Presentation: Rachel Baggeley
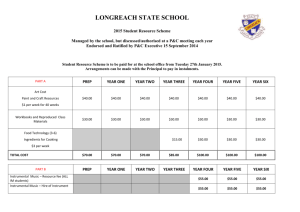
advertisement
Oral pre-exposure prophylaxis (PrEP) for populations at substantial HIV risk Dr. Rachel Baggaley, HIV dept. WHO, Geneva GNP+ WEBINAR: What does PrEP mean for people living with HIV: science, policy and implementation? Date: Thursday, 30th July 2015 Time: 4pm CET Why consider PrEP 2.1 million people infected with HIV in 2013 Among key populations: Burden of HIV infection is 19 fold higher among MSM and 49 fold higher among transgender women compared with the general population. High rates of HIV incidence among MSM across all regions. High HIV prevalence among sex workers in Africa >20% in Nigeria;>50% in South Africa and Zimbabwe. Estimates from South Africa show a 5.6% HIV prevalence among girls aged 15–19 years, increasing to 17.4% for young women aged 20– 24 years. Demonstrated need for more prevention options HIV incidence in 18-35 year women in this community: 9.1% 9.1 per 100 women-yrs (95% CI: 7 - 12) Source: Abdool Karim Q et al, Science 2010 HIV in pregnant women in rural South Africa (2001-2013) Age Group (Years) HIV Prevalence (N=4818) ≤16 11.5% 17-18 21.3% 19-20 30.4% 21-22 39.4% 23-24 49.5% >25 51.9% Source: Abdool Karim Q, Int J Epi, 2014 “Explosive HIV epidemic” among MSM in Bangkok Rationale to focus initial PrEP efforts on younger MSM 60-month cumulative HIV-incidence among MSM in Bangkok, 2006–2012. MSM=men who have sex with men Source: van Griensven F, et al. AIDS, 2013 Mar 13;27(5):825-32. Study Overall evidence for PrEP: July 2015 Effect size (CI) IPERGAY – on demand Truvada 86% (39; 99) (MSM – France & Canada) PROUD – daily oral Truvada 86% (62; 96) (MSM – United Kingdom) Partners PrEP – daily Truvada 75% (55; 87) (Discordant couples – Kenya, Uganda) Partners PrEP – daily oral Tenofovir 67% (44; 81) Oral PrEP (Discordant couples – Kenya, Uganda) TDF2 – daily Truvada 62% (22; 84) (Heterosexuals men and women- Botswana) iPrEx – daily Truvada 44% (15; 63) (MSM - America’s, Thailand, South Africa) FEMPrEP – daily Truvada 6% (-52; 41) (Women – Kenya, South Africa, Tanzania) MTN003/VOICE – daily Truvada -4% (-49; 27) (Women – South Africa, Uganda, Zimbabwe) MTN003/VOICE – daily Viread -49% (-129; 3) Topical PrEP (Women - South Africa, Uganda, Zimbabwe) CAPRISA 004 – coital Tenofovir gel 39% (6; 60) (Women – South Africa) MTN003/VOICE – daily Tenofovir gel 15% (-21; 40) (Women – South Africa, Uganda, Zimbabwe) FACTS 001– coital Tenofovir gel 0% (-40, 30) (Women – South Africa) -130 -60 -40 -20 0 20 40 Effectiveness (%) 60 80 100 Adherence and effectiveness GRADE table: HIV infection Quality assessment No of studies Design Risk of bias Inconsistency Indirectness Imprecision No of patients Oral PrEP Other (containing considerations tenofovir) Control Effect Relative (95% CI) Quality Importance Absolute HIV Infection--PrEP vs. Placebo--Adherence >70% 3 randomised trials no serious risk of bias 39/3866 (1%) 79/2284 (3.5%) RR 0.30 (0.21 to 0.45) 24 fewer per 1000 (from 19 HIGH fewer to 27 fewer) CRITICAL 53/2455 (2.2%) 97/2457 (3.9%) RR 0.55 (0.39 to 0.76) 18 fewer per 1000 (from 9 fewer to 24 fewer) HIGH CRITICAL no serious no serious no serious none inconsistency indirectness imprecision 146/3002 (4.9%) 95/2031 (4.7%) RR 0.95 (0.74 to 1.23) 2 fewer per 1000 (from 12 HIGH fewer to 11 more) CRITICAL no serious no serious no serious none inconsistency indirectness imprecision 3/367 (0.82%) 22/353 (6.2%) RR 0.15 (0.05 to 0.46) 53 fewer per 1000 (from 34 HIGH fewer to 59 fewer) CRITICAL no serious no serious