Benjamin - Rating Agency Outlook
advertisement
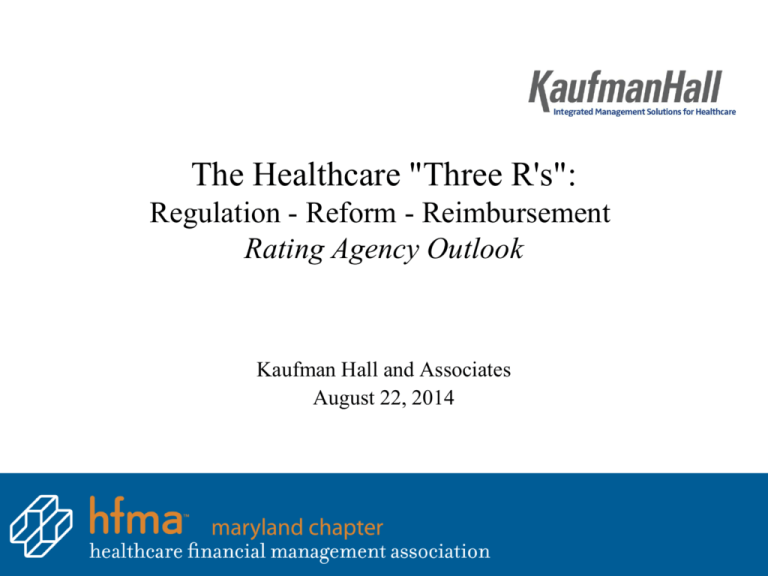
The Healthcare "Three R's": Regulation - Reform - Reimbursement Rating Agency Outlook Kaufman Hall and Associates August 22, 2014 Discussion Agenda • • • • Background and Methodology Standard & Poor’s Medians Moody’s Medians Fitch Medians 1 RATING AGENCY: BACKGROUND AND METHODOLOGY 2 Key Themes from Rating Agencies • All rating agencies give the health care industry a negative outlook • Increasing challenges in preserving profitability – inpatient volumes pressured, increasing use of high-deductible health plans, Medicare and other payers with lower than historical rate increases • Harder-to-find cost savings • Uncertainty about the Affordable Care Act • Focus on management to navigate the changing environment • Strategic partnerships will continue 3 Why Does a Credit Rating Matter? • Creditworthy organizations have improved capital market and borrowing opportunities – Less restrictive bond covenants – Access to a wider range of lending institutions – Avoidance of a debt service reserve fund • Creditworthy organizations have a lower cost of capital – A” vs. “BBB” historical interest rate spread range of approximately 75+ bps – Access to a variety of debt options • Creditworthy organizations are market consolidators – Nationwide, organizations with the highest credit ratings have been the most attractive partners, have excess capital capacity and the lowest cost of capital to consolidate the market 4 Negative Outlooks Reflect Accelerating Industry Pressures “…negative sector outlook reflects the forces of pressure weighing on the sector (lower reimbursement, suppressed inpatient volumes, higher deductible plans and additional spending cuts) as it enters this potentially historic period of change” Fitch, December 11, 2013 “The negative outlook is due to a multitude of factors, including: top line revenue constraints, the impact of health care reform readiness activities, soft demand, and emerging changes to the payment environment" Standard & Poor’s, December 10, 2013 “Our sector outlook for not-for-profit hospitals remains negative reflecting the challenging operating landscape over the next 12-18 months as patient volumes shrink and revenue growth slows" Moody’s Investors Service, November 25, 2013 5 Rating Agency Perspective: Key Drivers • Economy: unemployment, state budges, healthcare funding • Utilization: flat to declining industry-wide • Reimbursement: pressure on rates and what’s reimbursed • Expenses: vs. revenue growth, continued reduction efforts • Payer mix: government, commercial, cost shifting • Physician alignment: investment and operating losses • Healthcare reform: uncertainty and bi-modal transition period • New market entrants: private equity, for-profits, insurers, retail • Consolidation: search for scale leading to rapid consolidation 6 Credit Ratings Are Influenced by Range of Factors Can be influenced in short-term Cannot be influenced in short-term • • • • • • • • • • Financial performance, trends, and expectations Strategic and financial planning Governance/ management Market position Payor mix Physician relations Debt and capitalization position Size and critical mass which mitigate risk Number of physical locations for diversification Industry trends and external perception of risk 7 Distribution of Tax-Exempt Healthcare Ratings Non-IG Moody 9% S&P 27% 10% Fitch BBB / Baa A 49% 35% 6% 15% 47% 28% 0% AA / Aa 8% 41% 20% 40% 25% 60% Non Investment Grade 80% 100% Investment Grade Moody’s B3 B2 B1 Ba3 Ba2 Ba1 