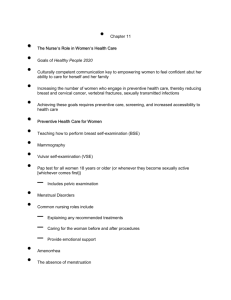
Disease Description & H&P Diagnosis and Diagnostic Study Clinical
advertisement

Disease Disease Primary Dysmenorrh ea Description & H&P H&P Menstrual pain associated with menstrual cycles in the absence of pathological findings – usually begins within 1-2 years after menarche. CC – Lower abdominal cramps, may radiate to back and groin and upper thighs HPI- o o pain often starts several hours before menses, and lasts 24-72 hours commonly associated symptoms - nausea, vomiting, diarrhea, backache, headache, fatigue, dizziness Diagnosis and Diagnostic Study Diagnosis and Diagnostic Study No testing necessary in many cases, depending on history and exam o potentially useful tests pregnancy test Pap smear cervical cultures (or polymerase chain reaction for gonococci and chlamydia) vaginal wet mount for bacterial vaginosis, trichomoniasis, candidiasis CBC or ESR for infection or inflammation urinalysis TSH o tests to consider in difficult cases pelvic ultrasound hysteroscopy hysterosalpingogram laparoscopy may be last resort Diagnosed By H&P Secondary Dysmenorrh ea o o o secondary dysmenorrhea menstrual pain associated with pelvic pathology symptoms usually begin after age 20-25 years in cases of secondary dysmenorrhea symptoms which may suggest secondary dysmenorrhea: dyspareunia menorrhagia; heavy menstrual flow suggests adenomyosis, myomas, polyps fever infertility suggests endometriosis, chronic inflammation Cervical Cultures to R/O pelvic infections Pelvic imaging to R/O presence of uterine fibroids or other anomalies Ultrasound or MRI Clinical Intervention and Clinical Therapies Clinical Intervention and Clinical Therapies Intervention Oral contraceptives Depot-medroxyprogesterone acetate; surgical laporatomy if marked disability Pharmacologic therapy non-steroidal anti-inflammatory drugs (NSAIDs) may reduce pain but increase neurological adverse events in women with primary dysmenorrhea (level 2 [mid-level] evidence) o insufficient evidence to guide selection of specific NSAID o dosing options include ibuprofen (Motrin, Advil) 800 mg orally 3 times daily, 600 mg orally every 6 hours, or 400 mg orally every 4 hours naproxen sodium (Anaprox) 550 mg orally twice daily mefenamic acid (Ponstel) 250 mg orally every 4-6 hours celecoxib (Celebrex) 400 mg initially then 200 mg orally twice daily o not recommended in advanced renal disease, hepatic insufficiency, nursing mothers Exercise Other Other Pain is produced by uterine vasoconstriction, anoxia and sustained contractions mediated by prostaglandins Disease Dysfunctiona l Uterine Bleeding: Heavy Menstrual Bleeding, hypermenorr hea; menorrhagia Description & H&P excessive menstrual blood loss which interferes with woman's physical, emotional, social and material quality of life(1) normal menstrual flow is 2-8 days(1) menstrual blood loss > 60-120 mL/period associated with anemia and iron depletion Causes: o potential causes in women with ovulatory cycles uterine fibroid (leiomyoma) increased fibrinolytic activity in endometrium increased prostaglandin levels o specific cause often not recognizable in heavy menstrual bleeding related to hormonal imbalance Chief concern (CC): o excessive menstrual blood loss which interferes with woman's physical, emotional, social and material quality of life(1) Past medical history (PMH): o features that may be more common in women with hemostatic disorder (such as von Willebrand disease) excess menstrual bleeding since menarche bleeding after dental extraction postoperative bleeding postpartum hemorrhage Social history (SH): o heavy menstrual bleeding associated with absence from work Diagnosis and Diagnostic Study Making the Diagnosis: history of excessive menstrual blood loss which interferes with woman's physical, emotional, social and material quality of life Differential diagnosis: o o bleeding disorders von Willebrand disease thrombocytopenia structural lesions uterine leiomyomata endometrial cancer cervical cancer cervical erosions cervical polyps vaginal lesions Diagnostic Testing CBC Coagulopathy testing hemostatic abnormalities may be common in women with menorrhagia at any age white women with menorrhagia may have increased prevalence of inherited bleeding disorders adolescents with menorrhagia may have abnormalities of platelet count or function Imaging- ultrasound (First Line); hysteroscopy (second line when Ultrasound inconclusive); sonohysterography Endometrial biopsy - used to rule out endometrial cancer or atypical hyperplasia o indications include o persistent intermenstrual bleeding o treatment failure in women > 45 years old - Clinical Intervention and Clinical Therapies o improvement in quality of life measures should be goal of any interventions o clarifying values and patient preferences may reduce hysterectomy rates for menorrhagia medications levonorgestrel-releasing intrauterine system (LNG-IUS) appears effective for heavy menstrual bleeding and is treatment of choice if o hormonal treatments are acceptable o at least 12 months use anticipated combined oral contraceptives is second-line drug treatment option either nonsteroidal antiinflammatory drugs (NSAIDs) or tranexamic acid (Lysteda) considered o second-line treatment option if either hormonal or non-hormonal treatments are acceptable preferred treatment option if hormonal treatments are not acceptable o tranexamic acid should not be used before LNG-IUS if long-term use is anticipated oral progestins (such as norethisterone 15 mg once daily on menstrual cycle days 5-26) or injected long-acting progestinsconsidered third-line treatment options danazol may be effective for heavy menstrual bleeding surgery/procedures surgery reduces menstrual bleeding at 1 year more than medical therapy, but levonorgestrel-intrauterine system improves quality of life as effectively as surgery endometrial ablation o preferable to hysterectomy in women with heavy menstrual bleeding alone and uterus ≤ 10 week pregnancy size o is effective for reducing heavy uterine bleeding in most women o preprocedure endometrial thinning may improve operative conditions and amenorrhea at 12 months referral for consideration of surgery or uterine artery embolization (UAE) as first-line treatment recommended for women with large fibroids and heavy menstrual bleeding and other significant Other Complications: o o anemia iron deficiency anemia Disease Description & H&P Diagnosis and Diagnostic Study Skin: o look for signs of bleeding disorders Abdomen: o inspect and palpate for abdominal and/or suprapubic mass Pelvic: o Vaginitis – Atrophic Vaginitis visual inspection for vulvar, vaginal or cervical lesions bimanual exam for uterine or adnexal mass, uterine enlargement or tenderness Description: o vaginal changes due to post-menopausal estrogen deficiency or other conditions associated with estrogen deficiency Also called: Diagnosis o usually a clinical diagnosis based on history and physical exam o diagnosis may be supplemented by vaginal pH and/or cytology Differential diagnosis: o o o urogenital atrophy vaginal atrophy Who is most affected: o post-menopausal women without estrogen replacement Causes: Lack of estrogen Risk Factors – anti estrogen medication; medroxyprogesterone, tamoxifen, danazol, leuprolide, nafarelin; cigarette smoking Associated conditions: o urinary tract symptoms (frequency, urge, dysuria)(1) o lower urinary tract infection(1) o pelvic organ prolapse History: Chief concern (CC): o Other symptoms such as dysmenorrhea or pressure symptoms UAE, myomectomy or hysterectomy should all be considered, discussed and documented when surgery for fibroid-related heavy menstrual bleeding is considered necessary vaginal hysterectomy preferred over abdominal hysterectomy after incorporating individual assessment dilation and curettage (D&C) should not be used as therapeutic treatment Physical: o Clinical Intervention and Clinical Therapies lack of vaginal lubrication o o superimposed microbially-induced vaginitis Candida vulvovaginitis bacterial vaginosis (BV) trichomoniasis contact reaction to irritants squamous cell carcinoma of cervix Diagnostic Testing o o o estrogen therapy (vaginal preferred due to limited systemic absorption) is primary treatment local estrogen therapy may be delivered by vaginal cream, ring, or tablet local estrogen therapy by various methods appear equally effective for reducing symptoms of vaginal atrophy (level 2 [mid-level] evidence) vaginal moisturizer or lubricant as supplement or alternative systemic (oral or transdermal) estrogen replacement may be recommended if osteoporosis or vasomotor symptoms Pathogenesis: o thin vaginal epithelium, with resultant glycogen and lactic acid deficiency Disease Description & H&P with coitus pruritus dyspareunia discharge may occur History of present illness (HPI): o o o o o menopause history of condition requiring antiestrogenic therapy o breastfeeding o use of certain personal hygiene products (for example, perfumes, powders, soaps, deodorants, panty liners, spermicides, lubricants containing irritants) Physical: Pelvic: o o o early stages vestibule thin and dry vagina mildly erythematous later stages loss of labial fat pad resutis in pendulous labia majora labia minora less distinct clitoral prepuce decreases, so clitoris may appear larger vagina loses elasticity and rugal folds vagina becomes shortened, narrower (introital stenosis) vagina easily traumatized possible associated findings urethral caruncle cystocele rectocele uterine prolapse Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other Disease vulvovaginal Candidiasis Description & H&P Chief concern (CC): Diagnosis and Diagnostic Study o most commonly presents as acute vulvar pruritus or vaginal discharge o vaginal irritation and soreness o vulvar burning o dyspareunia o external dysuria History of present illness diagnosis suspected in woman with symptoms (such as vaginal itching, vaginal discharge, or external dysuria) wet preparation (saline or 10% potassium hydroxide) or Gram stain of vaginal discharge showing yeasts, hyphae, or pseudohyphae culture or other test yielding positive results for a yeast species (HPI): o symptoms may be worse in week before menses Medication history: o ask about oral contraceptives antibiotic use corticosteroid use Past medical history (PMH): o ask about pregnancy diabetes mellitus immunosuppression Social history (SH): o ask about recent sexual history and behavior Physical: Pelvic: o o Bacterial vaginosis o vaginal exam may reveal thick white "cottage cheese-like" adherent discharge labial and vulvar erythema and swelling possible labial and vulvar fissure and pustulopapular peripheral lesions cervix normal on speculum exam polymicrobial infection of vulva and vagina may be asymptomatic typically presents with vaginal discharge Making the diagnosis: o clinical diagnosis using (Amsel criteria) requires 3 of the following homogeneous thin white or gray Clinical Intervention and Clinical Therapies o o do not treat if asymptomatic uncomplicated vulvovaginal candidiasis effective options include o numerous topical agents (butoconazole, clotrimazole, miconazole, nystatin, tioconazole, terconazole) o fluconazole (Diflucan) 150 mg orally in single dose oral and intravaginal antifungals appear to have similar effectiveness for uncomplicated vaginal candidiasis o addition of daily probiotics supplement to singledose fluconazole may further decrease symptoms of vulvovaginal candidiasis complicated vulvovaginal candidiasis (severe disease, infection not caused by Candida albicans, or infection in abnormal host) treat with topical agent for at least 7 days, or with fluconazole 150 mg orally every 72 hours (every 3 days) for 3 doses o topical boric acid or topical flucytosine may be effective against Candida glabrata vaginal boric acid and oral fluconazole may have similar efficacy for symptomatic outcomes in patients with diabetes o recurrent vulvovaginal candidiasis defined as > 4 symptomatic episodes within 1 year treat with topical or oral azole for 10-14 days initially o follow with suppressive therapy using fluconazole 150 mg orally in single dose weekly for 6 months o in pregnancy antifungal treatments for vulvovaginal candidiasis are FDA Pregnancy Category C except for nystatin vaginal tablets (Category A) and topical clotrimazole preparations (Category B) treatment for 7 days may be needed and topical imidazole may be more effective than nystatin) treat all symptomatic women first line therapy for nonpregnant women includes 1 of 3 antimicrobial regimens o metronidazole 500 mg orally twice daily for 7 days Other Prevention: o o consider fluconazole 150 mg orally as prophylactic treatment when giving systemic antibiotics or as maintenance therapy in especially susceptible patients(2) for maintenance treatment in recurrent vulvovaginal candidiasis(3) fluconazole 100-200 mg orally once weekly for 6 months considered firstline choice intermittent use of topical treatments is alternative Whiff test: o positive whiff test is presence of amine (fishy) odor of vaginal discharge Disease Description & H&P characterized by fishy odor o not a sexually transmitted disease o An overgrowth of Gardnerella and other aerobes Chief concern (CC): o o o o o o Trichomonia sis vulvovaginal itching or burning dyspareunia foul-smelling (musty or fishy) vaginal odor thin, gray-white vaginal discharge may be asymptomatic lack of perceived vaginal odor associated with unlikely diagnosis of BV women who have sex with women greatly affected History: Diagnosis and Diagnostic Study o o o in women motile T. vaginalis on wet mount of vaginal secretions culture for T. vaginalis if trichomoniasis suspected but not confirmed on wet mount other diagnostic tests o immuno-chromatographic assay test o nucleic acid probe test o polymerase chain reaction (PCR) test o transcription-mediated amplification test in men culture for T. vaginalis from urethral Other o discharge coating vaginal walls > 20% clue cells present on wet mount microscopy of vaginal discharge vaginal pH > 4.5 positive whiff test - fishy or amine odor of vaginal discharge alone or after addition of 10% potassium hydroxide (KOH) vaginal pH > 4.5 is most sensitive and amine odor most specific for BV Chief concern (CC): vulvar pruritus, burning, profuse vaginal discharge, rancid odor, postcoital bleeding(1, 2) o many women have little or no symptoms(1) o men may not have symptoms or may have symptoms of urethritis(1) Physical: Clinical Intervention and Clinical Therapies metronidazole gel 0.75% one full applicator (5 g) intravaginally