Community paramedic presentation
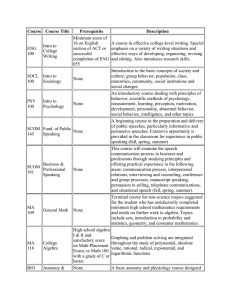
advertisement
I Am Worried. Can you Send Someone to See My Mom? Kristofer Smith, MD, VP Jonathan Washko, AVP Asantewaa Poku, Clinical Data Analyst Elizabeth Quellhorst, Administrative Manager Session Code A25, B25 Presenters have nothing to disclose 1 Session Objectives • Identify the key operational strategies necessary to build programs to keep high-risk frail elderly from going to the emergency room • Review lessons learned from a collaboration between an advanced illness management program and a community paramedicine program aimed at reducing admission rates for the high-risk frail elderly in the community • Understand how to ensure the financial viability of clinical collaboratives focused on high-risk patients by taking advantage of health care reform and/or partnering with insurance companies 2 Problem Statement • Seniors with multiple chronic conditions in an advanced state with functional impairment have frequent deteriorations in health status which requires meaningful 24x7 clinical responses. • These high risk, high cost populations have extreme difficulty getting to traditional outpatient services and therefore rely heavily on emergency department and hospital care. • Interrupting this cycle through at home clinical support programs could alleviate suffering, improve quality and decrease cost. 3 Advanced Illness Management – House Calls Program Background Complex medical management for more than 1,000 patients in Queens, Nassau, and Suffolk counties with multiple chronic conditions and functional impairment • Interdisciplinary care teams, which include physicians, nurse practitioners, social workers, and medical coordinators deliver primary and palliative care in the patient’s home in an effort to: – – – – – – Understand wishes of the patient and family (advance care planning) Maintain or improve functional status Reduce unnecessary utilization or unwanted care Increase days at home Allow for death with dignity at home Care for the whole person: social work and care coordination 5 Advanced Illness Management – House Calls Program Background House Calls Patients, N= 1071 Age 110 Oldest 84 Average 21 Youngest 69% Female 31% Male = 10 patients Nassau, Suffolk and Queens counties * November 2014 Census Advanced Illness Management – House Calls Program Background House Calls Stats* * November 2014 Census Program Background • Established in 1993, providing air and ground BLS, ALS, SCT, CCT and 911 services • 600+ Emergency Medical Technicians and Paramedics • Largest health system based ambulance service in New York Metropolitan area and one of the largest in the United States • Duly accredited by the Commission on Accreditation of Ambulance Services (CAAS) and the National/International Academics of Emergency Dispatch, Accredited Center of Excellence (ACE) 8 Program Background • Over 110 available response units across New York City, Nassau, and Suffolk • More than 135,000 requests for service per year • 24x7x365 Fault tolerant services • Advanced Medical Priority Dispatch System with Dispatch Life Support • Clinician answers every call utilizing call prioritization & triage system • All ALS system operates under a High Performance EMS operations model • Reliable, clinically appropriate response time 9 Unique, Innovative & Integrated Solution • Comprehensive Mobile Integrated Healthcare / Community Paramedicine Program • Telemedicine • Centralized Command and Control System • Integrated into EMS System as a Clinical Safety Net • Advanced Analytics • Integrated Quality Assurance / Improvement 10 Key Mobile Integrated Healthcare Community Paramedicine Program Elements • MIH Framework – Regulatory Approach – Specialized Training – Specialized Equipment • EMS Operations – – – – – Command