Baa3 Baa2 Baa1 A3 A2 A1 Aa3 Aa2 S&P, Fitch B- B B+ BB- BB BB+ BBB- BBB BBB+ A- A A+ AA- AA Note (1): Based on Moody’s most recent not-for-profit healthcare median report published August 2013 Note (2): Based on S&P’s most recent not-for-profit stand-alone hospital median reports published August 2014 Note (3): Based on Fitch’s most recent not-for-profit healthcare median report published August 2014 8 RATING AGENCY – STANDARD & POOR’S (S&P) 9 Standard & Poor’s • 2013 ratings published August 13, 2014 • Provides separate ratings for Stand-Alone Hospitals and Health Systems • The distribution of System ratings continues to be of significantly higher credit quality than that of Stand-Alone providers, with the majority of ratings in the 'AA' category and the higher end of the 'A' category, while the 'A' and 'BBB' categories dominate the stand-alone realm • In S&P’s opinion, systems remain better positioned than stand-alone providers to manage and adapt to industry forces, in part, due to the benefits of revenue and geographic diversity, overall scale, and capability to attract and retain top-tier physicians and management, all of which compensate for the systems' slightly weaker financial metrics in 2013 10 Standard & Poor’s Distribution of Ratings Stand-Alone vs. System Rating Categories 25% 20% 15% Stand-Alone System 10% 5% 0% AA AA- A+ A A- BBB+ BBB BBB- Spec 11 Standard & Poor’s 2013 System Medians • The 2013 medians for U.S. not-for-profit health care systems reflect a decline in operating performance for the first time since 2008 due to operating expenses that outpaced patient revenue growth. • Strong investment returns not only helped offset reduced margins, but they also bolstered many balance-sheet metrics with stronger unrestricted reserves and improved pension results. Increased balance-sheet strength in turn enhanced financial flexibility, enabling many health systems to absorb the impact of changing dynamics in health care delivery and reimbursement. 12 Standard & Poor’s 2013 System Medians (continued) • While revenue in 2013 grew at a faster pace than we expected, with an overall increase of 5%, expenses rose even more at 7%. This marks another year of patient revenue growth for systems, although we find the increase is tied less to volume growth and more to mergers and acquisitions, increased physician employment, which added hospital referrals as well as revenue from the owned practices, and special funding mechanisms such as provider fees and meaningful use technology funds from the government. • The growth in expenditures reflects higher operating costs to prepare for health care reform, including technology investment and consulting fees, higher physician costs, provider taxes paid, and increased salaries and pharmaceutical costs. 13 Standard & Poor’s System Profitability Trends 12.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% 2007 2008 Operating Margin 2009 2010 2011 Operating EBIDA Margin 2012 2013 Excess Margin 14 Standard & Poor’s System Liquidity Trends Days Cash on Hand 250 200 181 175 154 154 2008 2009 189 194 2011 2012 205 150 100 50 2007 2010 2013 Days Cash on Hand 15 Standard & Poor’s System Rating and Outlook Actions System Rating and Outlook Actions 16 14 12 10 2011 2012 2013 8 6 4 2 Downgrades Upgrades Negative Outlook Actions Positive Rating Actions 16 Standard & Poor’s System Outlook • • • • • Expects continued compression in operating margins in 2014 due mainly to inpatient volume decline. Anticipate nonoperating revenues, specifically investment earnings, will continue to