no serious none inconsistency indirectness imprecision HIV Infection--PrEP vs. Placebo--Adherence 40-70% 2 randomised trials no serious risk of bias no serious no serious no serious none inconsistency indirectness imprecision HIV Infection--PrEP vs. Placebo--Adherence <40% 2 randomised trials no serious risk of bias HIV infection--PrEP vs. no PrEP 2 randomised trials no serious risk of bias Systematic review results Analysis No. of studies RCTs comparing PrEP to placebo Overall 10 Adherence High (>70%) 3 Moderate (41-70%) 2 Low (≤40%) 2 Mode of Acquisition Rectal 4 Vaginal/penile 6 Biological sex1 Male 7 Female 6 2 Age 18 to 24 years 3 ≥25 years 3 Drug Regimen TDF 5 FTC/TDF 7 Drug Dosing Daily 8 Intermittent 1 RCTs comparing PrEP to no PrEP Overall 2 1 Sample Size (N) Risk Ratio (95% CI) p-value 17424 0.49 (0.33-0.73) 0.001 70.9 -- 6150 4912 5033 0.30 (0.21-0.45) 0.55 (0.39-0.76) 0.95 (0.74-1.23) <0.0001 <0.0001 0.70 0.0 0.0 0.0 <0.0001 0.009 ref 3167 14252 0.34 (0.15-0.80) 0.54 (0.32-0.90) 0.01 0.02 29.1 80.1 0.36 8706 8716 0.38 (0.25-0.60) 0.57 (0.34-0.94) <0.0001 0.03 34.5 68.3 0.19 2997 5129 0.71 (0.47-1.06) 0.45 (0.22-0.91) 0.09 0.03 20.5 72.4 4303 active 5693 active 0.49 (0.28-0.86) 0.51 (0.31-0.83) 0.001 0.007 63.9 77.2 0.88 17024 400 0.54 (0.36-0.81) 0.14 (0.03-0.63) 0.003 0.01 73.6 0.0 0.14 720 0.15 (0.05-0.46) 0.001 0.0 NA I2 P-value (metaregression) The iPrEx trial included 313 (13%) transgender women. 2 Includes only studies that stratified age by <25 and ≥25. 0.29 WHO guidance on PrEP (2012, 2014, 2015, 2016) 2012. Guidance for MSM & Serodiscordant Couples in the context of demonstration projects to encourage countries to conduct such demonstration projects 201. Consolidated KP Guidelines Recommendation for MSM Among men who have sex with men, PrEP is recommended as an additional HIV prevention choice within a comprehensive HIV prevention package (strong recommendation, high quality of evidence). 2015 Oral PrEP (containing TDF) should be offered as an additional prevention choice for people at substantial risk of HIV infection as part of combination prevention approaches forthcoming 2016 Implementation guidance, package of implementation tools for a variety of implementers and populations forthcoming Implementation tool / guidance, forthcoming Forthcoming new WHO PrEP recommendation New PrEP recommendation in 2015 interim ARV GL forthcoming Oral PrEP (containing TDF) should be offered as an additional prevention choice for people at substantial risk of HIV infection as part of combination prevention approaches • Enabling recommendation • Not population specific – For people at substantial HIV risk (provisionally defined as HIV incidence > 3 per 100 person–years in the absence of PrEP) • Offer as an additional prevention choice • Provide PrEP within combination prevention – – – Condoms and lube Harm reduction HIV testing and links to ART • Provide PrEP with comprehensive support – – – – Adherence counselling Legal and social support Mental health and emotional support Contraception and reproductive health services Who might benefit from PrEP – people at 'substantial' HIV risk Step 1. consider an incidence in a community/population of ≈ 3 per 100 person–years Step 2. Within a population with incidence ≈ 3% there will be significant heterogeneity. Not all people will have high HIV risk. Simple screening questions will help identify those at most risk within this population or community and those who are not using other effective HIV prevention methods Step 3 .Those who are identified