Psychosocial Factors and CHD - Heart Disease Prevention Program
advertisement
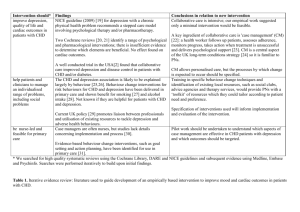
Psychosocial Risk Factors and Behavioral Interventions in Cardiovascular Disease Nathan D. Wong, PhD, FACC, FAHA Professor and Director Heart Disease Prevention Program Division of Cardiology, University of California, Irvine, CA USA President, American Society for Preventive Cardiology “ For every affection of the mind that is attended with either pain or pleasure, hope or fear, is the cause of an agitation whose influence extends to the heart, and there induces change from the natural constitution,in the temperature, the pulse and the rest” - Dr William Harvey, 1962 The term “Psychosocial” broadly categorizes factors which are: • Psychologic – e.g, anxiety, depression • Psychosocial – e.g., work stress, discrimination, emotional support • Social-structural – e.g., socioeconomic status, social integration, neighborhood effects Source: Rozanski A, Chap 34, Preventive Cardiology, Blumenthal, Foody, Wong, eds. Proposed Mechanisms Relating Chronic Stress to Atherosclerosis Rozanski et al., JACC 2005 Six Reasons that Promote Interest in Evaluation and Management of Psychosocial Stress in Heart Disease Rozanski et al., JACC 2005 INTERHEART Study: Psychosocial Index and Risk of Acute MI Psychosocial index based on individual items of depression, locus of control, work or home stress, financial stress, and adverse life events. Yusuf, Lancet 2004 Depression • Estimated prevalence of major depression in the US is 14%, but up to 30% in cardiac patients • Characterized by a depressed mood and combination of other symptoms such as weight change, sleep disturbance, insomnia, fatigue, feelings of guilt, worthlessness, and/or hopelessness. • Depression can stimulate the autonomic nervous system and HPA axis. It is also proinflammatory and is associated with increases in CRP, fibrinogen, IL-6 and other inflammatory measures, independent of BMI and other risk factors. • Of all psychosocial factors, evidence of association with CVD is strongest for depression. Depression: Evaluation • Measurement can be done by: – Beck Depression Invetory – Center for Epidemiologic Studies Depression Scale (CES-D) – Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) Major depression according to DSM-IV criteria indicates the presence of severely depressed mood and/or inability to take pleasure in all or most things that were previously considered enjoyable, lasting 2 weeks or longer and accompanied by functional impairment and somatic complaints, such as fatigue or loss of energy nearly every day, insomnia or hypersomnia, change in appetite, diminished ability to concentrate, feelings or worthlessness or inappropriate guilt, and recurrent thoughts of death or suicidal ideation Depression and CVD (cont) • Frasure-Smith et al (JAMA 1993) reported a 4-fold increase in mortality during 6 months following acute MI from depression in cardiac patients. • Meta-analysis examining depression as a factor in development of CHD in healthy individuals showed a risk factor-adjusted RR=2.69 for CHD incidence ( Rugulies, Am J Prev Med 2002). Depressive Symptoms and Cardiac Free Survival in Post-MI Patients Lesperance et al. Circulation 2002 Depression and CHD Depression and Brachial FMD Anxiety and CHD • Anxiety is characterized by heightened levels of perceived fear and nervousness– may include panic disorder, social phobia, obsessive-compulsive disorder, acute stress disorder, posttraumatic stress disorder. • Clear relation to sudden cardiac death in a dosedependent fashion • 32-year follow-up of men in the Normative Aging Study who reported two or more phobic anxiety symptoms had a 3.2-fold increased risk of fatal CHD and 5.7-fold increased risk of sudden death. • Ventricular arrhythmia may be the underlying mechanism since no relation seen between anxiety and MI. Anxious individuals also have reduced heart rate variability. • Some population surveys show prevalence to be approximately 20% Post Traumatic Stress Disorder (PTSD) • Present if after exposure of an inciting traumatic event the subject report re-experiencing the event, hyperarousal, and avoidance of traumatic reminders and emotional numbing. • A retrospective study of men who have served in the military shows a stepwise relation between symptoms of PTSD and nonfatal MI and cardiac death (Kubzansky, Gen Psychiat 2007). • Study of 1059 women shows relation between PTSD and incident CHD (Kubzansky, Health Psychol 2009). • Boscarino evaluated 4328 men who served in Vietnam war; PTSD associated with more than a two-fold increased risk of subsequent cardiac mortality, independent of depression symptoms (Psychosom Med 2008). Source: Rozanski A, Chap 34, Preventive Cardiology, Blumenthal, Foody, Wong, eds. Pessimism and Optimism • Optimists