grow, given that year-to-date investment market performance has remained sound. See that many cost escalators in 2013 have continued into 2014, including further operating costs to support infrastructure development, physician employment, joint-venture relationships, and mergers and acquisitions. These costs are likely to affect next year's medians as well. One bright spot may be what we believe is a near-to-medium-term spike in volume from Medicaid expansion and exchange patients. Under the Affordable Care Act, providers could see a drop in charity care and bad debt expenses, although there may be some offsetting increases from patients unable to afford high deductibles and copayments associated with their new insurance coverage. In addition, with continued merger and acquisition activity, health systems are creating opportunities to achieve cost reductions through increased economies of scale and regional clout. 17 S&P Rated Systems in Maryland System Rating Outlook Bon Secours Health System A- Stable Johns Hopkins Health System AA- Stable MedStar Health A- Stable University of Maryland Medical System A- Stable Rating as of August 13, 2014 18 Standard & Poor Stand-Alone Medians for 2013 ($ millions) S&P S&P S&P S&P S&P S&P S&P S&P S&P AA AA- A+ A A- BBB+ BBB BBB- Spec 12 $1,092.8 $1,198.9 16 $760.3 $697.7 60 $480.5 $398.9 49 $407.1 $253.6 60 $295.0 $171.9 39 $282.1 $138.9 46 $160.3 $75.7 42 $175.8 $59.6 38 $127.8 $29.1 Profitability Operating Margin Operating EBIDA Margin 5.4% 12.0% 5.7% 12.0% 4.0% 10.9% 2.4% 9.5% 2.3% 9.3% 1.4% 8.2% 1.2% 8.8% 1.0% 8.0% (2.8%) 4.9% Debt Position Debt Service Coverage Debt to Capitalization 6.3 21.4% 6.0 23.6% 4.9 26.7% 4.4 27.6% 3.4 35.2% 3.3 34.2% 2.5 37.9% 2.6 37.5% 1.7 49.8% Liquidity Cash to Debt Days Cash on Hand (days) 285.1% 393.4 237.0% 307.9 185.8% 290.9 179.1% 245.6 139.0% 191.6 123.3% 187.3 103.9% 161.4 103.1% 127.2 56.6% 95.2 Other Capital Spending Ratio Compensation Ratio 152.7% 58.3% 148.1% 56.6% 118.0% 53.7% 127.4% 56.8% 123.5% 57.1% 112.9% 55.7% 99.4% 56.5% 85.5% 56.2% 81.0% 55.2% Sample Size Net Patient Revenue Unrestricted Cash Medians based on and S&P Stand-Alone Median Ratios for Nonprofit Hospitals for Fiscal Year 2013 (published in 2014). 19 Standard & Poor’s Stand-Alone Hospital Profitability Trends 14.0% 12.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% 2008 2009 Operating Margin 2010 2011 Operating EBIDA Margin 2012 2013 Excess Margin 20 Standard & Poor’s Stand-Alone Hospital Liquidity Trends Days Cash on Hand 250 187 192 198 2010 2011 Days Cash on Hand 2012 2013 200 150 146 152 2008 2009 165 100 50 - 21 Standard & Poor’s 2013 Stand-Alone Medians • The 2013 median ratios for stand-alone hospitals were mixed, with weaker operating margins offset by balance-sheet improvement. • Balance-sheet measures improved for the most part, with an increase in unrestricted reserves despite softer operating income as many providers enjoyed favorable investment returns. • This is reflected in improved nonoperating income, which has boosted excess income from a year earlier. However, unrestricted reserves to operating expenses, as measured by days' cash on hand, was mixed at some rating levels. • The growth in nonoperating income also highlights a growing dependence on nonoperating income, which leaves many providers exposed to uncertain investment markets. 