and Control Call Center Integration High Performance EMS Marginal vs. Specialized Approach IT Systems Integration • Clinical – – – – Telemedicine, On Line Medical Control Formulary, Diagnostics & Treatment Modalities Death at Home with Dignity Quality Assurance / Improvement 12 Mobile Integrated Healthcare Community Paramedicine Program Non-Transport Solution Options Diagnostics Treatments Formulary Expanded Physical Assessment Basic Airway Management Magnesium Sulfate Ipratropium Bromide SAO2 Suctioning Solu-medrol Sodium Chloride ETCO2 Oxygen Therapy Glucagon Diazepam Blood Glucose Medical Equipment Adjustment Nitroglycerine Fentanyl Temperature Burn Care Metoprolol Diphenhydramine Weight Hemorrhage Control Labetalol Midazolam Vital signs Invasive Tube Assessment Odansetron Morphine Sulfate EKG Rhythm Interpretation IV Catheter Placement & Removal Dextrose 50% Lorazepam 12 Lead EKG NG Tube Placement & Removal Albuterol Environmental Assessment Pain Management Tetracaine Medication Administration Naloxone In Home Assistance Aspirin IV Fluids Furosemide 13 Mobile Integrated Healthcare Community Paramedicine Program Transport to ED Required Solutions Diagnostics None Require Transport Treatments Formulary Advanced Airway Management (ALS) Atropine BiPAP / CPAP Dopamine Severe Hemorrhage Control Adenocard C-Spine Immobilization Epinephrine Defibrillation / Cardioversion Calcium Chloride External Pacing Vasopressin IO Placement Amiodarone Long Bone Splinting Diltiaizam Sodium Bicarbonate Etomidate Vecuronium 14 Integrating Telemedicine • In 2014, the Verizon Foundation awarded a grant to the North ShoreLIJ Health System • LG G2 wireless devices and lines of service were provided as in-kind support to allow for secure video conferencing (WebEx) between the paramedic, OLMC MD, and patient/family during Community Paramedicine responses • Launched in September 2014, integration of telemedicine allows for more accurate assessment and enhanced “physician extender” ability. 15 Comprehensive Mobile Integrated Healthcare Community Paramedicine Program • Year One Program Results – – – – – Operational Metrics Clinical Metrics Outcome Metrics Quality of Care & Patient Safety Metrics Financial Metrics 16 Operational Metrics There were a total of 2,889 House Calls patient calls over the course of the first year Community Paramedicine was activated for 386 of these calls (13.4%) 88 Community Paramedicine calls (22.8%) resulted in transport to the hospital Community Paramedicine Responses Time (min) Average CP Response time 22 Average CP time on scene 65 Average task time 80 Over 60% of the calls occurred during House Calls non-business hours 17 Operational Metrics CP Call Volume by Month 70 60 50 40 30 20 10 0 18 Clinical Metrics EMD Coding by Category respiratory/ cough/mucous public assist/no medical 7% concern 5% behavioral abnl 2% labs/vitals 5% cardiac 4% pain/discomfort/reaction/ uti 13% GI/nausea /vomit 10% dizzy/weak/lethargic/am s/ neuro/dehy/intk or output issues/fever/ diabetes 45% 19 catheter issue 1% circulatory/cellulitis/skin 8% Clinical Metrics EMD Problem/ Nature Transport Avoidance Transport Avoided Transported Sick Persons (Specific Diagnosis) Breathing Problems Unable To Determine 42 Falls 20 5 Chest Pain (Non-Traumatic) 14 7 Unconscious/Fainting (Near) 15 2 Hemorrhage/Lacerations 9 8 Stroke (CVA) 10 1 Abdominal Pain/Problems 7 3 Convulsions/Seizures 5 1 Heart Problems/AICD 5 Diabetic Problems 4 Traumatic Injuries (Specific) 2 Psychiatric/Abnormal Behavior/Suicide Attempt 2 Unknown Problems (Person Down) 1 Overdose/Poisoning (Ingestion) 1 Headache 1 Back Pain (Non-Traumatic or Non-Recent…1 Cardiac or Respiratory Arrest/Death 0 20 72 64 22 22 17 Clinical Metrics EMD Problem/Nature by Non-Transport Type CP: Evaluated CP: Evaluated & Treated CP: Pronouncment