tend to see negative events as temporary and positive events are more permanent; negative events are attributed to external causes rather than self-condemnation. • Pessimists have an opposite explanatory style to events. • One study of 7216 subjects showed the extent of pessimism to be directly related to the risk of all-cause mortality (Grodbardt, Psychosom Med 2009) • In the largest such study, the Women’s Health Initiative showed among 97,253 women that those those who were optimistic had a 30% lower rate of cardiac mortality (Tindle, Circulation 2009) Pessimism vs. Optimism and Cardiac Events Personality Constructs: Type A Behavior Pattern • The Type A behavior pattern includes a harddriving, time-patient, and hostile behavior. • Friedman and Rosenman showed the Type A Behavior Pattern to be related to both CAD risk and recurrent MI; however subsequent studies showed no relationship, so this has been of diminished interest. • The Recurrent Coronary Prevention Project did show intervention from counselling on Type A behavior to reduce recurrent MI rates and cardiac deaths (Friedman et al., Am Heart J 1986) Hostility • Reflects emotional (anger, contempt), behavioral (verbal and physical aggression), and cognitive (cynicism, mistrust) factors. • Predicts incident CHD in healthy individuals, even after risk factor adjustment (Niaura et al.. Health Psychol 2002). • Hostility is associated with heightened cardiovascular reactivity and higher blood pressure. • Higher prevalence in those with lower SES; has been suggested as a mechanism linking low SES with CVD outcomes. • May be a stronger indicator of incident CHD than of recurrent CHD or its progression. Social Relations • Vast literature on social networks, social support, and CVD • Alameda County Study showed those who lacked ties to others (index of contacts with friends and relative, marital status, and church membership) were 1.9-3.1 times more likely to die over 9 years, including from ischemic heart disease and other causes. • A large study in Tecumseh, Michigan found a strong positive association in men, but not women between social support and mortality,. Even after adjustment for other risk factors. • US Physicians Study showed socially isolated men had a 1.8-fold significantly greater risk of fatal CHD in multivariable analysis/. Social Support and Mortality Marriage Satisfaction and Carotid Plaque Presence and Progression Positive Emotions and Well-Being • Recent research has focused on positive psychological factors. • Positive emotions have been defined to include happiness and states of being that reflect a positive engagement with the environment such as curiosity and interest. • This gives the individual increased ability to cope with stress. • Metaanalyses involving 70 studies shows positive wellbeing to be associated with lower mortality (Chida, Psychosom Med 2008). • A study of 1238 elderly persons showed those who identified with a higher purpose in life had a 40% lower risk of mortality over 2.7 years (Boyle, Psychosom Med 2009). Laughter, Mental Stress and effects on Brachial Reactivity Purpose in Life and Mortality Low Purpose Job Strain and CHD • Falk et al (Am J Pub Health 1992) showed job strain to be associated with a 2-fold increase in mortality; this was amplified when accompanied with poor social networks. • Other studies have shown a higher prevalence of MI in those with increased job strain, and higher job control to be associated with a lower prevalence of hypertension. • Some studies have shown no relation of job demands or strain with hypertension or elevated blood pressure. Effort-Reward Imbalance (ERI) • This construct argues that risk is increased when workplace effort is not commensurate with tangible—eg salary or intangible—support rewards. • Prospective studies show ERI predicts CVD incidence, even after adjustment for other risk factors. Conceptual Models of Work Stress Effects of Psychosocial Intervention • General effects of psychosocial interventions have been modest. • A metaanalysis of 36 studies involving 12,851 patients showed only a slight reduction in non-fatal MI and no reduction in cardiac mortality; however, many studies often had a negligible improvement in anxiety or depression (Ross, Cochane Database Syst Rev 2009). • However, in the cardiac rehab setting, a metaanalysis of 23 randomized trials showed all-cause mortality to be 28% lower in those trials that included psychosocial interventions compared to those who did not (Linden, Eur Heart J 2007), but reduction in mortality seen only in those who effectively reduced psychological distress. From Rozanski A, Chap. 34 Preventive Cardiology, Blumenthal, Foody, Wong, eds. Intervening on Depression: ENRICHD Trial (Berkman LF et al., JAMA 2003) • Enhancing Recovery in Coronary Heart Disease (ENRICHD) study was a