22 Standard & Poor’s Stand-Alone Hospital Medians Distribution of Ratings 80 70 60 50 40 2012 2013 30 20 10 AA AA- A+ A A- BBB+ BBB BBB- Spec 23 Standard & Poor’s Stand-Alone Hospital Medians Net Patient Revenue $1,200 $1,000 $800 2012 2013 $600 $400 $200 $AA AA- A+ A A- BBB+ BBB BBB- Spec 24 Standard & Poor’s Stand-Alone Hospital Medians Operating Margins 6.0% 5.0% 4.0% 3.0% 2012 2013 2.0% 1.0% 0.0% AA AA- A+ A A- BBB+ BBB BBB- Spec -1.0% -2.0% 25 Standard & Poor’s Stand-Alone Hospital Medians Operating EBIDA Margins 14.0% 12.0% 10.0% 2012 2013 8.0% 6.0% 4.0% 2.0% AA AA- A+ A A- BBB+ BBB BBB- Spec 26 Standard & Poor’s Stand-Alone Hospital Medians Unrestricted Cash $1,400.0 $1,200.0 $1,000.0 $800.0 2012 Cash 2013 Cash $600.0 $400.0 $200.0 $0.0 AA AA- A+ A A- BBB+ BBB BBB- Spec 27 Standard & Poor’s Stand-Alone Hospital Medians Days Cash on Hand $450.0 $400.0 $350.0 $300.0 $250.0 2012 2013 $200.0 $150.0 $100.0 $50.0 $0.0 AA AA- A+ A A- BBB+ BBB BBB- Spec 28 Standard and Poor’s Contemplated Updated Rating Methodology “The criteria establishes a formal framework for performing credit analysis using the same elements that have long been a part of our analysis and that are routinely discussed in our rating committees.” – Standard & Poor’s, December 5, 2013 • • Basic framework uses a weighted average of an enterprise and financial profile score Financial Profile • Enterprise Profile – 40%: Financial Performance – 30%: Liquidity & Financial Flexibility – 30%: Debt & Contingent Liabilities – 20%: Industry Risk – 20%: Economic Fundamentals – 50%: Market Position – 10%: Management & Governance • After these scores are accumulated, certain positive and negative factors outside the outlined framework are assessed – Management strength, close affiliation with strong organizations (ex. AMC with a University), specialty designations, etc. 29 Preliminary S&P Rating Analysis: Financial Profile Sample Hospital I. Financial Performance Net Patient Service Revenue ($M) EBIDA Margin Operating Margin Excess Margin Maximum Annual Debt Service Coverage Lease-adjusted MADS Coverage Weight 40% 16.7% 16.7% 16.7% 16.7% 16.7% 16.7% FY 2011 FY 2012 FY 2013 FY11 to FY13 (weighted) Value Score 689.6 5.2% -0.5% -2.2% 2.0 1.3 735.2 8.5% 2.2% 0.8% 3.6 2.6 758.2 7.2% 1.0% 4.2% 3.0 1.8 736.4 7.2% 1.1% 1.7% 3.0 2.0 Initial Score: 2 6 4 5 4 5 4.33 II. Assessing Liquidity and Financial Flexibility Average Age of Plant (yrs) Capital Expenditures/Depreciation Expense Cash on Hand (Days) Unrestricted Reserves/Long-Term Debt Unrestricted Reserves/Contingent Liabilities 30% 15% 15% 30% 30% 10% 16.1 211.7% 100.4 70.3% 87.7% 11.7 75.6% 102.2 75.4% 92.5% 10.3 93.6% 106.1 80.4% 100.8% 12.0 110.9% 103.6 76.6% 95.3% Initial Score: 4 4 5 5 5 4.70 III. Assessing Debt and Contingent Liabilities Debt Burden Long-Term Debt/Capitalization Contingent Liabilities/Long-Term Debt Funded Status (DB Pension) 30% 25% 25% 25% 25% 2.5% 79.8% 82.1% 52.6% 2.4% 81.5% 83.7% 52.6% 2.4% 60.0% 82.4% 65.5% 2.4% 71.5% 82.8% 58.4% Initial Score: 2 6 6 5 4.75 Initial Financial Profile Score 4.57 30 Preliminary S&P Rating Analysis: Enterprise Profile Sample Hospital I. Industry Risk 20% II. Economic Fundamentals Primary Service Area Population 20% 100% III. Market Position Market Share Medical Staff Payer Mix Clinical Quality and Information Technology 50% 50% 20% 15% 15% IV. Management and Governance 10% Initial Enterprise Profile Score Value N/A Initial Score: Score 3 3 1,200,000 Initial Score: 2 2 25% N/A N/A N/A Initial Score: 3 3 4 3 3 N/A 2 Initial Score: 2 2.78 31 Preliminary S&P Rating Analysis: Indicative Rating Enterprise Profile Financial Profile 1 2 3 4 5 6 1 AAA AA+ AA- A- BBB+/BBB BB+/BB 2 AA+ AA/AA- A+ A- BBB/BBB- BB/BB- 3 AA- A+ A BBB+/BBB BBB-/B+ BB- 4 A A/A- A-/BBB+ BBB/BBB- BB B+ 5 BBB+ BBB/BBB- BBB-/B+ BB BB- B 6 BBB- BB BB- B+ B B- Sample Hospital 32 Standard & Poor’s Stand-Alone Outlook • S&P expects the trend in weaker operating margins to continue as providers are facing mounting challenges, including weaker volume trends, increased integration costs relating to physician employment, and substantial investments in technology amid an evolving reimbursement environment due to health care reform. • S&P expects these trends will continue to pressure the sector over the next several years especially given the difficulty of finding the next level of expense cuts to offset the investments providers need to make to maintain their financial stability. • S&P believes the sector is at a tipping point where negative forces have started to outweigh many providers‘ ability to implement sufficient countermeasures. 33 S&P Rated Stand-Alone Hospitals in Maryland System Rating Outlook Anne Arundel Health System A- Stable Greater Baltimore Medical Center A Stable LifeBridge Health, Inc. A Positive Mercy Health Services BBB Negative Meritus Health, Inc. BBB- Stable Peninsula Regional Medical Center A Stable Rating as of August 13, 2014 34 RATING AGENCY – MOODY’S INVESTORS SERVICE 35 Moody’s Medians for 2012 ($ millions) Moody's Moody's Moody's Moody's Moody's Moody's Moody's Moody's Moody's "Aa2" "Aa3" "A1" "A2" "A3" "Baa1" "Baa2" "Baa3" "Below Baa" $2,329.7 $2,824.4 $1,379.9 $1,055.7 $746.6 $536.4 $464.7 $279.0 $391.9 $194.2 $446.4 $175.8 $252.0 $102.4 $206.7 $76.1 $202.5 $42.3 Profitability Operating Margin Operating EBIDA Margin 3.9% 10.8% 3.5% 10.4% 3.6% 10.9% 3.2% 10.2% 1.9% 10.0% 1.2% 7.8% 1.2% 8.8% 1.2% 7.9% (1.8%) 4.7% Debt Position Debt Service Coverage Debt to Capitalization 9.2 29.7% 7.0 31.8% 5.4 34.7% 5.6 37.3% 4.2 41.0% 3.5 47.4% 3.0 49.3% 3.5 47.6% 2.2 57.8% Liquidity Cash to Debt 222.2% Days Cash on Hand (days) 289.9 177.4% 239.1 151.1% 218.8 139.5% 207.9 112.7% 175.9 92.0% 149.0 81.6% 139.5 86.4% 132.9 55.9% 80.1 125.6% 105.5% Net Patient Revenue Unrestricted Cash Other Capital Spending Ratio 132.9% 143.5% 123.8% 121.2% 113.6% 85.9% 95.8% Medians based on and Moody’s Nonprofit Hospitals and Healthcare Systems for Fiscal Year 2012 (published in 2013). 36 2012 Moody’s Rating Distribution by Revenue Size 100% 110 86 62 41 22 $2.0B- $4.0B $4.0B+ 75% 50% 25% 0% $250M- $500M $500M- $1.0B $1.0B- $2.0B Aa A Baa Non-IG Source: Information supplied by Moody’s Investors Service based upon 2008-2012 published ratios. 37 Moody’s Healthcare Scorecard - Overview • Moody’s updated their methodology in March 2012 and released a rating methodology report explaining their approach to assigning ratings to not-for-profit providers – As part of the report, Moody’s included a scorecard that has a weighted quantitative grid • The report also included a set of qualitative factors that can impact the rating – Subjective and weights vary from credit to credit – As guidance, these factors can impact the rating by one notch but there is no exact weight for each sub-factor • In addition to an updated rating methodology, Moody’s is currently tracking key ratios and statistics not previously tracked – Unique patients, Medicare readmission rates, Readmission rate, Total case mix index, # of employed physicians, Worked RVUs for employed physicians, active medical staff (independent & employed) – Each indicator is meant to give insight as to the organizations ability to succeed in a new value based/post reform healthcare environment 38 Moody’s Healthcare Scorecard – Quantitative Factors Sample Hospital – FYE 2013 Sub-Factor Weights Value