once daily for 5 days o clindamycin cream 2% one full applicator (5 g) intravaginally once daily at bedtime for 7 days for pregnant women with symptoms - treat with 1 of 3 regimens o metronidazole 500 mg orally twice daily for 7 days o metronidazole 250 mg orally 3 times daily for 7 days o clindamycin 300 mg orally twice daily for 7 days recommended treatment includes 1 of o metronidazole 2 g orally in single dose o tinidazole 2 g orally in single dose alternative treatment - metronidazole 500 mg orally twice daily for 7 days o before or after addition of 10% potassium hydroxide (KOH) whiff test can also be positive with Trichomonas wet mount(3) perform wet mount preparation by 1 of 2 methods o dilute vaginal discharge with 1-2 drops of 0.9% normal saline solution, then place on slide with coverslip, or o place vaginal discharge into 2 mL test tube containing saline, then place on slide o examine slide microscopically using lower power (10X) and high dry power (40X) look for clue cells (vaginal epithelia coated with coccobacilli) consider microscopic exam of 10% potassium hydroxide (KOH) preparation to rule out vulvovaginal candidiasis(look for evidence of hyphae) Pathogenesis: o sexually transmitted disease o human host - lives only in vagina, Skene's ducts, male or female urethra (warm, moist areas) o attaches to walls of vagina, causes inflammation and discharge Likely risk factors: o loss of normal acidity of vagina Disease Description & H&P Pelvic: o profusely frothy, thin, foulsmelling, greenish-yellowto-gray, purulent, creamy vaginal discharge; vaginal tenderness, may have vulvar edema/erythema Diagnosis and Diagnostic Study o o o o o Pelvic Inflammato ry Disease (PID) o o infection of female upper genital tract many cases involve sexually transmitted organisms (for example, Neisseria gonorrhoeae, Chlamydi a trachomatis) often polymicrobial condition may include any combination of inflammatory disorders endometritis salpingitis pelvic peritonitis parametritis oophoritis pathogens - many cases are polymicrobial(1) Neisseria gonorrhoeae Chlamydia trachomatis endogenous pathogens (that is, not sexually transmitted) include History: Chief concern (CC): o o may be asymptomatic(1) symptoms, if present, may include(1, 2) lower abdominal pain Clinical Intervention and Clinical Therapies Other swab, urine, or semen pH testing of vaginal secretions whiff test wet mount of vaginal secretions culture for T. vaginalis of vaginal secretions in women if trichomoniasis suspected but not confirmed on wet mount of urethral swab, urine or semen in men pH testing of vaginal secretions elevated pH (> 4.5) common in trichomoniasis and bacterial vaginosis whiff test no historical, physical, or laboratory findings can conclusively diagnose PID laboratory studies may be normal in patient with PID abnormal laboratory studies may provide supportive but not confirmatory evidence definitive diagnosis, if needed, may require invasive testing, but treatment may be based on clinical findings alone in most cases no single test has adequate sensitivity and specificity to reliably diagnose or rule out PID additional criteria which support diagnosis include o oral temperature > 38.3 degrees C (> 101 degrees F) o abnormal cervical or vaginal mucopurulent discharge o presence of abundant white blood cells (WBC) on saline microscopy of vaginal fluid (wet mount) o elevated erythrocyte sedimentation rate o elevated C-reactive protein o laboratory documentation of cervical infection with Neisseria gonorrhoeae or Chlamydia trachomatis Diagnosing perform pregnancy test to rule out ectopic pregnancy o test for Neisseria gonorrhoeae and Chlamydia trachomatis(recommend male partner be tested) IV regimens 1 of following recommended regimens o cefoxitin 2 g IV every 6 hours or cefotetan 2 g IV every 12 hours, PLUS doxycycline 100 mg orally or IV every 12 hours continue initial regimen until at least 24 hours after clinical improvement after discharge continue oral therapy withdoxycycline 100 mg orally every 12 hours to complete 14 days of therapy if tuboovarian abscess, consider adding clindamycin ormetronidazol e to doxycycline for more effective anaerobic coverage o clindamycin 900 mg IV every 8 hours, PLUSgentamicin loading dose 2 mg/kg IV or intramuscularly, then maintenance dose 1.5 mg/kg every 8 hours gentamicin once daily may be as effective but not studied in PID (see Single-daily dosing of aminoglycosides) continue initial regimen until at least 24 hours after clinical improvement after discharge continue oral therapy withclindamycin 450 mg orally 4 times daily or switch to doxycycline 100 mg orally every 12 hours to complete 14 days of therapy if tuboovarian Pathogenesis: nearly all cases are from ascending infection of bacteria from the endocervix risk for PID correlates with risk for acquiring new sexually transmitted diseases aged < 25 years in 75% cases and 10 times increased risk single status, divorce, separation earlier age at first intercourse and increasing number of male sex partners Differential to include o ectopic pregnancy o ovarian torsion o appendicitis Disease Description & H&P or pelvic pain fever abnormal vaginal discharge or bleeding, itching or odor dyspareunia back pain vomiting History of present illness (HPI): o ask about sexual history, including risks for sexually transmitted diseases o ask about date of last menstrual period to assess for possibility of ectopic pregnancy o ask about quality of pain (absence of migration of pain may suggest PID over appendicitis) o ask about procedures involving uterine instrumentation that may cause postsurgical PID, such as pregnancy termination intrauterine device insertion within previous 6 weeks hysterosalpingography intrauterine insemination in vitro fertilization Physical: General physical: o fever may occur Abdomen: o lower abdominal tenderness and rebound tenderness may be present bilateral abdominal tenderness may suggest PID over appendicitis Pelvic: o assess for Diagnosis and Diagnostic Study o o o o inflammatory markers which may support diagnosis of PID white blood cell count (WBC) erythrocyte sedimentation rate C-reactive protein wet mount of vaginal fluid may show WBC transvaginal ultrasound is imaging modality of choice in initial evaluation of pelvic pain for cases requiring more definitive evaluation other diagnostic alternatives include computed tomography magnetic resonance imaging laparoscopy Clinical Intervention and Clinical Therapies abscess, clindamycinrecommende d instead ofdoxycycline for more effective anaerobic coverage alternative regimen - ampicillin-sulbactam 3 g IV every 6 hours PLUS doxycycline 100 mg orally or IV every 12 hours (effective coverage against Chlamydia trachomatis, Neisseria gonorrhoeae and anaerobes and for patients who have tuboovarian abscess) Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other o tenderness on bimanual exam of cervix, uterus or adnexa (usually described as cervical motion tenderness or adnexal tenderness) cervical discharge cervical friability pelvic mass findings may be mild with Chlamydia o Breast Mass o most breast masses are benign (most commonly fibroadenoma), but breast mass associated with increased risk of breast cancer in postmenopausal women History: History of present illness (HPI): o o ask about duration of mass change in mass size changes related to menstrual cycle ask about related symptoms breast tenderness or swelling history of fever nipple discharge o pathologic cause more likely if patient > 50 years old, or discharge is bloody, bloodcontaining, watery, unilateral, spontaneous, or involves a single duct o physiologic cause more likely with initial evaluation imaging for palpable breast mass for women ≥ 40 years old mammography is recommended study but ultrasound may be appropriate initial study if had mammography in previous 6 for women 30-39 years old - either mammography or ultrasound of breast for women < 30 years old - ultrasound of breast followed by mammography if o ultrasound suspicious for malignancy o ultrasound is negative or does not correlate with palpable mass o if the clinical examination or other risk factors are concerning Magnetic resonance imaging: o o magnetic resonance imaging (MRI) may be useful for detection of breast lesions in high risk patients, including those with(1, 2, 3) silicone breast implants prior breast conserving surgery known carcinoma axillary metastasis and unknown primary site extra dense breast tissue magnetic resonance imaging plus clinical exam and mammogram may be more sensitive than ultrasound plus clinical exam and mammogram to rule out malignancy in women with suspected invasive breast cancer o o o aspiration of painful cyst may be adequate if simple cyst, no residual mass, and no bloody aspirate if initial ultrasound and/or mammogram demonstrate specific benign findings such as simple cyst or lymph node, further evaluation not necessary if suspicious for malignancy on clinical exam or imaging core needle biopsy associated with higher diagnostic accuracy for detection of breast cancer than fine needle aspiration cytology in patients with palpable breast masses consider triple test score o clinical exam, imaging, and tissue sampling each scored 1 for benign, 2 for suspicious, and 3 for malignant o triple test score validated to be accurate for diagnosing breast cancer if score ≥ 6 and rule out breast cancer if score 3-4 o excisional biopsy recommended if triple test score 5 Benign causes of breast mass: o infection and inflammation mastitis cellulitis abscess chronic infections from mycobacteria or parasites (such as filariasis) mammillary duct fistula sarcoidosis foreign bodies o solid, non-inflammatory lump fibroadenoma of breast (most common) benign cyst Malignant and premalignant causes of breast mass: o o o o breast cancer in women breast cancer in men ductal carcinoma in situ (DCIS) lobular carcinoma in situ Disease Description & H&P o o discharge that is bilateral, multiduct, multicolored or milky, sticky, and occurs with stimulation ask about history of breastfeeding and current lactation status ask about hormonal medication use prior or current use of oral contraceptives estrogen or hormone replacement therapy ) Past medical history (PMH): o o findings that may be associated with higher risk for breast cancer include family history of breast cancer postmenopausal hormone replacement therapy (HRT) contralateral breast cancer cancer of uterus or ovary atypical hyperplasia breast carcinoma in situ radiation therapy to chest ask about prior breast mass or biopsy recent breast trauma or surgery Family history (FH): o ask about breast cancer in firstdegree relatives mother, sister, or daughter with history of Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other breast or ovarian cancer before age 50 years or positive test for mutated breast cancer genes (if so, considerBRCA mutation testing) Physical: General physical: o Breast Cancer fever and chills may be indicative of infection (such as mastitis) breast cancer classified as carcinoma in situ (noninvasive carcinoma, stage 0) if cancer cells contained within duct (ductal carcinoma in situ) or lobule (lobular carcinoma in situ) invasive breast cancer (infiltrating breast cancer, stages I-IV) if cancer cells spread beyond basement membrane of duct or lobule to adjacent breast parenchyma o invasive breast cancer classified as(6, 7) early breast cancer stages I, IIa, IIb o no tumor extension to chest wall or skin o can include movable ipsilateral axillary lymph node metastases o no distant metastases locally advanced breast cancer - stages IIIa, IIIb, IIIc - any of the following without distant metastases o metastases in ipsilateral axillary lymph nodes that diagnosis of invasive breast cancer is based ontriple assessment, which includes findings on clinical assessment include o palpable breast mass o palpable lymph nodes o skin and/or nipple changes findings on mammography (with or without ultrasound) include o microcalcifications o spiculated opacities o nonpalpable lesions in ipsilateral or contralateral breast o solid masses that correlate with physical exam findings o adenopathy o architectural distortion tissue sampling - core needle biopsy and/or fine needle aspiration cytology o excisional biopsy used for equivocal cases o types of invasive breast cancer are distinguished based on pathology Differential diagnosis: o o o o o fibroadenoma ductal carcinoma in situ lobular carcinoma in situ if pain fibrocystic changes dorsal radiculitis Tietze syndrome (inflammation in costochondral junction) mastitis if nipple discharge(1) intraductal papilloma duct ectasia Early invasive breast cancer: o initial treatment options include breast-conserving surgery (lumpectomy) followed by radiation therapy to breast o breast-conserving surgery (plus radiation therapy) for early breast cancer appears as effective for survival and rate of distant metastases as mastectomy, but may be associated with need for re-excision or future mastectomy o neoadjuvant (preoperative) chemotherapy may be used for large tumors to improve resectability o adjuvant radiation therapy after breastconserving surgery may reduce 10-year recurrence risk and 15-year breast cancer-related mortality o o mastectomy indicated for patient preference, or if large or multicentric tumor precludes breast conservation therapy for Paget's disease of breast, central lumpectomy may result in similar 15-year breast cancer-specific survival as sentinel lymph node (SLN) biopsy is preferred method of axillary lymph node assessment for staging of early breast cancer with no clinical evidence of lymph node involvement adjuvant systemic therapy endocrine therapy for hormone receptorpositive tumors o tamoxifen (Nolvadex) 20 mg/day for 5 years recommended for premenopausal women and appears to histopathologic types of breast carcinomas in situ carcinomas o ductal carcinoma in situ (DCIS) o lobular carcinoma in situ (LCIS) incidental finding of microscopic abnormal tissue growth in lobules of breast does not progress to cancer, but associated with increased risk of subsequent invasive breast cancer in either breast invasive carcinomas o ductal o inflammatory clinical diagnosis associated with diffuse skin edema, skin and breast erythema (peau d'orange), firmness of underlying tissue without Disease Description & H&P are clinically fixed or matted o metastases in clinically detected internal mammary lymph nodes o tumor > 5 cm and metastases in movable ipsilateral axillary lymph nodes o tumor with direct extension to chest wall or skin