multicenter randomized clinical trial of 2,481 post-MI patients • Subjects met criteria DSM-IV criteria for major depression, minor depression with hx of major depression, or met certain criteria on a social support instrument. • Primary endpoint of cardiovascular mortality and non-fatal recurrent MI • Intervention involved 6 group sessions of cognitive behavioral therapy over 6 months, followed by open group membership, with SSRI use also allowed for unremitting or severe depression in both groups. ENRICHD (cont.) • Intervention did not increase event-free survival after 29 months (75.8% vs/ 75.9%). Also no differences in mortality or infarction in any of the subgroups (e.g. those isolated and depressed). • There were, however, significant improvements in depression and social support effected by the intervention. • Lack of overall benefit may be due to improvements in depression and social support that also occurred in the usual care group, as well as high SSRI use in both groups. • A follow-up analysis showed that those who responded with a reduction in depression had a reduction in late mortality. Intervention Trials on Stress • Based on the Ischemic Heart Disease Life Stress Monitoring Program, involving 461 male pts recovering from MI randomized to a stress monitoring intervention vs. usual care. Intervention involved home nursing interventions, individually tailored involving education, support, collaborative problem solving, and referral. • After 1 year, risk of death due to cardiac causes was reduced in half, and after 7 years differences still persisted (Fraser-Smith et al, Psychosom Med 1985 and 1989). Intervention Trials (cont.) • Montreal Heart Attack Readjustment Trial involved treatment of life stress in a larger cohort of 1376 men and women post-MI, but showed no benefit, and in fact a significant increase in cardiac and all-cause mortality among women in the intervention group (Fraser-Smith et al., The Lancet 1997). • Those responding to the support intervention within two home visits had improved outcomes, compared to those who continued to display high levels of distress. Rozanski et al., ACC Review on Psychosocial Factors and CHD, JACC 2005 Stepped Collaborative Approach for Managing Psychosocial Stress Rozanski et al., JACC 2005 Screening for Psychosocial Risk: AHA Science Advisory on Depression (Lichtman J et al. Circulation 2008) • The recommendations, which are endorsed by the American Psychiatric Association, include: – early and repeated screening for depression in heart patients – the use of two questions to screen patients – if depression is suspected the remaining questions are asked (9 questions total) – coordinated follow-up for both heart disease and depressive symptoms in patients who have both. From: Lichtman J et al., Circulation 2008 Lichtman J et al., Circulation 2008 AHA Science Advisory on Depression: Other Recommendations • Evaluation by a professional qualified in diagnosing and managing depression • Screening for other psychiatric disorders. • Treatments include cognitive behavioral therapy, physical activity, cardiac rehabilitation, and/or antidepressant drugs. • Selective serotonin reupake inhibitor (SSRI) treatment may be effective for treating depression. Studies show mixed findings in relation to cardiac events and mortality. • Routine screening should be done in multiple settings, including the hospital, physician’s office, clinic and cardiac rehabilitation center to avoid missing the opportunity to effectively treat depression. • Coordination of care between health providers is essential for patients with combined medical and psychiatric diagnoses. Lichtman J et al., Circulation 2008 From Rozanski A, Chap. 34 Preventive Cardiology, Blumenthal, Foody, Wong, eds. Steps to Promote Effective Adherence to Behavioral Suggestions (cont.) From Rozanski A, Chap. 34 Preventive Cardiology, Blumenthal, Foody, Wong, eds. Summary • Evidence of associations between a number of psychosocial factors--including depression, anxiety, hostility, social networks and support, and occupational stress with cardiovascular disease. • Adverse psychosocial characteristics to cluster with traditional biological and behavioral risk factors • The highest levels of psychosocial risk are generally found among the socially disadvantaged. From Bennett and Berkman, Preventive Cardiology 2005 Summary (cont.) • Results of large-scale clinical trials of psychosocial interventions have been mixed with respect to their impact on CVD outcomes. • Screening of certain psychosocial factors, especially depression, is recommended in the primary and secondary prevention setting. • Greater consideration of psychosocial influences on cardiovascular outcomes and behavioral risk factors may enhance clinical efforts to improve both primary and secondary prevention outcomes.