Score Implied Rating 25% 10% 784,135 3.0 5.43 9.51 A1 Baa3 5% 5% 44.1 21.9 7.28 10.75 A3 SG Factor 2: Operating Performance (30%) Operating Cash Flow Margin (%) Debt to Cash Flow (x) MADS Coverage (x) 10% 10% 10% 7.20 7.50 3.70 8.70 10.08 7.20 Baa2 Baa3 A3 Factor 3: Balance Sheet and Capital Plan (25%) Days Cash on Hand (x) Cash to Debt (%) Monthly Liquidity to Demand Debt (%) 10% 10% 5% 99 75 0.94 8.85 9.02 20.90 Baa2 Baa2 SG Factor 1: Market Position (45%) Total Revenue ($000's) Revenue Growth Rate (%) (3 yr CAGR) Medicare and Medicaid payer mix (% of Gross Revenues) Medicare Medicaid Weighted Score Legend Aaa Aa1 Aa2 > 1.5 2.5 ≤ 1.5 2.5 3.5 Aa3 3.5 4.5 A1 4.5 5.5 A2 5.5 6.5 A3 6.5 7.5 Baa1 Baa2 Baa3 7.5 8.5 9.5 8.5 9.5 10.5 SG 10.5 Weighted Score: 8.64 Grid Rating Baa2 39 Moody’s Healthcare Scorecard – Qualitative Factors • These factors can impact the rating by one notch each (up to three notches total), but there is no exact weight for each sub-factor Factors 4 & 5: Governance, M anagement, Debt Structure and Other Debt Structure Specific Considerations Positive, Negative, or Neutral Analyst Notching (+/-) Net Notching → 0.0 4) Governance and M anagement a. Composition of Board and Senior Management b. External Disclosures and Internal Controls c. Integrated Short and Long-Range Planning d. Ongoing Self-Assessment and Benchmark ing e. Government and Stak eholder Relations 5) Debt Structure and Legal Security a. Interest Rate, Counterparty, and Refinancing Risk b. Borrowing Terms and Covenants c. Legal Security and Other Bondholder Protections Other Credit Specific Considerations a. Multi-year Trend in Key Operating and Balance Sheet Factors b. Ownership and Support by University or State/Local Government c. Presence or Absence of CON d. Mark et Share e. Other Factors (ex: Comprehensive Debt) 40 RATING AGENCY – FITCH RATINGS 41 Fitch Medians for 2013 ($ millions) Sample Size Operating Revenue Fitch Fitch Fitch Fitch Fitch Fitch Fitch Fitch AA AA- A+ A A- BBB+ BBB BBB- 14 $2,588.5 45 $1,484.1 31 $695.6 38 $545.7 30 $479.0 41 $431.0 18 $306.8 10 $341.6 Profitability Operating Margin Operating EBIDA Margin 6.0% 11.7% 3.9% 10.9% 3.7% 10.4% 2.0% 9.3% 2.2% 9.1% 0.7% 7.8% 1.0% 8.0% 2.5% 8.4% Debt Position Debt Service Coverage Debt to Capitalization 5.5 26.9% 5.3 32.3% 4.5 35.1% 3.6 35.4% 3.2 42.2% 2.8 44.8% 2.3 49.7% 3.0 43.6% Liquidity Cash to Debt Days Cash on Hand (days) 191.2% 287.2 167.4% 275.6 168.2% 237.3 138.5% 239.3 110.1% 178.1 158.4% 52.3% 125.8% 52.9% 112.2% 54.3% 126.1% 55.5% Other Capital Spending Ratio Compensation Ratio 110.8% 54.4% 97.1% 145.9 103.1% 57.8% 91.7% 142.2 86.6% 56.8% 88.2% 128.1 88.6% 54.9% Medians based on Fitch’s Ratios for Nonprofit Hospitals and Healthcare Systems for Fiscal Year 2013 (published in 2014). 42 Fitch’s 2013 Median Ratios • Fitch reported the 2013 results on August 11, 2014 • For the first time in the past 6 years, Fitch Ratings observed a decline in operating profitability across all rating categories. • Fitch attributes the primary causes driving the decline to be ongoing softness in volumes coupled with the transition to lower cost services, continued reimbursement pressure and ongoing costs associated with the implementation of the Patient Protection and Affordable Care Act (PPACA). 