advanced breast cancer - stage IV (distant metastases) Diagnosis and Diagnostic Study o Clinical Intervention and Clinical Therapies partial duct obstruction hyperprolactinemia fat necrosis History: Chief concern (CC): o o breast mass can present as breast pain History of present illness (HPI): ask about palpable breast mass including o duration of mass o changes in size of mass o changes related to menstrual cycle nipple discharge o pathologic cause more likely if patient > 50 years old, or discharge is bloody, bloodcontaining, watery, unilateral, spontaneous, or involves a single duct o physiologic cause more likely with discharge that is bilateral, multiduct, multicolored or milky, sticky, and occurs with o o reduce recurrence risk and all-cause mortality over 15 years o for postmenopausal women options which may reduce recurrence risk compared to tamoxifen alone include tamoxifen for 2-3 years followed by aromatase inhibitors for 2-3 years for total 5 years aromatase inhibitor monotherapy for 5 years trastuzumab (Herceptin) for human epidermal growth factor receptor type 2 (HER2)-positive tumors may increase overall survival and disease-free survival but may increase risk for heart failure chemotherapy o decision to use chemotherapy should be individualized, especially if favorable prognosis where absolute benefit is small o combination chemotherapy for early breast cancer may reduce 15-year allcause mortality, breast cancer mortality, and recurrence risk bisphosphonates bisphosphonates (as a drug class) may not be associated with reduced rates of recurrence or bone metastases in patients with early breast cancer; clodronate and zoledronic acid each have mixed results in large randomized trials bisphosphonates may not decrease fracture rate but may decrease bone loss so recommended if osteoporosis along with lifestyle interventions, calcium, and vitamin D to reduce risk for bone loss Locally advanced breast cancer: for locally advanced breast cancer including inflammatory breast cancer - treatment includes neoadjuvant chemotherapy surgery o for noninflammatory disease mastectomy or breast-conserving therapy o for inflammatory disease - mastectomy radiation therapy endocrine therapy if hormone receptorpositive, including use in neoadjuvant therapy Other o o o o o palpable mass involving ≥ one-third of breast findings due to tumor embolization to dermal lymphatics and engorgement of superficial capillaries classified as T4d for staging so stage III or IV on presentation associated with poor prognosis does not apply to locally advanced cancer presenting late in course of disease and with skin involvement medullary, not otherwise specified medullary with lymphoid stroma mucinous (colloid) if < 1 cm, has very low incidence of axillary lymph node metastases, but sentinel lymph node biopsy may be appropriate papillary (predominantly micropapillary pattern) tubular - if < 1 cm, has very low incidence of axillary lymph node Disease Description & H&P stimulation breast pain - ask about location, severity, and relationship to menstrual cycle or physical activity skin changes ask about hormonal medication use o prior or current use of oral contraceptives o estrogen or hormone replacement therapy breast pain without other symptoms not associated with increased risk of breast cancer Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other addition of HER2 inhibitor (such as trastuzumab) if HER2-positive, including use in neoadjuvant therapy Advanced breast cancer: o o o for advanced (metastatic) breast cancer chemotherapy recommended for women with triple-negative tumors (HER2, estrogen receptor, and progesterone receptor), symptomatic or rapidly progressive organ metastases, or disease refractory to hormone therapy combination chemotherapy associated with increased survival and time to progression compared to single-agent chemotherapy, but may increase adverse effects taxane-containing regimens may improve overall survival, time to progression, and overall response compared to some other chemotherapy regimens chemotherapy agents which may improve survival or progression-free survival in women with advanced breast cancer which progresses on first-line therapy include eribulin (Halaven), everolimus (Afinitor), and ixabepilone (Ixempra) for HER2-positive advanced breast cancer trastuzumab (Herceptin) may improve survival but associated with increased risk of cardiac dysfunction addition of lapatinib (Tykerb) to paclitaxel (or to letrozole) may increase progressionfree survival addition of pertuzumab (Perjeta) to trastuzumab plus docetaxel increases progression-free survival (level 1 [likely reliable] evidence) endocrine therapy for hormone receptor-positive advanced breast cancer endocrine therapy associated with similar survival rates compared to chemotherapy for initial treatment of hormone receptorpositive metastatic breast cancer; endocrine therapy may be preferred due to better tolerability, except in rapidly progressive disease aromatase inhibitors (anastrozole, letrozole, exemestane) may have survival benefit over other endocrine therapies in postmenopausal women with advanced breast cancer o o o metastases, but sentinel lymph node biopsy may be appropriate o lobular o undifferentiated o squamous cell o adenoid cystic o secretory o cribiform microinvasive carcinoma invasive carcinoma with no focus of tumor cells > 1 mm typically occurs with DCIS or LCIS with small foci of tumor cells beyond basement membrane rarely occurs without noninvasive disease Paget's disease exudate or crust of nipple and areola caused by infiltration of epidermis by noninvasive breast cancer epithelial cells can occur with noninvasive disease (usually DCIS, rarely LCIS) or with invasive disease (infiltrating) breast sarcomas account for < 1% of all primary breast malignancies usually occur in women ages 40-60 years most common types include o angiosarcoma o malignant fibrous histiocytoma o stromal sarcoma other types can include o phyllodes tumor (includes epithelial component) Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o o o o o o o o preferred first-line therapy is anastrozole 1 mg orally once daily or letrozole 2.5 mg orally once daily, alternative is tamoxifen 20-40 mg/day orally endocrine therapies used for disease progression after first-line therapy include exemestane 25 mg orally once daily or fulvestrant (Faslodex) 250 mg intramuscularly once monthly bisphosphonates (oral or IV) may reduce risk of skeletal events in women with advanced breast cancer and clinically evident bone metastases may not reduce risk of skeletal events in women with advanced breast cancer without prior bone metastasis appear effective for pain relief in painful bone metastases denosumab (Xgeva) may reduce risk for skeletal-related events more than bisphosphonates in women with breast cancer and bone metastases ) low-molecular-weight heparin (LMWH) reduces symptomatic venous thromboembolism (VTE) ) and possibly 2-year mortality in patients with advanced cancer surgical resection of primary tumor associated with increased survival in retrospective studies of patients with advanced breast cancer Recurrent breast cancer: breast-conserving surgery for recurrent ipsilateral breast cancer may be associated with worse survival compared to mastectomy limited evidence regarding adjuvant systemic therapy for women with isolated locoregional recurrence following primary treatment of operable breast cancer Surveillance after primary cancer treatment: mammography surveillance might improve overall survival and breast cancer-specific survival breast magnetic resonance imaging (MRI)appears more accurate than clinical exam, mammogram, and ultrasound for detection of breast cancer recurrence more intensive approaches to follow-up (addition of chest x-ray and bone scan) may improve disease-free survival but not overall survival compared with regular physical exams and Other o o o o o fibrosarcoma liposarcoma leiomyosarcoma spindle-cell sarcoma rhabdomyosarcom a Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other yearly mammography in women with early breast cancer Cystocele descent of pelvic organs toward or through the vaginal opening due to loss of connective tissue support in ≥ 1 of the following anatomic locations anterior vaginal wall o most common o usually involves bladder prolapse (cystocele) posterior vaginal wall o usually involves rectal prolapse (rectocele) o may involve small intestine (enterocele) vaginal apex o usually involves prolapse of uterus, cervix, or posthysterectomy prolapse of vaginal cuff (vault prolapse) o may involve small intestine (enterocele), colon (sigmoidocele), or bladder (cystocele) Also called: o o o o o o o pelvic relaxation urogenital prolapse uterovaginal prolapse uterine prolapse cystocele rectocele enterocele Chief concern (CC): o most women are asymptomatic symptoms vary by position of uterus and pressure on surrounding pelvic structures, and may not correlate with stage or o Making the diagnosis: o o o o o diagnosis usually made clinically by pelvic exam during routine well-woman evaluation or in women with symptoms of pelvic organ prolapse such as vaginal bulge and incontinence seeing or feeling vaginal bulge with tissue prolapsing to or past vaginal opening considered most specific symptom for pelvic organ prolapse grading systems used to standardize findings on physical exam Baden-Walker grading system commonly used in clinical practice to evaluate anterior, apical, and posterior pelvic floor support defects Grade Description 0 1 o o No prolapse Normal position for each pelvic site o Prolapse halfway to hymen o Prolapse to hymen o Prolapse halfway past hymen o Maximum descent possible for each pelvic site 2 3 4 Baden-Walker Grading System: Pelvic Organ Prolapse Quantification (POP-Q) staging system o developed by the International Continence Society (ICS), the American Urogynecologic Society (AUS), and the Society of Gynecologic Surgeons (SGS) o commonly used for clinical research purposes o conservative management consider watchful waiting in asymptomatic or mildly symptomatic women with early stage prolapse without descent beyond hymen pelvic floor muscle training (Kegel exercises) o characterized by systematic contraction of pelvic floor muscles by conscious contraction, electrical stimulation, or biofeedback training o often used adjunctively to symptomdirected therapy such as pessaries o pelvic floor muscle training may improve prolapse symptoms in women with pelvic organ prolapse mechanical support (pessary) o consider pessary use in all women with symptomatic prolapse prior to surgical intervention o pessary selection usually determined by severity of prolapse and patient's cognitive status, manual dexterity, and level of sexual activity o pessary use reported to help resolve most prolapse symptomsat 2 months in women with symptomatic pelvic organ prolapse surgical management surgical correction usually delayed in premenopausal women until all anticipated childbearing has been completed women presenting with cervical lesions or other evidence of cervical disease should be evaluated and treated prior to prolapse repair surgical approach to pelvic organ prolapse is either reconstructive or obliterative o reconstructive approach goal of reconstructive surgery is correction of pelvic prolapse and relief of associated symptoms while maintaining sexual function procedures may be performed by vaginal, abdominal, or laparoscopic approach (vaginal Differential diagnosis: o o o o o uterine leiomyoma prolapsed submucosal myoma may present as vaginal bulge or pressure bladder diverticula presenting as vaginal bulge in 2 patients in case series editorial can be found in , commentary can be found in primary invasive vaginal carcinoma presenting as irreducible third degree uterovaginal prolapse in 60year-old woman in case report Skene gland abscess presenting as painful periurethral mass in case report urethral leiomyoma presenting as exophytic periurethral mass in 27year-old woman in case report Disease Description & H&P o severity of prolapsed may present with ≥ 1 of the following vaginal symptoms o sensation of or visible bulge or protrusion from vagina (considered only symptom specific to pelvic organ prolapse) o pelvic pressure or heaviness o feeling of something "falling out" of vagina urinary dysfunction o stress incontinenc e o frequency o urgency o obstructed voiding, including weak or prolonged urinary stream urinary hesitancy feeling of incomplete emptying bowel dysfunction o incontinence of flatus or liquid or solid stool o straining during defecation o urgency o sense of blockage or obstruction during defecation o feeling of incomplete emptying o manual pressure (splinting) on perineum or vagina to begin or complete defecation (more Diagnosis and Diagnostic Study Stage Description No prolapse (anterior and posterior points all -3 cm, and cervix [C] or posterior fornix [D] is between TVL and TVL 2 cm) Prolapse > 1 cm above hymen (< -1 cm) and criteria for stage 0 not met Prolapse ≤ 1 cm above or below hymen (at least 1 point is -1, 0, or +1) Prolapse > 1 cm below hymen Most distal prolapse ≤ 2 cm less than TVL 0 I II III IV Clinical Intervention and Clinical Therapies Complete eversion of lower genital tract Most distal prolapse TVL - 2 cm beyond hymen Abbreviation: TVL, total vaginal length. Pelvic Organ Prolapse Quantification (POP-Q) Staging System: o approach accounts for 80%-90% of procedures) reconstructive surgery may involve hysterectomy or may preserve the uterus mesh may be used as a surgical adjuvant in reconstructive procedures obliterative approach goal of obliterative surgery is to correct pelvic prolapse by partial or total closure of vaginal canal colpocleisis usually reserved for elderly women who are at high risk for complications with reconstructive procedures prefer to avoid hysterectomy do not desire to maintain vaginal use for intercourse Other Disease Description & H&P o common with posterior vaginal prolapse) o digital evacuation to complete defecation dyspareunia rarely painful but patients may mistakenly attribute other sources of pelvic and/or low back pain to prolapsed History of present illness (HPI): o o sensation of or actual vaginal bulging may vary over time may be asymptomatic or mildly symptomatic in the morning with protrusion worsening throughout the day may be worse after excessive standing, heavy lifting, coughing, or physical exertion may progress with increasing body mass index but not reversed by weight loss symptoms of urinary dysfunction may change