecule, rapidly absorbed from stomach - Peak blood alcohol reached in 30mins - Vd approximates TBW (0.5-0.7L/kg) - Higher levels reached in women b/c lower TBW and less GI ADH metabolism - 90% oxidized in the liver, the remainder excreted via lungs and kidneys - Zero order kinetics – i.e. fixed clearance amount (not related to time or concentration) of about 1drink/hour - 2 major pathways, 3rd final common pathway: Alcohol Dehydrogenase (ADH) - EtOH –(ADH)-> Acetaldehyde - Requires NAD+ -> NADH (lactic acidosis and hypoglycaemia in acute toxicity) - Inhibited by fomepizole Microsomal Ethanol Oxidizing System (MEOS) - Utilises NADPH - Activates at higher levels (when ADH system saturated b/c depletion of NAD) - Induced in chronic alcoholism (generation of toxic fee radicals) Acetaldehyde Metabolism - Acetaldehde –(aldehyde dehydrogenase, ALDH)-> Acetate - Inhibited by disulfiriam (and metronidazole, trimethoprim) or may be genetic underactivity - Accumulation of acetaldehyde -> facial flushing, nausea, vomiting, headache Pharmacodynamics 1. CNS - Effects many receptors in signaling pathways, esp: enhances action of GABA (inhibitory) at GABAA and inhibits glutamate (excitatiory) opening NMDA receptor (learning and memory) - Sedation, anxiolytic -> impaired motor function, slurred speech, ataxia -> emesis, stupor -> coma -> respiratory depression and death (>500mg/dL) 2. Cardiac – reduced contractility 3. SMC – vasodilator (via CNS and direct effects of acetaldehyde) Chronic consumption 1. Liver and GI - Fatty liver -> hepatitis -> cirrhosis -> failure - Pancreatitis - Small bowel damage – malabsorption of nutrients and vitamins 2. Nervous system - Tolerance and dependence (delirium tremens) - Neurotoxicity (peripheral neuropathy, B12 deficiency -> Wernicke’s encephalopathy) 3. Cardiovascular - Cardiomyopathy - Arrythmias - HTN - CVD 4. Haematologic 5. Endocrine 6. Fetal alcohol syndrome 7. Immune 8. Cancer risk 2005-1 Describe the metabolism of methanol. - Oxidation via ADH to formaldyhyde, formic acid and CO2 ADH inhibited by fomepizole, and EtOH has higher affinity Toxicity due to the metabolites, especially formic acid Folic acid dependent pathway Leads to metabolic acidosis w/ elevated anion and osmolar gap Key symptoms is visual “like being in a snowstorm” What specific modalities of treatment are available for the treatment of severe methanol poisoning? Common treatment: Support of respiration 1. Suppression of metabolism (EtOH or formepizole) 2. Removal w/ haemodialysis 3. Alkalinisation Also: Formic acid to prevent formic acid accumulation 2010-2 Explain the rationale for use of benzodiazepines in alcohol withdrawal - Down-regulation of neuro-inhibitory GABA receptors in alcohol dependent individual leads to symptoms of GABA deficiency in withdrawal (anxiety -> seizures) - BZD act at a modulatory site on the GABAA receptor to facilitate GABA binding to the GABAA receptors, enhance chloride channel opening, and overcome neuroexcitatory symptoms of GABA deficiency 4.10 Anti-parkinsonian agents (3) 2007-2 Why is levodopa used in combination with carbidopa? - Carbidopa is a peripheral dopa decarboxylase inhibitor - Because it doesn't penetrate the blood brain barrier, it reduces the peripheral metabolism of levodopa => increased levodopa levels and increased half-life resulting in more dopa being available for entry into brain to exert its effects. What are the adverse affects of levodopa? - GIT: Anorexia, nausea and vomiting in up to 80% of patients. Due to stimulation of emetic centre in brainstem Incidence I, to < 20% if a peripheral decarboxylase inhibitor is added. - CVS: Arrhythmias-tachycardia, ventricular ectopics, AF. Due to increased catecholamine formation peripherally. Postural hypotension - Dyskinesias: Up to 80% of those receiving levodopa for long periods. - Behavioural effects: Depression, anxiety, agitation, insomnia, nightmares, euphoria and mood changes. More common if taking a levodopa with a decarboxylase inhibitor. Due to higher levels presenting to the brain. - Fluctuations in clinical response occurs with increasing frequency as treatment continues. - Miscellaneous: Mydriasis, acute glaucoma, Coombs positive haemolytic anaemia, gout, abnormalities of taste and smell, Brownish discolouration of saliva, urine or vaginal secretions, priapism, abn urea, LFTs. - Drug Interactions: Pyridoxine enhances metabolism of levodopa. Hence effect drecreased. 4.11 Anti-migraine agents (2) 2011-1 What drugs can be used in the treatment of an acute attack of migraine? - Simple analgesia (eg paracetamol, aspirin, codeine) - Metoclopramide - Prochlorperazine - Ergot alkaloids eg ergotamine (+/- caffeine added) - Chlorpromazine - Triptans e.gg sumatriptan - Opoids can be used but not treatment of choice How do triptans work? - Structural analogue of 5-HT - Selective agonists at 5-HT1 receptors - These receptors are found on cerebral & meningeal vessels - Causes vasoconstriction Chlorpromazine can be used to treat acute migraine. What are the major side effects of chlorpromazine? - Hypotension - Sedation - Anticholinergic (dry mouth, dry eyes, urinary retention, constipation) - Extrapyramidal (eg acute dystonia) - Pain with IM injections, risk of muscle necrosis 2005-2 Please describe the pharmacokinetics of Sumatriptan - Bioavailability 15% (other agents in the group have availabilities of 40- 70%) - t½ 2-3 hours - Given S/C, nasally, orally - Poor bio-availability given s/c What are the pros and cons in using Sumatriptan for migraine? Pros: - Mild side effect eg tingling, dizziness, muscle weakness, neck pain, injection site reactions - Effective Cons: - Contraindicated in patients with IHD due to coronary spasm - Short duration of action (several doses required for prolonged attack) - Very expensive