CP: Evaluated & OLMC Care Plan Change CP: Evaluated/Treated/Pronouncment Sick Persons (Specific Diagnosis) 36 Breathing Problems 22 Unable To Determine 26 Falls 14 4 2 Cardiac or Respiratory Arrest/Death 22 Chest Pain (Non-Traumatic) 8 4 2 Unconscious/Fainting (Near) 5 7 3 Hemorrhage/Lacerations 5 0 4 Stroke (CVA) 5 4 1 Abdominal Pain/Problems 3 3 1 Convulsions/Seizures 2 21 Heart Problems/AICD 12 2 Diabetic Problems 1 3 Traumatic Injuries (Specific) 2 Psychiatric/Abnormal Behavior/Suicide…2 Unknown Problems (Person Down) Overdose/Poisoning (Ingestion) 1 Headache 1 Back Pain (Non-Traumatic or Non-…1 21 16 11 24 26 5 12 1 Clinical Metrics Emergency Medical Dispatch Priority Codes ECHO DELTA CHARLIE • Choking with complete obstruction • Allergic reaction with ineffective breathing • Respiratory/cardiac conditions with ineffective breathing • Allergic reaction with AMS • Breathing problems with AMS • Breathing problems color change • Burn ≥ 18% of body area • Choking with abnormal breathing • Abnormal breathing conditions • Cardiac problems (with history) • Headache with speech problems • Overdose with Altered Mental Status • Stroke conditions BRAVO • Unknown conditions • Possibly dangerous trauma injuries • Non-imminent labor • Serious hemorrhage ALPHA • Low acuity response with no priority symptoms OMEGA • Response level for special referrals • Poison control center or nurse advice • Non-priority complaints 22 Clinical Metrics Transport Avoidance by EMD Priority Code Transports avoided Transported 0.00% 73.3% 26.7% 80.5% 19.5% 67.5% 32.5% 78.7% 21.3% 100.0% 71.2% 28.8% 23 Clinical Metrics EMD Priority Code by Non-Transport Type CP: Evaluated CP: Evaluated & Treated CP: Pronouncement CP: Evaluated & OLMC Care Plan Change CP: Evaluated/Treated/Pronouncement 100% 26% 32% 48% 38% 24% 63% 12% 27% 26% 57% 35% 6% 4% 1% 11% 8% 82% 62% 26% 24 12% Clinical Metrics Administered Treatment by Disposition Evaluated & Treated Evaluated, Treated & Transported IV catheter/saline lock placement 32 Medication administration - Intravenous 35 Oxygen therapy (blow by/ nasal cannula/nebulizer/trach mask) 22 Medication administration - Nebulized Medication administration - Oral 16 3 Hemorrhage control Medication administration - Intramuscular 5 5 1 2 3 Medication administration - Sublingual Pain Management 22 4 2 BVM ventilation 1 Medication administration - Intranasal 1 25 13 19 5 Clinical Metrics Administered Medication by Disposition CP: Evaluated & Treated Albuterol (0.083%) Sodium Chloride 0.9% Furosemide Ipratropium Bromide Morphine Sulfate Solu-medrol Aspirin Nitroglycerin Dextrose 50% Ondansetron Glucagon Metoprolol Naloxone Fentanyl Diazepam Labetalol CP: Evaluated, Treated & Transported 15 14 13 6 6 4 10 6 8 6 4 1 3 1 4 3 1 1 2 2 2 1 1 1 1 26 Clinical Metrics Follow-Up Planning Non-Documented 5% Scheduled CP follow up 2% House Calls follow up – Telephonically 14% No Follow up needed 55% House Calls follow up Patient Visit 24% 27 Quality of Care & Patient Safety Avoidable Transports by Presenting Problem Transports Presenting Problem of Potentially Avoidable Transports Hypotensive w/o IV access 1 Hyperglycemia 1 Lacerations 1 GI/Constipation 1 UTI 1 61% 13% 26% Foley Catheter/Pubic Tube issues 3 Labs needed Non-avoidable transports Patient/ Family choice 4 Peg Tubes 5 Pneumonia/Resp. Infection 6 0 Potentially avoidable if received in home care 28 1 2 3 4 5 6 7 Quality of Care & Patient Safety RCA to avoid future Transports 34 (38.6%) of the 88 CP transports were potentially avoidable Reason for Transport # Occurrences Potential Solution Patient/Family Choice 11 Patient/Family Education Labs needed 4 I-STAT/ Point of Care testing Peg Tubes 5 Ultra Sound/X-ray, Training for CP Foley Catheter/Pubic Tube issues 3 Training for CP Pneumonia/Resp. Infection 6 I-STAT/ABX/Chest X-ray UTI 