with disease severity stress urinary incontinence may occur with mild prolapse and improve or resolve as prolapse progresses beyond hymen women with prolapse beyond hymen more likely to report symptoms of obstructed voiding, including position change and/or manual Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other pressure on prolapsed area (splinting) to begin or complete urination Menopause Description: o o normal physiological event cessation of menstrual periods, but menopausal symptoms often occur before menopause Definitions: o menopause - cessation of menses o reproductive stage - from menarche (first menstrual period) to beginning of perimenopause (when cycles become variable) o perimenopausal - time around menopause during which menstrual cycle and endocrine changes are occurring, including first 12 months without periods o postmenopausal - begins at time of final menstrual period, overlapping with perimenopause by 12 months o menopausal transition climacteric - time from late reproductive stage into postmenopause Who is most affected: o o o average age 51 (2 years earlier in smokers) median onset of perimenopause 45.5-47.5 median age of natural menopause 51.4 based on crosssectional study of 14,620 women aged 40-55 years risk factors for earlier age of menopause were current smoking, lower educational o history of no menstrual period for 1 year in women > 45 years old generally accurate for diagnosis o some physicians order follicle-stimulating hormone (FSH) to confirm diagnosis earlier o perimenopause should be diagnosed based on menstrual history and age, laboratory testing unnecessary; best predictors that menopause will occur within 4 years, based on prospective cohort studies age > 50 years amenorrhea for 3-11 months menstrual cycle irregularity within 12 months follicle-stimulating hormone (FSH) normal range o child < 4 milli-units/mL o reproductive period 6-10 milli-units/mL o perimenopause 14-24 milli-units/mL o menopausal > 30-40 milli-units/mL single FSH value unreliable in perimenopausal years; serial FSH levels needed o o use of estrogen (hormone replacement therapy [HRT]) primary reasons for considering estrogen are o symptom relief - described here o prevention of osteoporosis risks may outweigh benefits for long-term use of HRT estrogen should NOT be used for cardiovascular disease prevention treatments for alleviation of menopausal symptoms vasomotor symptoms o estrogen proven to reduce vasomotor symptoms o phytoestrogens may reduce hot flash severity or frequency in women with vasomotor menopausal symptoms, insufficient data to define effective phytoestrogen supplements but extracts containing genistein ≥ 30 mg/day have most supportive evidence o other treatments shown in randomized trials to reduce vasomotor symptoms include progestogens in high doses (but rarely given without estrogens) tibolone (Livial), not available in United States clonidine venlafaxine (Effexor) paroxetine (Paxil) gabapentin St. John's wort urogenital symptoms o vaginal lubricants o estrogen reduces symptoms of urogenital atrophy o tibolone improves libido and vaginal lubrication o testosterone improves sexual enjoyment and libido estrogen shown to improve quality of life in short-term trials estrogen reduces depressive symptoms in Causes: o physiologic process of ovarian failure, oocyte depletion Pathogenesis: o decreased estradiol-17beta secretion by ovarian follicles o decreased sex hormone binding globulin (SHBG) leads to increased free testosterone o hot flushes may be due to acute lowering of hypothalamic setpoint from estrogen withdrawal o hypothalamic-pituitary insensitivity to estrogen may occur in perimenopausal women diethylstilbestrol (DES) exposure in utero associated with increased lifetime risk of early menopause Complications: o most menopausal symptoms (for example, hot flushes) usually resolve with time o genital atrophy may be chronic o perimenopausal transition may be associated with increased risk for new depressive symptoms Differential diagnosis: o o o pregnancy hypothyroidism, hyperprolac tinemia primary ovarian insufficiency (POI), Savage syndrome (no receptors on ovary), autoimmune oophoritis Disease Description & H&P o o o o o o o o attainment, being separated/widowed/div orced, nonemployment and history of heart disease; risk factors for later age of menopause were parity, prior use of oral contraceptives, and Japanese race Chief concern (CC): hot flush (vasomotor instability) then cold sweat (night sweats) urogenital symptoms vaginal dryness, vaginal irritation, dyspareunia, decreased sexual pleasure, dysuria, frequency, urgency, suprapubic pain psychologic symptoms mood swings (emotional lability), difficulty concentrating, apathy urinary incontinence NOT associated with menopausal transition History of present illness (HPI): secondary amenorrhea, by definition up to 90% women have altered menstrual pattern during perimenopause (510 years) self-limited appearance of increased scalp hair loss (perhaps related to synchronous hair shedding and asynchronous replacement) anovulation associated with irregular cycle intervals and bleeding duration but not with heavy bleeding o novulation associated with Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies postmenopausal women health recommendations upon reaching menopause health recommendations regarding cardiovascular disease prevention health recommendations regarding osteoporosis prevention o increased dose recommendations for calcium and vitamin D - calcium 1,2001,500 mg/day and vitamin D 400-800 units/day o weight-bearing exercise o only medications proven definitively to prevent fractures are bisphosphonates (alendronate, risedronate) o other medications which may prevent fractures include estrogen, calcitonin and sodium fluoride o for details, see Osteoporosis andCalcium and vitamin D for treatment and prevention of osteoporosis o cognitive behavior therapy (delivered by group or self-help approach) may reduce overall problem rating of hot flushes and night sweats in menopausal women o alternative therapies may be effective Diet: o calcium 1,200-1,500 mg/day and vitamin D 400-800 units/day recommended calcium citrate has best absorption, and may be preferred if o achlorhydria o constipation or gas with calcium carbonate o history of renal stones calcium carbonate (CaCO3) is cheaper, and absorption can be improved by taking with fruit (acid) role of calcium in peri- and postmenopausal women based on consensus opinion of The North American Menopause Society can be found in Menopause 2001 Mar/Apr;8(2);84 o flaxseed 40 g/day reduced total and highdensity lipoprotein (HDL) cholesterol compared with wheat germ placebo based on 1-year randomized trial of 199 menopausal women differences were not clinically significant o Other Disease Description & H&P o short cycles (< 21 days) o long cycles (> 36 days) o short duration of menstrual bleeding (1-3 days) o long duration of menstrual bleeding (> 8 days) heavy bleeding associated with o baseline leiomyomata o overweight o obesity o hysterectomy accelerates menopause by 3-5 years postsurgical menopause more severe o smoking accelerates menopause by 3-5 years and also increases severity of symptoms estradiol converted to antiestrogen 2hydroxy-estradiol Physical: General physical: o if seen during hot flush, may observe flushed face and anterior chest wall for about 90 seconds Skin: o thin elastic skin, increased facial hair, thin brittle nails Pelvic: o o pelvic relaxation vagina - decreased secretions, pale thin epithelium, loss of rugae, vulvar/vaginal atrophy cervix - decreased secretions o Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies and no significant differences in menopausal symptoms Reference - J Clin Endocrinol Metab 2005 Mar;90(3):1390 in BMJ 2005 May 7;330(7499):1094 o omega-3 fatty acids may not alleviate symptoms of depression in middle-aged women (level 2 [mid-level] evidence) based on randomized trial without intentionto-treat analysis 120 patients with moderate-to-severe depression randomized to ethyleicosapentaenoic acid 0.15 g plus ethyldocosahexaenoic acid 0.15 g daily vs. placebo for 8 weeks depression improved in both groups but no significant difference between treatments omega-3 fatty acids beneficial in patients with moderate depression based on subgroup analysis o Prempro FDA approved in lower dose with ethinyl estradiol 0.45 mg and medroxyprogesterone 1.5 mg o Premarin 0.45 mg dose FDA approved for vasomotor symptoms associated with menopause and symptoms of vulvar and vaginal atrophy transdermal estradiol 0.03% gel may reduce frequency and severity of hot flushes in postmenopausal women o one frequently used progestin is medroxyprogesterone acetate (Provera, generic) but not specifically indicated for reduction in vasomotor symptoms o micronized progesterone 300 mg orally once daily associated with reduction in hot flashes and/or night sweats in 12-week randomized placebo-controlled trial in 133 healthy postmenopausal women, allocation concealment not stated megestrol acetate (Megace) 20 mg twice daily can reduce hot flashes up to 80% but may cause weight gain testosterone may improve sexual motivation addition of testosterone to hormone therapy may improve sexual desire and satisfying sexual activity in peri- and postmenopausal women Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Non-hormonal therapies: o systematic reviews of nonhormonal therapies for hot flashes treatments with evidence for efficacy o selective serotonin reuptake inhibitors (SSRI) or serotonin norepinephrine reuptake inhibitors (SNRI) antidepressants o SSRIs reduce frequency and severity of hot flashes in menopausal and postmenopausal women o venlafaxine extended-release 75 mg/day may reduce effect of hot flashes o desvenlafaxine 100-200 mg/day may modestly reduce number of hot flushes in postmenopausal women clonidine Clonidine (Catapres): o clonidine 0.1-0.2 mg twice daily 2 randomized trials with 96 women found clonidine more effective than placebo for reducing hot flushes side effects - orthostatic hypotension, dizziness, blurred vision, constipation, dry mouth contraindications - hypotension, coronary insufficiency, cerebrovascular disease, chronic renal failure gabapentin Gabapentin (Neurontin): o gabapentin may modestly reduces hot flashes with adverse effects o gabapentin may be as effective as estrogen but with more side effects o gabapentin associated with increased rate of headache, dizziness and disorientation o treatments with limited or inconsistent evidence for efficacy o isoflavones o black cohosh o vitamin E Eszopiclone (Lunesta): eszopiclone (Lunesta) may reduce insomnia and possibly menopausal symptoms in Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other women with perimenopausal-onset insomnia Phenobarbital/belladonna/ergotamine o (Bellergal): Bellergal-S (phenobarbital 40 mg, ergotamine 0.6 mg, belladonna 0.2 mg) 1 tablet orally twice daily may be addictive not highly effective sedating contraindications - alcohol or drug dependence, asthma, urinary retention Intrauterine Pregnancy o most common signs and symptoms are due to hormonal changes of pregnancy - estrogen, progesterone, human chorionic gonadotropin (hCG), human placental lactogen (hPL), relaxin, prolactin, increased renin and angiotensin o serum human chorionic gonadotropin (hCG) is positive even before missed period, see Pregnancy testing for details Comment Test Value s Decreas Albumin e General symptoms: o amenorrhea commonly the initial symptom see Pregnancy testing o weight gain ideally 25-35 lbs (11.516 kg) see Weight gain in pregnancy o fatigue worse in first trimester, improves in second trimester sleep alterations HEENT symptoms: o tender, bleeding gums may appear in second month of pregnancy and worsen until 1 month before delivery will regress following Bicarbonate Decreas e Dilutional effect Compensat ory to respiratory alkalosis pO2 General Physical: o o o use acetaminophen (Pregnancy Category B) avoid NSAIDs NSAIDs (including COX-2 inhibitors) affect fetal kidneys and ductus arteriosus aspirin is Pregnancy Category C in doses < 150 mg/day and Pregnancy Category D in standard doses NSAIDs are Pregnancy Category B in first and second trimesters, but Pregnancy Category D in third trimester Headache: o Unchang ed may be due to increased blood flow and swelling of sinus drainage tracts, fatigue, tension or eye strain o relaxation and warm compresses may help with symptom relief o acetaminophen may be needed o if dizziness, blurred vision, or scotomata, consider pregnancy-induced hypertension Breast pain: Increase support bra acetaminophen Heartburn (reflux): Blood gases (arterial) pH Analgesia: o o o o pCO2 reduced blood pressure (mean 105/60 mm Hg) result of reduced systemic vascular resistance and smooth muscle relaxation caused by progesterone gradual return to normal blood pressure in third trimester Skin: Decreas e Mild respiratory alkalosis Decreas Increased BUN o o o progesterone leads to relaxation of lower esophageal sphincter and reduced bowel motility especially in first trimester, while expanding uterus displaces stomach in third trimester frequent small meals avoid lying recumbent after eating, sleep with head elevated avoid overeating, spicy foods, fried foods, gasproducing foods (cabbage, Brussels sprouts, o darkening of linea alba (linea nigra), areola, axillae, perineum and inner thighs all attributed to melanocytic stimulation by estrogen and progesterone extensive abdominal hyperpigmentation in woman of dark skin color in case report chloasma - "mask of pregnancy" occurs in up to 75% of pregnant women reddish brown color may develop over bridge of nose and under eyes usually resolves in 1 year, but sometimes not Disease Description & H&P delivery nasal congestion and nosebleeds - from estrogen and progesterone-mediated perivascular edema o headaches common related to sinus congestion, tension, fatigue Breast symptoms: Diagnosis and Diagnostic Study e GFR Calcium Decreas e Due to decreased albumin Cholesterol Increase Creatinine Decreas e Increased GFR Creatinine clearance Increase Increased GFR Increase Lower renal threshold Decreas e Dilutional and increased use by growing fetus Transferrin Increase Greater iron absorption due to increased requiremen t Magnesium Decreas e o o breast tenderness, swelling, tenderness, tingling, heaviness o common in first 8 weeks post-conception o due to increasing amount of beta-hCG, estrogen, progesterone Circulatory symptoms: o o lower extremity edema, varicose veins mostly in third trimester due