43 Fitch’s 2013 Median Ratios (continued) • Balance sheet liquidity metrics further strengthened with key measures including days cash on hand (DCOH), cushion and cash to debt ratios continuing year-over-year improvement. Fitch believes the balance sheet improvements reflect strong investment returns, solid yet reduced profitability levels, vigilant capital/expense management and aggressive revenue cycle management. • Overall Median Rating Is ‘A’: Since 2003, the median rating in Fitch’s portfolio has migrated upward to ‘A’ from ‘A−’. Furthermore, there has been a significant increase in the percentage of ‘AA−’ rated entities among Fitch’s rated borrowers since 2003. Fitch believes this trend is likely to continue as the sector further consolidates as industry pressures prompt lower-rated credits to affiliate, align or merge with stronger partners. 44 Capital Expenditure Trends 170.0% 160.0% 150.0% 140.0% S&P Moody's Fitch 130.0% 120.0% 110.0% 100.0% 2008 2009 2010 2011 2012 2013 45 Days Cash on Hand Trends 200.0 190.0 180.0 170.0 160.0 150.0 140.0 130.0 120.0 110.0 100.0 S&P Moody's Fitch 2008 2009 2010 2011 2012 2013 46 Fitch Midyear Outlook • Year-to-date rating actions display credit stability within the sector through the first-half of calendar year 2014. • From January 2014–July 18, 2014, Fitch affirmed 100 ratings, downgraded 12 and upgraded 10. Over the same period, there were 31 outlook changes: 16 negative and 15 positive. • Key drivers on negative rating actions or outlook changes primarily reflect the negative impacts related to unexpected inpatient volume declines and an inability to adjust expenses quickly against weaker-than-anticipated revenue. 47 Fitch Midyear Outlook (continued) • Rating drivers on positive rating actions were more varied; several were driven by realized benefits of strategic affiliations, while others’ were a result of volume growth and more efficient operations. • While Fitch expects the majority of rating actions in 2014 to be affirmations, downgrades are likely to outpace upgrades. Fitch believes negative rating actions are likely to be more prevalent among borrowers in the ‘BBB’ rating category and below. Expense-control initiatives will likely garner diminishing returns, and increased uncertainty and costs associated with PPACA implementation will make the operating environment increasingly challenging to manage. 48 Fitch Year-To-Date Ratings YTD Outlooks as of July 2014 YTD Rating Actions as of July 2014 2% 1% Affirmed 8% 10% Stable Positive Negative 90% 9% Upgrade Downgrade 80% Rating Watch On 49 Fitch Rated Hospitals in Maryland System Rating Outlook Affinity Health Alliance A Stable Anne Arundel Health System A- Stable Bon Secours Health Care System A- Stable Calvert Memorial Hospital A Stable Carroll Hospital Center BBB+ Stable Doctors Community Hospital BB+ Stable Frederick Memorial Hospital. BBB+ Stable Johns Hopkins Health System AA- Stable MedStar Health A Stable University of Maryland Medical System A Stable Rating as of August 11, 2014 50 Speaker Biography Jane Benjamin, Vice President, Kaufman Hall & Associates, Inc. Provides both strategic and financial planning assistance to hospitals and health systems nationwide. Her experience includes strategic and financial planning, reimbursement, mergers and acquisitions, demand and utilization forecasting, and financial modeling. Prior to joining Kaufman Hall, Mrs. Benjamin worked for Ernst & Young in its Health Sciences Advisory Services Group for 19 years and was an adjunct faculty member at Carnegie Mellon University. Mrs. Benjamin has an M.B.A. and an M.A. in Healthcare Administration from the University of Iowa and is a CPA. Contact information: Jane Benjamin Vice President Kaufman, Hall & Associates, Inc. 5202 Old Orchard Rd., Suite N700 Skokie, Illinois 60077 724.327.5770 jbenjamin@kaufmanhall.com 51