at highest HIV risk and a would welcome and want to take an additional prevention option 'offering PrEP' could be considered. Defining ‘substantial risk’ • PrEP trials recruited populations at substantial risk of acquiring HIV infection, as defined by HIV incidence of >2 / 100 PY in control arms. • HIV incidence >2.0 per 100 person years was deemed sufficient to warrant offering oral PrEP in the recommendations by IAS-USA expert panel in 20141. • Modeling suggests that incidence >2-3/100 PY would be cost effective 1Marrazzo JM, del Rio C, Holtgrave DR, et al. HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society– USA Panel. JAMA 2014; 312:390–409. Defining ‘substantial risk’ HIV incidence in control arms of PrEP studies Study Population BKK TDF IDU FEM PREP Women VOICE Women iPrEx RCT MSM and TGW iPrEx Gap MSM and TGW iPrEx OLE MSM and TGW Partners Men and PrEP RCT women in SDC TDF2 Men and Women PROUD MSM Ipergay MSM Incident HIV Infections Person Years HIV Incidence Rate 95% CI 33 35 60 83 4823 n/a 1308 2113 0.7 5.0 4.6 3.9 0.47 to 0.96 n/a 3.5 to 5.9 3.1 to 4.8 43 1044 4.1 3.1 to 5.6 13 n/a 2.1 1.5 to 4.5 52 1578 2.0 n/a 24 n/a 3.1 n/a 19 14 214 n/a 8.9 6.6 6.0 to 12.7 n/a Van Damme NEJM 2012; Baeten NEJM 2012; Marrazzo NEJM 2015; Thigpen NEJM 2012; Choopanya Lancet 2013; Grant CROI 2013; Grant Lancet Infectious Diseases 2014. Where we are now ?from trials to implementation • Who will be offered PrEP? – What subgroups of population/s at 'substantial HIV risk' would benefit most – How to identify/screen for/target – Who in those groups would find acceptable/ most likely to use • PrEP delivery approaches and issues? – Where best to deliver PrEP • STI, FP, ANC/PNC, HIV, community… – Monitoring issues • Frequency of visits/follow up • Frequency of HIV re-testing for those on PrEP • How much screening for safety • How to deliver PrEP effectively? – How to support adherence to daily PrEP use – What does adherence to PrEP "mean" – how good is good enough – How to monitor adherence to PrEP? (differs from treatment) Implementation guidance • Identifying people at substantial risk – modelling and costing • Testing – options and in line with national testing algorithms, ?role of self- testing – Prior to offer – During taking • Pre-screening and monitoring – Renal – systematic review – (bone) – systematic review – Hepatitis B – systematic review • Drug resistance – systematic review • Issues for different populations – – – – – MSM Transgender PWID Sex workers AGYW – esp. adolescent specific issues Immediate issues to address • • • Making the case for PrEP, but not overselling it – Cost and cost-effectiveness – How does cost compare to other prevention options Defining and identifying the populations – Initial focus of the very high incidence populations – Screening tools for assessing risk Policy – How to support PrEP availability in countries – How to involve communities where PrEP programmes are planned to inform and empower them to choose – How to address legal issues and constraints • Social issues and human rights – Always within a comprehensive prevention programme – Always voluntary and informed Listening to and learning from communities “Young people need more than just PrEP tablets. They need social support to foster their self-esteem and motivation.” Ivan Fahy ShOUT! LGBT Youth Group (Ireland) "PrEP empowers me" Bathabile, 23 Zimbabwean sex worker on PrEP “If we continue to see sexual health as taboo, more unnecessary infections will occur.” Mark Josef Rapa University of Malta LGBT Society