to increased plasma volume and compression of venous return from gravid uterus expansion of plasma volume o begins at fourth week of pregnancy o increases by 15% in first trimester o peaks at 28-34 weeks, then plateaus until delivery o average gain at term 1,100-1,600 mL dizziness and syncope may be positional, may occur when supine more often in warmer climates - lower vascular resistance due to dilation of peripheral vessels to dissipate heat Glycosuria Iron Clinical Intervention and Clinical Therapies onions) limited evidence regarding treatment of heartburn in pregnancy ranitidine is the best-studied medication shown to be effective for heartburn in pregnancy, evidence based on small short-term trials aluminum phosphate has efficacy as an antacid antacids effective, but may bind iron o calcium carbonate (Tums) may provide antacid and source of calcium generally considered safe and first-line therapy excessive carbonate can lead to milk-alkali syndrome (hypercalcemia, renal impairment, metabolic alkalosis) H2 blockers o all 4 drugs are FDA Pregnancy Category B o ranitidine (Zantac) and cimetidine(Tagamet; Nu-Cimet in Canada) preferred over famotidine (Pepcid) and nizatidine (Axid) due to more fetal safety data o cimetidine no recommended by some researchers due to possibility of feminization exposure to proton pump inhibitors in early pregnancy might not be associated with significantly increased risk of adverse outcomes proton pump inhibitors o omeprazole (Prilosec; Losec in Canada) is Pregnancy Category C despite C rating, some recommend omeprazole as proton pump inhibitor of choice due to more fetal safety data embryonic and fetal toxicity reported, but low risk o other proton pump inhibitors are Pregnancy Category B esomeprazole (Nexium) lansoprazole (Prevacid) -recommended by some as proton pump inhibitor of choice pantoprazole (Protonix) rabeprazole (AcipHex) Abdominal pain: o sharp pain often due to spasm of round ligaments often associated with movement Other completely vascular spiders appear in 66% of white patients and 11% of black patients during 25 months of pregnancy 90% regress by 3 months postpartum most common around eyes o striae (stretch marks) over abdomen, breast, hips develop in 65% of pregnant women permanent but may fade over time o hirsutism and acne - due to placental androgens HEENT: o o brownish-red opacities on posterior cornea (Krukenberg spindles) o swollen nasal turbinates o gingivitis, gum hypertrophy, bleeding gums Breast: o breast enlargement due to vascular engorgement, ductal growth (estrogen effect) and alveolar hypertrophy (progesterone effect) o breast veins become more visible o nipples may become more erect and darker o areolae darken o expression of colostrum from nipples may occur in third trimester Cardiac: o o o o heart rate increases slightly systolic ejection murmur (II/VI) heard in 96% of women diastolic murmur in pregnancy is abnormal wide splitting of S1 and Disease Description & H&P Diagnosis and Diagnostic Study due to enlarged uterus compressing inferior vena cava, causing venous pooling and decreased cardiac output Respiratory symptoms: o dyspnea of pregnancy, decreased exercise tolerance o 60%-70% of women will experience in first or second trimester o may cause sleep disturbance o causes progesterone-induced hyperventilation in early pregnancy decreased functional residual capacity due to limited movement of diaphragm secondary to gravid uterus in late pregnancy Gastrointestinal symptoms: o o increased appetite and dietary cravings persists throughout pregnancy driven by increased estrogen nausea and vomiting occurs in 70% of pregnancies usually between 6-16 weeks gestation more common in younger women, primigravidas and overweight women rarely severe enough to compromise nutrition mostly due to high levels of serum estrogen and hCG, but can be due to hyperthyroidism, Osmolality Uric acid Decreas e Dilutional Decreas e During 1st and 2nd trimesters, dilutional Serum Enzymatic Activities o Alkaline phosphatase Increase Drug metabolism Increase o Serum Hormones Cortisol Increase Growth hormone Increase Insulin Increase Parathyroid hormone Progesterone Clinical Intervention and Clinical Therapies Increase Due to decreased total calcium Increase 9-47 ng/mL (1st trimester); 55-255 ng/mL (3rd trimester) more common on right side due to normal dextrorotation of uterus improved physical fitness and abdominal wall muscle tone can help prevent round ligament strain advice for patients o regular exercise o avoid sudden movement o rise and sit gradually o rest and local heat is best treatment, consider lying down on side of pain o analgesia occasionally necessary with acetaminophen abdominal pain in second or third trimester should be evaluated to rule out uterine irritability or premature contractions also consider non-pregnancy-related abdominal problems appendicitis - occurs in 0.13% pregnancies in any trimester, 35% fetal mortality with perforation, may be felt in right upper quadrant instead of right lower quadrant, laparoscopic appendectomy has been safely performed in pregnancy (Surg Endosc 1990;4:100) nephrolithiasis (renal colic) - 1/1,000 pregnancies, may have increased incidence of preterm labor (Am Fam Physician 1989;40:185), usually diagnosed by ultrasound but may be difficult to differentiate obstructive vs. physiologic hydronephrosis cholelithiasis and cholecystitis (biliary colic) - increased risk of cholelithiasis in pregnancy, but no increased incidence in symptomatic biliary disease; 1-6 in 10,000 pregnant patients get cholecystectomy, safest period is second trimester gastroenteritis - oral hydration preferable, monitor hydration status closely hepatic disorders o intrahepatic cholestasis of pregnancy o acute fatty liver of pregnancy - rare but fatal, more common in young primiparas and multiple gestation, usually late in third trimester; onset with anorexia, nausea, vomiting, malaise, headache; later epigastric and RUQ abdominal pain, jaundice, coma with Other splitting of S2 heart sounds in third trimester o point of maximal impulse shifted cephalad to fourth intercostal space and laterally to midclavicular line (due to enlarging uterus) o cardiac output increased by 30%-50% above baseline, higher in left lateral decubitus position o jugular venous distension (JVD) common Lung: o physiological hyperventilation elevation of diaphragm decreased functional residual capacity tidal volume increases 40% at rest, minute ventilation increases by 30% Abdomen: o o o striae gravidarum linea nigra - line of increased pigmentation develops from xiphoid to symphysis pubis uterine enlargement palpable at 12-14 weeks manual measurement of fundal height as accurate as ultrasound from 18-32 weeks gestation insufficient data to assess utility of routine use of symphysisfundal height measurements in routine antenatal care, no evidence of improved pregnancy outcome in single identified trial expected fundal height Disease Description & H&P multiple gestation, or molar pregnancies vomiting in early pregnancy reported in 56% of 9,098 firsttrimester registrants; more common in primigravidas, younger women, women with limited education, nonsmokers and women weighing > 170 lbs: vomiting associated with lower incidence of stillbirth, miscarriage or premature delivery o gastroesophageal reflux occurs in 50% of women in third trimester due to relaxation of lower esophageal sphincter (by progesterone) and expanding uterus o constipation from decreased gastric motility and increased water absorption (progesterone-related) Neurologic symptoms: o headache prevalence in pregnancy migraine during pregnancy diagnosis significantly associated with o stroke o myocardial infarction/heart disease o pulmonary embolus/venous thromboembolism o hypertension o preeclampsia/gestational hypertension o smoking o diabetes Diagnosis and Diagnostic Study Prolactin Increase Testosterone Increase Thyroxine-binding globulin Increase Free T4 Unchang ed Free T3 Unchang ed Total T4 Increase Due to increased thyroxine binding globulin TSH Decreas e In first trimester Hematologic values Bleeding time Unchang ed Blood volume Increase by 50% ESR Increase Fibrinogen Increase Decreas Hemoglobin/hema es by Average Clinical Intervention and Clinical Therapies hepatic encephalopathy, bleeding diathesis, metabolic acidosis, mild hypertension, proteinuria, edema; high maternal mortality if diagnosis and delivery delayed o PIH-associated hepatic changes include nausea, vomiting, epigastric and RUQ abdominal pain; HELLP syndrome includes microangiopathic hemolytic anemia, elevated transaminases and thrombocytopenia o fulminant hepatitis - usually viral, delivery of fetus may be necessary for survival ruptured ovarian cyst adnexal torsion red degeneration (necrobiosis) of uterine fibroid - most common in early second trimester Back pain: o compensatory lumbar lordosis, ligament laxity, poor abdominal muscle tone and poor posture contribute to back pain o prevention includes avoiding excessive weight gain, improving posture, proper bending with straight back, wearing flat or low-heeled shoes o firm bed mattress, local heat, massage may help o acetaminophen if analgesia needed o consider lumbar disk disease if associated leg weakness o exercise may reduce low back pain during pregnancy Constipation o progesterone decreases bowel motility especially in first trimester, expanding uterus displaces and compresses intestine in third trimester o iron replacement may also worsen constipation o increase fluids (at least 2 quarts/day = 8 glasses/day = 64 oz/day) o increase bulk (fresh fruit, vegetables, whole grains, fiber supplementation) o fiber supplementation (as bran or wheat fiber) daily effective in treating constipation in pregnancy based on 1 trial; if ineffective, stimulant laxatives are more effective than bulkforming laxatives but may cause more side effects, based on 1 trial (Reference - Cochrane Database Syst Rev 2001;(2):CD001142 [review Other = 37.1 cm + 0.119 x (gestational age in days - 280) + 0.074 × (initial weight in kg - 66.5) + 1.01 (if parous, 0 if nulliparous) + 0.91 (if female fetus, 0 if male fetus), based on series of 325 women with uncomplicated singleton pregnancies who had ultrasound dating < 20 weeks gestation o Leopold maneuvers for fetal size and position o fetal heart tones for viability Back: o lumbar lordosis to maintain center of gravity Neuro: o unsteady gait in third trimester due to relaxation of pelvic joints, lumbar lordosis, and gravid uterus Extremities: o lower extremity edema usually bilateral, consider deep vein thrombosis (DVT) if unilateral due to compression of inferior vena cava by gravid uterus Pelvic: o o o o o congestion and bluish hue of vagina (Chadwick's sign) in early first trimester due to increased blood flow softening of cervix (Hegar's sign) mucous plug softening and enlargement of uterus after 6 weeks uterine size larger than dates with full bladder, trophoblastic disease, uterine fibroids, multiple Disease Description & H&P Diagnosis and Diagnostic Study migraine diagnosis not associated with several non-vascular diagnoses (pneumonia, transfusions, postpartum infection or hemorrhage) Genitourinary symptoms: tocrit 10-15% Plasminogen Increase o Platelets Decreas e urinary frequency, nocturia, stress incontinence due to enlarging uterus and increased progesterone urinary stasis may lead to increased urinary tract infections in pregnancy, age > 35 years, high body mass index (BMI), and family history of incontinence associated with risk for urinary incontinence Musculoskeletal symptoms: Normal > 100,000 Red cell volume s Increased erythropoie tin 2-4 fold due to increased human placental lactogen and red cell mass WBC Average 12,000 cells/mm 3 Increase o o low back pain carpal tunnel syndrome most common in second and third trimesters results from edema of hands and wrists should resolve after delivery o leg cramps usually during second half of pregnancy mainly gastrocnemius muscle tend to occur during sleep, often cause awakening may be due to calcium or magnesium deficiency hip pain - hormone relaxin contributes to laxity of sacroiliac joint and symphysis pubis, beginning at 10-12 weeks of pregnancy o unsteady gain after 20 weeks gestation due to 12.5 g/dL Increase Abbreviations: BUN, blood urea nitrogen; ESR, erythrocyte sedimentation rate; GFR, glomerular filtration rate; THS, thyroid-stimulating hormone; WBC, white blood cell count. Serum Chemistries: o tumor markers including serum carbohydrate antigen 15-3, squamous cell carcinoma antigen, and CA-125 may be elevated during normal pregnancy Clinical Intervention and Clinical Therapies updated 2010 Jan 18]) exercise mild laxatives (milk of magnesia), stool softeners, bulk producers (cellulose powders) are also safe and effective o cathartic laxatives and enemas rarely needed o review of constipation treatments in pregnancy increase fluid intake increase fiber in diet bulking agents (for example, psyllium) considered first-line therapy osmotic/saline laxatives o lactulose and magnesium citrate are Pregnancy Category B o PEG, sodium phosphate (Visicol) and magnesium hydroxide (Milk of Magnesia) do not have pregnancy category designation o PEG considered first choice if bulking agents ineffective o long-term use of magnesium citrate or sodium phosphate may lead to hypermagnesemia, hyperphosphatemia and dehydration stimulant laxatives o bisacodyl (Correctol) and senna(Senokot) o Pregnancy Category C o low risk in short-term use o long-term use not recommended stool softener o docusate (DSS) o Pregnancy Category C o no toxicity reports o contained in some prenatal vitamins lubricants - avoid use in pregnancy o castor oil is Pregnancy Category X o mineral oil is Pregnancy Category C lubiprostone (Amitiza) is Pregnancy Category Diarrhea o fluid replacement o attapulgite (Kaopectate in Canada) is Pregnancy Category C attapulgite considered antidiarrheal of choice in pregnancy formulation of Kaopectate contains bismuth subsalicylate and NOT recommended o loperamide (Imodium) in Pregnancy Category B o o Other gestations, macrosomia, polyhydramnios o uterine size less than dates with intrauterine growth retardation (IUGR), oligohydramnios, malpresentation Rectal: o hemorrhoids due to increase in portal system venous pressure Disease Description & H&P o o o lordosis of pregnancy and changes in center of gravity pelvic pain uterine sensations quickening (sensation of fetal movement) occurs at 16-20 weeks gestation o 16-18 weeks in multigravidas o 19-20 weeks in primigravidas Braxton-Hicks contractions