1 I-STAT/ABX/Foley replacement GI/Constipation 1 Laxative, Training for CP Lacerations 1 Suture training for CP Hyperglycemia 1 Insulin Hypotensive w/o IV access 1 Conscious IO access 29 Quality of Care & Patient Safety Physician Survey Responses Did the information provided by the Community Paramedicine evaluation change your medical management? Yes 118 (74%) 0% • • • • • 20% No 41 (26%) 40% 60% “Patient had large laceration on foot and it would not have been washed and dressed properly (with a pressure dressing) if the Community Paramedic was not there.” “The negative neurological exam helped remove possibility of CVA.” “I was not going to prescribe antibiotics until the evaluation by CP medics revealed abnormality of skin.” “The patient complained of being short of breath but her normal oxygen saturation provided reassurance that she could be treated at home.” "I was going to order an x-ray, which would have meant waiting 5+ hours for results. But one leg was actually found to be rotated and shorter than the other, so immediate transport was arranged, avoiding hours of suffering." 30 80% • • • • 100% Death pronouncement Reassurance for overwhelmed or distressed caregiver Public assist Patient is on hospice; has no intention of being hospitalized Quality of Care & Patient Safety Physician Survey Responses If the Community Paramedicine evaluation had not been available, would you have advised the patient to go to the ER? Yes 110 (69%) 0% 20% No 50 (31%) 40% 60% 80% 100% • “I definitely was going to send the patient to the ER if Community Paramedicine had not been available.” • “The Community Paramedics’ evaluation gave me more confidence in my plan. I would have recommended that the patient go to ER based on the symptoms described by the patient’s daughter.” • “I originally was going to have the patient stay home, but then found that she was somnolent and hypoxic so I sent her to the hospital for further evaluation.” • “Patient was recently accepted onto hospice and wanted to stay home.” 31 Quality of Care & Patient Safety Physician Survey Responses Did video monitoring enhance your evaluation of the patient during the Community Paramedicine response? Yes 59 (81%) No 14 (19%) 0% 20% 40% 60% 80% 100% • “It showed the intensity of the bleeding from the patient’s trach.” • “I was able to see urine and that the foley was draining despite what the patient stated.” • "Video conferencing allowed me to see my patient pre-Lasix. Since she is my patient, I was able to see that she was more lethargic than usual, despite the paramedic's report that she looked 'fine.' I could see her change from baseline status. She appeared more energetic after the Lasix was given, and she was able to stay at home." • "I was able to see on video conference that the patient was flat in bed, and recommended he be raised HOB to help with cough. I decided not to prescribe Albuterol." 32 Quality of Care & Patient Safety Patient Satisfaction Survey Results • 107 surveys were mailed to the patient home following a Community Paramedicine (CP) response from 9/17/14 to 12/5/14. – Surveys were not mailed to patients who passed away. – Patients who had multiple CP responses within a 1-3 day window received one survey. • 32 surveys were completed (30% response rate) – 5 (16%) were completed by the patient – 27 (84%) were completed by a family caregiver 33 Quality of Care & Patient Safety Patient Satisfaction Survey Results I was satisfied with how the oncall House Calls The Community provider and My goals for I would use the Paramedics Community medical care Overall, I was CP service in a delivered highParamedics were accounted satisfied with my future medical quality services managed my for in the CP experience. emergency. and care. medical issues. treatment plan. 100% 80% 60% 28 (93%) 27 (90%) 2 (7%) 