o common in third trimester o irregular contractions less frequent than every 8 minutes other symptoms - pruritus, paresthesias (from nerve compression), snoring, swelling of vulva/vagina, palpitations Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies limited human data, animal data suggests low risk avoid during first trimester, possible increase in fetal cardiac malformation o antidiarrheals NOT recommended alosetron (Lotronex) is Pregnancy Category B, bismuth subsalicylate (Pepto Bismol, Kaopectate) is Pregnancy Category C; salicylate absorption can increase perinatal mortality, premature closure of ductus arteriosus, neonatal hemorrhage, decreased birth weight, prolonged gestation or labor, and possible teratogenicity diphenoxylate/atropine (Lomotil) is Pregnancy Category C, teratogenic in animals Nasal congestion: o may be related to increased circulation and edema mediated by estrogen o increasing humidity with vaporizer may be helpful o saline nose drops or sprays are safe and effective Nasal and Ocean are some common brand names can be made at home by adding 1/2 teaspoon table salt to 1 cup warm water, make fresh daily, use dropper for application FDA Pregnancy Category A o decongestants avoid oral decongestants, which have been associated with small increase in minor birth defects oral decongestants should be avoided during first trimester of pregnancy due to association with gastroschisis use pseudoephedrine if oral drug necessary, best safety record during pregnancy of oral decongestants topical nasal decongestants o can cause rhinitis medicamentosa if used > 3 days Allergic symptoms: o topical nasal steroids effective in allergic rhinitis, but must be used continuously and have 3-7 day Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies lag period; FDA Pregnancy Category C (antihistamines chlorpheniramine (Chlor-Trimeton; ChlorTripolon in Canada) considered first-line if oral antihistamine needed, FDA Pregnancy Category B doxylamine is Pregnancy Category A, but cough/cold products with doxylamine usually contain other products other antihistamines that are Pregnancy Category B o clemastine (Tavist) o diphenhydramine (Benadryl) o cetirizine (Zyrtec; Reactine in Canada), but not recommended during first trimester o loratadine (Claritin), but not recommended during first trimester antihistamines that are Pregnancy Category C o brompheniramine (Dimetapp) o desloratadine (Clarinex) o fexofenadine (Allegra) o promethazine (Phenergan; o triprolidine (Actifed) ough medications that are Pregnancy Category C benzonatate (Tessalon Pearls) codeine (Pregnancy Category D for prolonged use or high doses at term) - avoid use in first trimester dextromethorphan (Robitussin DM) guaifenesin (Robitussin, Fenesin, Humibid, Mucinex) - avoid use in first trimester hydrocodone (Pregnancy Category D for prolonged use or high doses at term) - avoid use in first trimester Hemorrhoids: o o o o o o treat constipation prevention by avoiding constipation and prolonged sitting Kegel exercises improve rectal muscle tone often regress after delivery if symptomatic, especially after delivery from prolonged pushing sitz baths (immersing hips and buttocks) with warm water for 20 minutes then application of witch hazel (Tucks pads) preparation H, Anusol, Tucks, ProctoFoam safe Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o Contracepti on Other and effective thrombosed (hard and tender) external hemorrhoids may require incision and evacuation under local anesthesia progestogen-only contraceptives Pearl index about 0.3% with perfect use and about 9% with typical use (includes inconsistent or incorrect use) usual dosing regimen with progestogen-only pills is 1 active pill orally once daily (no or placebo or pill-free interval) progestogen-only pills are considered best option for women who prefer oral contraceptive but have contraindications to combined oral contraceptives including nonbreastfeeding women immediately postpartum (not associated with increased risk of thrombosis) IUDs most women are good candidates for hormonal and nonhormonal IUDs, including, both parous women and nulliparous women, adolescents, and women with history of ectopic pregnancy significant complications are rare. both hormonal and nonhormonal IUDs may be inserted any time during cycle when pregnancy can be excluded options include copper IUD, levonorgestrelreleasing intrauterine system barrier methods barrier methods include male condom or female condom, diaphragm, cervical cap, andsponge these methods are often used with spermicide barrier methods are less effective than hormonal methods or IUDs tubal sterilization indicated for well-informed women who have completed childbearing considered ideal candidates for sterilization, but age and parity should not limit use there are no absolute contraindications to tubal sterilization interval procedure may be performed anytime, but ideally between days 6-13 of menstrual cycle postpartum and postabortion procedures may also be performed o o o o o emergency contraception is defined as contraceptive methods used after unprotected intercourse or potential contraceptive failure and before implantation emergency contraception may be indicated for any reproductive-aged woman who does not want to be pregnant following unprotected or inadequately protected sexual intercourse no clinical exam or testing is required prior to administering emergency contraception although consider pregnancy testing and testing for sexually transmitted infections initiate emergency contraception as soon as possible after unprotected intercourse as efficacy declines with increasing delay between intercourse and treatment (not effective once implantation has occurred) emergency contraception options copper intrauterine device (IUD) o considered most effective method of emergency contraception with about 0.09% pregnancy rate if inserted within 5 days of intercourse o well-tolerated in most women o efficacy not Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o efficacy varies by sterilization technique and patient age (women aged < 30 years at sterilization may have increased risk for method failure compared to older women) o Essure (hysteroscopic procedure) reported to be most effective sterilization method overall fertility awareness-based methods fertility awareness-based methods are an alternative to hormonal methods and devices, but effectiveness depends on appropriate guidelines being followed consistently. methods include o calendar or rhythm method (estimates timing of ovulation by documenting longest and shortest cycle durations over 6-12 month period) o temperature or basal body temperature (BBT) method (estimates times of ovulation by measuring BBT daily until elevated readings for ≥ 3 days indicate ovulation has occurred) o ovulation or Billings ovulation method (estimates timing of ovulation by assessing cervical mucus secretions throughout cycle) o symptothermal methods (combination of preceding 3 methods) o at-home use of technological instruments (such as ovulation prediction kits) to identify fertile phase via samples of urine, saliva, or cervical mucus (may be combined with other methods) emergency contraception emergency contraception is used to avoid pregnancy after unprotected intercourse or potential contraceptive failure and before implantation emergency contraception should be initiated as soon as possible after unprotected intercourse as efficacy declines with increasing delay between intercourse and treatment options include copper IUD, levonorgestrel (Plan B), ulipristal acetate (UPA), and combined oral contraceptives Combined oral contraceptives (COCs): Other o affected by body weight (may be used in obese women) o requires insertion by trained medical professional o associated with same contraindications as routine IUD use o if IUD fails to prevent pregnancy, immediately remove device and rule-out ectopic pregnancy (may have increased risk if pregnancy occurs during use) levonorgestrel (Plan B) progestogen-only oral contraceptive available in single-dose (1.5 mg) or double-dose regimens (2 pills containing levonorgestrel 0.75 mg each taken 12 hours apart) considered most effective when administered within 72 hours (3 days) of intercourse and associated with about 1.1%-2.4% failure rate levonorgestrel may be used ≥ 1 time/cycle, even if earlier episode of unprotected intercourse occurred outside 120 hour treatment window (will not disrupt implanted pregnancy) levonorgestrel may be used in women with contraindications to daily hormonal Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o o o o COCs contraindicated women with certain medical conditions including but not limited to breast cancer venous thromboembolism migraine with aura dosing regimens usual dosing regimen is 1 active pill orally once daily for 21 consecutive days followed by 7-day pill-free adverse effects estrogenic effects (such as altered bleeding patterns, mood changes, breast enlargement/tenderness, and nausea) androgenic effects (such as acne, hirsutism, and lipid changes) COCs reported to double the risk for venous thromboembolism compared to nonusers, but overall risk is still low current use of oral contraceptives may be associated with increased risk for ischemic stroke but not hemorrhagic stroke or myocardial infarction noncontraceptive benefits may include improvement in acne premenstrual symptoms and dysmenorrhea menorrhagia polycystic ovary syndrome oral contraceptives and cancer combined oral contraceptives may be associated with decreased mortality from cancer and various other causes COCs may reduce risk for some cancers, like endometrial and ovarian cancer Progestogen-only injectable contraceptives: o depot medroxyprogesterone acetate (DMPA) (Depo-Provera) formulations include o depot medroxyprogesteroneacetate (Depo-Provera) 150 mg/1 mL administered by healthcare provider via intramuscular injection every 3 months o Depo-subQ Provera 104 mg/1 mL administered by patient or healthcare provider via subcutaneous injection every 3 months Other o o contraceptives ulipristal acetate (CDB2914) progesterone receptor modulator developed for use as emergency oral contraceptive in single 30 mg dose considered most effective when taken up to 120 hours (5 days) after unprotected intercourse with about 2% pregnancy rate and no apparent decline in efficacy during that time repeat dosing with ulipristal acetate (UPA) not recommended combination oral contraceptives (Yuzpe regimen) may be formulated from variety of standard oral contraceptives o standard dose is 2 tablets of Ovral in 2 dose regimen (2 tablets/dose) with first dose within 72 hours of unprotected intercourse and second dose 12 hours later o other brands may be substituted for Ovral with similar efficacy o associated with about 3.2% failure rate o Yuzpe regimen associated with significantly more nausea and vomiting than levonorgestrel-only regimen o anti-emetic taken 1 Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other DMPA may be used by women of all ages, testing not typically indicated in healthy women prior to starting DMPA administration o first DMPA injection may be given any time in menstrual cycle if reasonably certain woman is not pregnant if administered within 5-7 days of start of menstrual cycle, backup contraception not required if administered > 5-7 days since start of menstrual cycle, advise patient to abstain from intercourse or use back-up contraception for 7 days o repeat DMPA injections every 3 months (1213 weeks) o hormone-related adverse effects o bleeding irregularities most common adverse effect associated with DMPA use (in about 20%40% patients) o DMPA may be associated with 2-3 kg (4.4-6.6 lbs) weight gain over 1 year, complications o DMPA associated with decreased bone mineral density (level 3 [lacking direct] evidence) o loss of bone mineral density with use of depot medroxyprogesterone may reverse after method discontinuation (level 3 [lacking direct] evidence) o recent DMPA use (within last 5 years) for ≥ 12 months may be associated with increased risk for breast cancer o implantable contraceptives are a type of longacting reversible contraceptive (LARC) method (along with intrauterine devices)(1) primary mechanism of action is prevention of ovulation by suppression of hypothalamic-pituitary-ovarian axis progestin-only implants may also reduce pelvic pain associated with dysmenorrhea, endometriosis, and pelvic congestion syndrome o etonogestrel-releasing implant Implanon is a progestin-only subdermal contraceptive implant for use up to 3 years Nexplanon is a radiopaque, bioequivalent modification of Implanon with redesigned o hour before Yuzpe emergency contraception may help reduce incidence and severity of nausea and vomiting mifepristone (RU486) (Mifegyne) availability limited to China and Vietnam (not licensed for use in United States, Canada, or United Kingdom) associated with about 1.5% failure rate (varies by dose and time of treatment during menstrual cycle) progesterone receptor modulator (antiprogestin) containing mifepristone additional considerations risk of pregnancy reported to be 3 times greater in women with body mass index (BMI) ≥ 30 kg/m2 compared to women with BMI < 25 kg/m2 with any hormonal emergency contraception concomitant use (and up to 28-days after last use) of liver enzymeinducing drugs may decrease efficacy of hormonal emergency contraception by reducing concentrations of levonorgestrel (LNG), ulipristal acetate, and combination oral contraceptives Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies inserter healthcare providers in the United States should complete FDA-mandated training from manufacturer prior to insertion or removal of implants o transdermal patch or vaginal ring are methods of delivering continuous combined hormonal contraception o contraceptive patch (Ortho Evra/Evra) transdermal combined hormonal contraceptive containing estrogenic ethinyl estradiol (EE) and progestogenic norelgestromin contraceptive patch may increase risk of venous thrombosis in women without previous thrombotic disease NuvaRing contains estrogenic ethinyl estradiol 2.7 mg and progestogenic etonogestre Barrier methods: Condom: o male condom male barrier contraceptive characterized by thin sheath designed to cover entire length of penile shaft during intercourse Female condom female barrier contraceptive characterized by soft, loose-fitting sheath or pouch (polyurethane, nitrile, or latex) about 17 cm long with flexible ring on each end accounts for about 0.2% of all condom use worldwide Cervical cap: o o o cervical cap is a small, metal, rubber, or plastic cap designed to prevent sperm from entering cervix reported first-year pregnancy rates 4.8%-19.3% (may be more common in nulliparous women) use contraindicated in women with notably distorted cervical anatomy cervical intraepithelial neoplasia (CIN) cervical cancer history of toxic shock syndrome (USMEC Category 3; UKMEC Category 3) high risk of HIV infection (USMEC Category 4; UKMEC Category 4 due to concomitant use of spermicide) HIV infection with or without use of antiretroviral therapy (USMEC Category Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o o o 3;UKMEC Category 3 due to concomitant use of spermicide) AIDS (USMEC Category 3; UKMEC Category 3 due to concomitant use of spermicide) see Barrier contraceptive methods for details Other barrier methods: sponge disposable female barrier contraceptive designed to absorb ejaculate, carry spermicide, and block ostium of uterus (external cervical os) not recommended for use in women with history of toxic shock syndrome (USMEC Category 3; UKMEC Category 3) types include o Today sponge o Pharmatex sponge (vaginal tampon) o Protectaid sponge spermicide chemical barrier contraceptive characterized by mechanical interference with sperm movement and biochemical immobilization and destruction of sperm due to relatively low efficacy, spermicide alone not recommended for contraception in some regions, including Western Europe o reported pregnancy rate in first year of use 6%-18% with perfect use 26%-28% with typical use (includes method- and user-failure) o insufficient evidence to establish efficacy of spermicides for pregnancy prevention FDA requires manufacturer warning stating nonoxynol-9 does not prevent HIV or other sexually transmitted disease transmission and may increase risk of contracting HIV/AIDS nonoxynol-9 may increase susceptibility to human papillomavirus infection, especially in women with HIV indications and contraindications well-informed women who have completed childbearing considered ideal candidates for sterilization, but age and parity should not limit use Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other o o o Cervical Cancer o o invasive carcinoma originating in transformation zone of cervix, most commonly in squamous cells second most common cancer in women there are no absolute contraindications to tubal sterilization timing interval procedure may be performed anytime, but ideally between days 6 and13 of menstrual cycle postpartum procedure may be performed o at time of cesarean delivery o within 2 days postpartum (if not performed within 2 days postpartum, wait ≥ 6 weeks postpartum to perform interval procedure) postabortion procedure may be performed immediately or within 1 week after abortion if no suspicion of pelvic infection efficacy efficacy varies by sterilization technique and patient age (women aged < 30 years at sterilization may have increased risk for method failure compared to older women) Essure (hysteroscopic procedure) reported to be most effective sterilization method overall (10-year cumulative pregnancy rate 0.01%-0.02%) 10-year cumulative failure rate about 1.9% for abdominal tubal sterilization procedures tubal sterilization may be performed via transcervical route (hysteroscopy) with mechanical implants including o Essure o Adiana o Ovabloc abdominal route o with laparoscopic techniques, including electrocoagulation mechanical devices tubal excision (complete or partial salpingectomy) o with minilaparotomy, including Pomeroy technique (most common) Making the diagnosis: Treatment overview: o o most women diagnosed as part of evaluation of abnormal Pap smear, with or without symptoms (such as vaginal bleeding or other discharge), using colposcopically directed cervical biopsy o treatment plan is based on clinical staging (FIGO staging and radiologic staging) and risk assessment including nodal status and histological biopsy results treatment for early invasive cancer (small tumors histologic types squamous cell carcinoma is most frequent type accounting for two-thirds of cervical cancers(1, 2, 3, 4) adenocarcinoma accounts for about 10%-20% cervical Disease Description & H&P worldwide, third most common cause of female cancer mortality Chief concern (CC): o o o o o early stage disease usually asymptomatic and detected by cervical smear symptoms at presentation reported in about 16%-32% of women vaginal bleeding or bloodstained vaginal discharge may be postcoital, intermenstrual, postmenopausal, or spontaneous lymphedema in lower extremities (from lymphatic compression of locally invaded pelvic lymph nodes) pelvic pain if lymph nodes involved may have backach Diagnosis and Diagnostic Study o other methods of diagnosis include cervical biopsy of grossly visible or palpable lesion cone biopsy (via laser or cold knife cone) if microinvasion or early stage cervical carcinoma suspected Differential diagnosis: o o Chlamydia trachomatis or other sexually transmitted infection in women presenting with complaint of vaginal bleeding, serosanguineous vaginal discharge, pelvic pain inflamed or friable cervix endometrial adenocarcinoma MRI preferred to CT scan and should include pelvic and abdominal imaging o better than CT for tumor extension assessment o equal to CT for nodal involvement assessment Clinical Intervention and Clinical Therapies ≤ 4 cm confined to cervix) based on European Society for Medical Oncology (ESMO) and Scottish Intercollegiate Guidelines Network (SIGN) guidelines initial treatment is surgery or radiation o surgery and radiation therapyappear to have similar efficacy for early stage (IB or IIA) cervical cancer o for patients who have surgery,chemoradiation used if any of following risk factors positive margins parametrial involvement pelvic node involvement o consider adjuvant radiation therapyfor patients who have negative nodes, and any 2 of the following greater than a third stromal invasion lymphovascular space invasion tumor diameter > 4 cm o adjuvant radiation therapy after radical hysterectomy may decrease risk of disease recurrence compared with no further treatment FIGO stage IA1 o treat with either of conization with free margins simple hysterectomydepending on patient age, desire for childbearing, and hormonal status o pelvic lymphadenectomy pelvic lymphadenectomy recommended by ESMO if lymphovascular space involved SIGN recommends not removing pelvic lymph nodes during treatment for International Federation of Gynecology and Obstetrics (FIGO) IA1 disease FIGO stage IA2 o treat with surgery o pelvic lymph nodes should be removed o surgical options include simple or radical hysterectomy or conization ortra chelectomy (fertility-sparing alternative to hysterectomy) in young patients FIGO stage IB1 - no standard treatment, options include Other cancers(1) o small cell carcinoma rare compared to squamous cell carcinoma or cervical adenocarcinoma Who is most affected: o women aged 30-45 years Causes: o persistent infection with oncogenic types of human papillomavirus (HPV)(1, 3) o most prevalent oncogenic types are HPV-16, HPV-18 Pathogenesis: o progression of epithelial change associated with human papillomavirus (HPV) infection(6, 7) viral particles enter basal layer through small tears in mucosa, infect metaplastic epithelium in ring of mucosa known as cervical transformation zone molecular virology of HPV persistence, progression, and invasion poorly understood o not known how often precancer develops from mild lesion vs. an equivocal lesion or cytologically normal HPVinfected tissue o persistent HPV infection of epithelium in cervical transformation zone causes most cases of cervical cancer Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o surgery options includehysterectomy and radical trachelectomy SIGN recommends radical surgery for stage IB1 disease if there are no contraindications , not recommended if tumor > 4 cm o external irradiation plus brachytherapy (short-waved radiation therapy delivered by applicators inserted in uterus via vagina) o combined radiation therapy and surgery - preoperative brachytherapy followed by surgery 6-8 weeks later treatment for locally advanced cancers (FIGO stage IB2 tumors and higher) based on ESMO and SIGN guidelines stage IB2-IVA o chemoradiation associated with increased survival compared to radiation therapy alone in women with locally advanced cervical cancer, but may increase acute toxicity o chemotherapy as adjuvant to radiation therapy may reduce risk of death and disease progression o chemotherapy SIGN recommends any patient considered suitable for radiation therapy should have concurrent chemotherapy with a platinumbased chemotherapy if well enough to tolerate have their hemoglobin level monitored and corrected if it falls below 12 g/dL insufficient evidence of usefulness of adjuvant chemotherapy after chemoradiation o external irradiation plus brachytherapy o SIGN recommends monitoring hemoglobin in patients receiving radiation or chemoradiation and correct if hemoglobin level falls below 12 g/dL (120g/L o adjuvant extrafascial hysterectomy after radiation therapy may be considered for patients with persistent disease Other progression from small cervical intraepithelial neoplasia (CIN) lesion to cancer can take > 10 years o regression of CIN may occur o cancer spreads locally to parametria, vagina, and pelvic sidewall o nodal spread common, usually occurs in stepwise manner to pelvic lymph nodes, then to para-aortic nodes smoking associated with increased risk of squamous cell carcinoma of the cervix but not adenocarcinoma diethylstilbe strol (DES) exposure in utero may increase risk for cervical cancer Disease complications: o o o lymphedema (may also be treatment related) in 1 or both lower limbs(5) complications due to advanced disease progression(5) renal failure, ureteric obstruction (from lymphadenopathy or tumor invasion) thrombosis and hemorrhage rectovaginal or vesicovaginal fistulas (rare) sexual dysfunction many women with cervical cancer experience sexual problems (disease or treatment related) due to vaginal changes and/or hormonal changes including(5) o loss of libido Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies stage IVB - platinum-based combination chemotherapy may be beneficial, such as o cisplatin with paclitaxel o cisplatin with topotecan o treatment for locoregional and metastatic recurrence palliative chemotherapy standard treatment for most patients SIGN recommends cisplatin with either topotecan or paclitaxel for palliative chemotherapy for stage IVB or recurrent cervical cancer pelvic exenteration an option for central pelvic recurrence without extrapelvic metastases consider salvage radiation therapy in patients with pelvic recurrence who were not previously irradiated o SIGN recommendations for pregnant women with cervical cancer choice of therapeutic modality should be decided for nonpregnant patients immediate treatment recommended for women diagnosed before 16 weeks gestation for women with early stage disease (FIGO IA1, IA2, IB) diagnosed after 16 weeks of gestation, treatment may be delayed to allow fetal maturity to occur for women with advanced disease (FIGO 1B2 or greater) diagnosed after 16 weeks gestation, decision to delay must be based on gestational age at time of diagnosis Medications: o Chemoradiation: chemoradiation associated with increased survival compared to radiation therapy alone in women with locally advanced cervical cancer Surgery and procedures: Indications: o surgery for early stage disease conserves ovarian function results in less vaginal shortening and fibrosis compared to radiation therapy, Other o change in sexual activity o decreased orgasm women who have been treated for cervical cancer more likely than controls without cancer to have persistent vaginal changes that compromise sexual activity (N Engl J Med 1999 May 6;340(18):1383 full-text) review of sexual morbidity after radical hysterectomy for cervical cancer can be found in Expert Rev Anticancer Ther 2010 Jul;10(7):1037 Complications of radiation therapy: o o o acute radiation toxicity may include(2) fatigue diarrhea irritative bladder symptoms acute toxicity is increased when concomitant chemotherapy is given, especially(1, 2, 5) hematologic effects (anemia, leukopenia, thrombocytopenia) gastrointestinal effects late radiation side effects (occur ≥ 3 months after completion of radiation therapy)(2, 5) small bowel obstruction fistula rectal bleeding rectosigmoid stenosis ureteric stricture bladder o urinary frequency, urgency Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies beneficial for residual sexual function allows accurate assessment of lymph node status Prevention of human papillomavirus (HPV) infection: HPV vaccination: o quadrivalent human papillomavirus (HPV) recombinant vaccine against HPV types (6, 11, 16, and 18) (Gardasil) Gardasil 0.5 mL intramuscular injections into deltoid or anterolateral thigh given at 0, 2, and 6 months; costs about $155 per dose or $465 for full course quadrivalent HPV vaccine induces immunogenicity in children aged 9-15 years quadrivalent HPV vaccine is effective in preventing cervical and external genital disease in women aged 24-45 years but may not be cost-effective quadrivalent HPV vaccine associated with decreased genital lesions related to HPV-6/11 in men aged 16-26 years bivalent HPV recombinant vaccine against HPV16/18 vaccine (Cervarix) Other o o o o dysuria detrusor instability hematuria ulceration Screening do not start cervical cancer screening before age 21 years Do not perform cervical cancer screening at age 21-65 years stop screening after age 65 years if consecutive normal testing for prior 10 years for women aged 21-29 years o cervical cytology (Pap smear or liquid-based) recommended every 3 years ) o human papillomavirus (HPV) DNA testing not recommended for women aged 30-65 years o combination of cytology screening plus HPV testing every 5 years recommended, but cytology screening alone every 3 years is an alternative o HPV testing alone not recommended cervical cancer screening appears to reduce incidence of invasive cervical cancer cervical cancer screening appears to reduce incidence of cervical cancer in women > 30 years old, but efficacy of Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Other screening uncertain in women < 30 years optimal screening interval for cervical cancer screening is uncertain management of abnormal screening results varies by abnormality, age, and prior history colposcopy generally recommended for highgrade cytologic