3 (10%) 28 (93%) 28 (93%) 27 (90%) 40% 20% 0% Neutral 2 (7%) 2 (7%) Agree Strongly Agree 34 2 (7%) 1 (3%) Quality of Care & Patient Safety Patient Satisfaction Survey Results If the Community Paramedicine Program did not exist, what would you have done during your medical emergency? Dialed 911 23 (62%) Went to the Emergency Room for evaluation or treatment 11 (30%) Waited to see if I got better 3 (8%) 0% 20% 40% 60% 80% 100% • “Could not have asked for more. Could not be more grateful for be in the House Calls Program.” • “I (the caregiver) was completely satisfied with the doctor and Paramedics in the prompt care my father received, from the time the doctor called me with the results of his blood work, to his care by paramedics, to his trip to the ER.” • “I was very impressed with the program. I am an RN and I truly appreciate the level of professionalism and caring that was shown to my father. Bernard (our paramedic) made my father feel at home immediately. This is a wonderful program.” • “I am the daughter of an elderly patient. The House Calls program and Community Paramedics have been an absolute lifesaver - for all of us. With your amazing care, we have been able to keep my mother at home, out of the hospital, comfortable, and incredibly 35 well cared for.” Outcome Metrics Admission Rate of Transported Patients CP Transport Inpatient Admission Rate Avg. CP Transport Inpatient Rate Non-CP Transport Inpatient Admission Rate Avg. Non-CP Transport Inpatient Admission Rate 110% 100% 100% 100% 90% 100% 100% 92% 88% 83% 80% 80% 83% 70% 82% 69% 60% 50% 50% November December 2013 2013 January 2014 February 2014 March 2014 April 2014 36 May 2014 June 2014 July 2014 August 2014 September 2014 October 2014 Community Paramedic Program Financial Metrics • Costs based on leveraging existing CEMS infrastructure • Calculated using fixed and variable costs per visit • Approximately $200 per visit @ 1.25 hours which includes: – Vehicle, maintenance and fuel – Salaries, wages and benefits – Medications, supplies and equipment – Dispatch services and specialized software – Integrated call services – Other general expenses 37 Payment Avoidance Estimations 38 Marketplace Challenges Government Payment Reductions Payer Mix Shift to Gov’t Payers & Exchanges Readmission Penalties Increased Consumerism and Price Transparency Downgrades/ DenialsRAC/MAC Inpatient Volume & Case Mix Declines Increased Provider Competition 39 Health System Strategy Strategy 40 Risk Based Contracts Program Type Description Full Risk • Receive all or portion of premium. • Responsible for total cost of care. Shared Risk • Share in upside/downside savings/losses relative to pre-established spending target. • Responsible for all or portion of medical spend. • Quality Gate • Eligible to share upside savings with payer relative to Shared Savings pre-established spending target. • Quality Gate 41 Margin Impact SourceAdvisory Board. The Essentials of Risk Based Contracting Comprehensive Mobile Integrated Healthcare Community Paramedicine Program Program successes to date • 24x7 on-demand Community Paramedic response effectively and efficiently fills care gaps in the home • Significant decrease in transports to the ED yielding subsequent payment and cost avoidance • High patient satisfaction levels • Zero adverse clinical outcomes • Low cost of services compared to acute care setting • Opportunities exist to lower transport rate even further 43 Comprehensive Mobile Integrated Healthcare Community Paramedicine Program Program challenges to date • Physician understanding and adoption of EMS capability and scope into workflow • Scope of practice / formulary limitations • State regulatory hurdles & limitations • Payer source (internally funded R&D project) • Data integration amongst disparate systems 44 Questions? 45