abnormalities, or lowgrade cytologic abnormalities which persist or are associated with positive HPV test repeat testing at shorter intervals (such as 12 months) generally recommended for lowgrade cytologic abnormalities or following negative colposcopy o Spontaneo us Abortion – First Trimester Abortion Description: o o spontaneous pregnancy loss occurring before 13 weeks gestation, with most losses occurring before 12 weeks gestation miscarriage - refers to spontaneous abortion before 20 weeks gestation, types include threatened spontaneous abortion bleeding before 20 weeks gestation with closed cervix, woman may or may not miscarry complete spontaneous abortion - all products o clinical presentation by type of spontaneous abortion threatened abortion o vaginal spotting or light bleeding o closed cervix o no size-date discrepancy on bimanual exam complete abortion o on exam history of heavy vaginal bleeding that has since abated closed cervix small, contracted uterus o on ultrasound empty uterus thickened endometrial lining missed abortion o on exam absence of vaginal bleeding Treatment expectant management o expectant management is effective method in selected cases of confirmed first trimester pregnancy loss o women with an intact gestational sac should be informed that resolution may take several weeks and efficacy may be lower o in absence of hemorrhage or infection, it is safe to wait indefinitely for miscarriage to complete without further intervention o patients can switch at any time to medical or surgical uterine evacuation medical uterine evacuation o most effective for incomplete miscarriage o may be preferred over expectant management for anembryonic gestation Who is most affected: o women with pregnancy < 12 weeks gestation o women > 35 years old Causes: o chromosomal abnormalities maternal infections(1) Listeria syphilis toxoplasmosis bacterial vaginosis, usually caused byMycoplasma or Ureaplas ma o bacterial vaginosis in early pregnancy may increase risk of miscarriage Disease Description & H&P o o o o o of conception have passed incomplete spontaneous abortion some but not all products of conception have passed inevitable spontaneous abortion - cervix has dilated but passage of products has not occurred, miscarriage is unavoidable, usually with vaginal bleeding septic spontaneous abortion - incomplete miscarriage associated with ascending infection of the endometrium, parametrium, adnexa uteri, or peritoneum recurrent miscarriage/spontaneous abortion - defined as ≥ 2 consecutive or 3 total clinical pregnancy losses anembryonic gestation (empty sac or blighted ovum) - gestational sac without embryonic structures embryonic or fetal demise (missed abortion) nonviable pregnancy (absence of embryo within intact gestational sac or absence of fetal heart activity in visible embryo) that has been retained in the uterus stillbirth - fetal death after 20-24 weeks gestation pregnancy of unknown location - positive urine or serum pregnancy test and transvaginal ultrasound findings of no intrauterine fluid collection with normal or near normal adnexa Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies closed cervix on ultrasound embryonic pole ≥ 5 mm without fetal cardiac activity embryonic pole < 5 mm and no interval growth in 1 week incomplete abortion o on exam heavy vaginal bleeding open cervix visible products of conception in cervical opening o on ultrasound, heterogeneous and/or echogenic material along endometrial stripe or in cervical canal septic abortion o pelvic exam and ultrasound findings similar to incomplete abortion o clinical signs of sepsis inevitable abortion may present with o on exam moderate vaginal bleeding open cervix no visible products of conception in cervical opening o on ultrasound visible products of conception in uterus fetal cardiac activity may be present or absent anembryonic gestation may present on ultrasound with(1) gestational sac > 13 mm without yolk sac or > 18 mm without embryonic pole empty gestational sac > 38 days of gestation and no interval growth > 1 week absent fetal heart tones on Doppler fetal monitor o Making the diagnosis: o diagnosis made with combination of clinical and ultrasound findings speculum exam with products of conception visible in cervical opening or vaginal vault can be diagnostic or missed abortion/miscarriage performed with misoprostol, which can be administered on outpatient basis as single or divided dose vaginally or orally with or without priming with mifepristone nonsteroidal anti-inflammatory drug (NSAID) before misoprostol may reduce side effects of fever, chills, and severe cramping (narcotic/acetaminophen may also be prescribed) vaginal misoprostol reported dose range 400-800 mcg vaginal misoprostol effective for completing miscarriage within 24 hours and avoiding need for uterine curettage with anembryonic gestation or missed abortion/miscarriage before 24 weeks misoprostol 400 mcg vaginally increases resolution rate of early miscarriages but increases pain oral misoprostol oral misoprostol appears no more effective than expectant management for priming with mifepristone, give 600 mg orally followed by misoprostol 400 mcg orally 48 hours later surgical uterine evacuation o surgical evacuation reduces rate of unplanned hospital admission but no differences in infection rates compared to expectant management in women with fetal demise or incomplete abortion/miscarriage before 13 weeks gestation o surgical uterine evacuation should be offered to women who prefer to complete their miscarriage in a shorter amount of time than that of expectant management or medical management o insufficient evidence to recommend routine antibiotic prophylaxis prior to surgical uterine evacuation, so o o Other reproductive tract abnormalities shortened cervix congenital uterine abnormalities o congenital uterine anomalies, particularly subseptate or septate, unicornuate, and bicornuate uteri, may be more common in women experiencing miscarriage than in unselected population Complications: o o hemorrhage or heavy bleeding defined as soaking through 2 sanitary pads per hour for two hours in a row if women experience heavy bleeding, screen for anemia and treat as indicated heavy bleeding may lead to symptoms ofhypovolemic shock, including o tachycardia and/or arrhythmia o tachypnea or dyspnea o fever or low body temperature o hypotension and/or syncope reproductive tract infection may be due to retained products of conception women with bacterial vaginosis at time of surgical uterine evacuation may be at increased risk for subsequent pelvic inflammatory disease (PID) bacterial sacroiliitis and Disease Description & H&P Diagnosis and Diagnostic Study Chief concern (CC): o o o most patients present with vaginal bleeding or recent vaginal bleeding that has subsided patients may also present with pelvic pain similar to period pain or cramps recent pelvic pain that has subsided size-dates discrepancy on bimanual exam loss of pregnancy symptoms typical presentation by type of miscarriage threatened spontaneous abortion may or may not have cramping inevitable spontaneous abortion - heavy bleeding with possible visualization of products of conception completed spontaneous abortion history of pain and bleeding and passage of products of conception, but subsided at presentation missed spontaneous abortion - may have spotting or brownish discharge and symptoms of early pregnancy o o o o in absence of visible tissue, consider ultrasound, beta-human chorionic gonadotropin (beta-hCG), progesterone or combination of tests to differentiate miscarriage from viable intrauterine pregnancy or ectopic pregnancy transvaginal ultrasound, serial serum hCG levels, and progesterone may all be required to establish definite diagnosis if serum hCG levels positive for pregnancy, but transvaginal ultrasound fails to confirm, diagnosis of pregnancy of unknown location warranted and should be made(6) if single hCG measurement < 3,000 milliunits/mL and patient stable o treatment for suspected ectopic pregnancy not indicated as may interrupt viable intrauterine pregnancy o confirm diagnosis of ectopic pregnancy vs. viable or nonviable intrauterine pregnancy with followup testing if single hCG measurement ≥ 3,000 milliunits/mL likely diagnosis is nonviable intrauterine pregnancy follow-up hCG and ultrasound indicated to confirm diagnosis prior to initiating treatment Clinical Intervention and Clinical Therapies antibiotic prophylaxis should be given based on individual clinical indications o screening for infection, including Chlamydia trachomatis, should be considered prior to surgical uterine evacuation o consideration should be given to offering local anesthesia or sedation for women who prefer it o vacuum aspiration preferable to sharp curettage o Rho(D) immune globulin (anti-D immune globulin, RhoGAM) often recommended for any bleeding before 20 weeks gestation if Rh-negative mother typical dosing in United States is 50 mcg (250 units) in women with bleeding before 12 completed gestational weeks and 300 mcg (1,500 units) after 12 weeks Royal College of Obstetricians and Gynaecologists (RCOG) recommendations for Rho(D) immune globulin in Rh(D) negative, nonsensitized women with miscarriage o indicated for spontaneous abortion/miscarriage at ≥ 12 weeks gestation o indicated for surgical evacuation of the uterus regardless of gestation o consider giving Rho(D) immune globulin for medical evacuation of the uterus regardless of gestation o not required for spontaneous abortion/miscarriage at < 12 weeks gestation as long as there is no instrumentation of the uterus o regardless of management method, followup indicated to assure completion of miscarriage o acknowledge psychological sequela with pregnancy loss and provide support, follow-up, and access to formal counseling when needed Medications: Misoprostol: History of present illness (HPI): o patient may present with history of o misoprostol can be administered on outpatient basis as single or divided dose orally, sublingually, or vaginally bleeding and cramping usually begin 2-6 hours after administration and most severe symptoms peak within 3-5 hours Other o gluteal abscess after dilation and curettage for incomplete miscarriage in case report psychological sequelae feelings of loss and grief common miscarriage associated with increased risk of depression especially in women without previous children Disease Description & H&P o o o spotting or bleeding pelvic pain or cramping ask about severity of bleeding and attempt to quantify by number of pads or tampons passage of products of conception pelvic pain - if present, quality, location, duration o slight pain is suggestive of threatened miscarriage o moderate pain is suggestive of inevitable, incomplete, or septic miscarriage o severe pain that has since abated is suggestive of complete miscarriage gestational age o date of last menstrual period o estimated length of gestation o previous ultrasound results General physical: patients with incomplete or septic spontaneous abortion may present with symptoms ofhypovolemic shock, including(5) tachycardia and/or arrhythmia tachypnea or dyspnea fever or low body temperature hypotension and/or syncope check for orthostatic vital signs Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies o o o o o o o o o bleeding may continue for up to 3 weeks side effects include nausea in 22%-35% fever in 15% diarrhea in 6%-21% vomiting in 7% Vaginal misoprostol: vaginal misoprostol doses used in clinical trials ranged from 400-800 mcg range of reported success rate after single dose of misoprostol 33%-60% at 24 hours success rates improve to 80%-88% with repeat doses higher success rate with incomplete spontaneous abortion than with other types of miscarriage side effects include nausea, fever, vomiting, and diarrhea increase with repeated doses increase with oral or sublingual route compared to vaginal route vaginal misoprostol effective for completing miscarriage within 24 hours and avoiding need for uterine curettage with anembryonic gestation or missed spontaneous abortion before 24 weeks Mifepristone: mifepristone destabilizes implantation site before treatment with misoprostol(4) success rate with combination of mifepristone plus misoprostol > 90% in early pregnancy loss(4) FDA-approved regimen for medical abortion is mifepristone 600 mg orally followed by misoprostol 400 mcg orally 48 hours later, but other regimens may be effective see dosage and administration in mifepristone for additional information mifepristone 48 hours before misoprostol appears no more effective than two doses of oral misoprostol 48 hours apart regardless of management method, follow-up indicated to assure completion of miscarriage and to process experience findings suggestive of completion of Other Disease Description & H&P Diagnosis and Diagnostic Study Clinical Intervention and Clinical Therapies Cardiac: o patients with incomplete or septic spontaneous abortion may present with maternal tachycardia and/or arrhythmia Pelvic: o vaginal bleeding and attempt to quantify amount and duration pelvic exam signs suggestive of first trimester pregnancy loss include open or closed cervix size-date discrepancy on bimanual exam small, contracted uterus products of conception in cervical opening o o miscarriage(1) o repeat ultrasound showing absence of previously documented pregnancy o 80% drop in beta-hCG level one week following passage of tissue if ectopic pregnancy has been excluded, no need to follow betahCG levels to zero for cases where no intrauterine pregnancy has been documented, consider following beta-hCG levels to resolution o in absence of hemorrhage or infection, safe to wait indefinitely for miscarriage to complete without further intervention o patients can switch at any time to medical or surgical uterine evacuation for any management method, counsel patient on signs that require immediate medical attention such as heavy bleeding - soaking through 2 sanitary pads per hour for 2 hours high fever (alert patients receiving medical management that misoprostol may cause fever within 24 hours of treatment and this should not be interpreted as infection) pelvic pain feeling ill several days after miscarriage regardless of management method, counsel patients that normal menstrual periods usually return between 1 and 2 months after miscarriage no medical necessity to withhold any contraceptive method once beta-hCG has returned to zero and products of conception have passed no evidence of medical necessity for delay of next attempt at conception Other