presentation - College of Computing & Informatics
advertisement

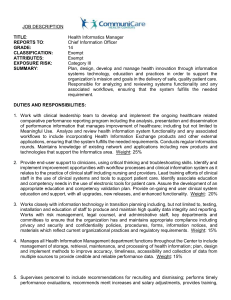
Medical Informatics Perspectives on Electronic Medical Records Scot M. Silverstein, MD Assistant Professor of Healthcare Informatics and IT Director, Institute for Healthcare Informatics Drexel University, College of Information Science & Technology April 20, 2006 Goals • Promote better understanding of Medical Informatics as a formal, cross-disciplinary clinical/IT specialty, lift veil of mystery that leads to misuse of term. • Raise awareness of national electronic medical records (EMR) initiatives on the provider side, and how these are important to healthcare providers as well as other sectors (e.g., pharma). • Provide insights into how Medical Informatics experience in solving provider sector EMR issues is valuable towards parallel issues in pharma and other R&D IT initiatives. The iSchools Focus is on how people seek, use or interact with information using technology, not simply on technologic devices and computer programs. • University of California, Berkeley School of Information Management and Systems • University of California, Irvine The Don Bren School of Information and Computer Sciences • University of California, Los Angeles Graduate School of Education and Information Studies University of Michigan The School of Information University of North Carolina School of Information and Library Science The Pennsylvania State University School of Information Sciences and Technology • Drexel University College of Information Science and Technology • Florida State University College of Information • Georgia Institute of Technology College of Computing Rutgers, the State University of New Jersey School of Communication, Information, and Library Studies • University of Illinois Urbana-Champaign The Graduate School of Library and Information Science Syracuse University School of Information Studies • Indiana University School of Informatics University of Texas, Austin School of Information • Indiana University School of Library and Information Science • University of Maryland College of Information Studies University of Pittsburgh School of Information Sciences University of Toronto Faculty of Information Studies University of Washington Information School Guiding Principles • Clinical IT will significantly benefit healthcare quality, efficiency and costs only if done well. • Clinical computing and business computing (management information systems) are different subspecialties of computing. • People issues are as critical towards success of clinical IT initiatives in the provider sector as well as in other healthcare sectors such as pharmaceuticals. Health-care sector must focus on switch to electronic records Dr. Glenn Steele Jr., president and CEO of Geisinger Health System, Philadelphia Inquirer, April 20, 2006 ( http://www.philly.com/mld/philly/14382256.htm ): An anxious son in New Jersey logs on to the Internet and stays up-to-date on his elderly parents' medical care in Pennsylvania. Doctors at a small community hospital perform a heart test on a newborn, and pediatric cardiologists at a children's hospital 60 miles away monitor the test via advanced video-feed capability. Doctors click on a computer screen and have immediate access to a patient's medical history and test results. Such are the advantages of information technology systems. They make test results available much faster, enable caregivers to provide computer-generated prescriptions and other patient orders, and even remind caregivers to check for certain conditions or schedule tests. Electronic health records make sense, but fully implementing them is a gigantic and formidable challenge that requires patience and a willingness to do things differently. And we have barely begun, though the push for greater use of IT is coming to the health-care industry with the force of a freight train. Like so many other reforms, IT promises to lower costs, increase quality, and transform our bulky system into a more efficient, user-friendly machine … Successfully implementing an electronic health record requires substantial resources for workflow analysis, software, testing, and training - both before and after implementation. To capture any cost and time efficiencies, healthcare organizations must redesign and automate complex work processes. Organizations will also need to find, attract, train, and retain an IT team with the necessary technical and clinical skills. Estimates are that it will take an additional four years to train 10,000 such workers - that's only two per U.S. hospital, with none left over for physician practices. Problems with healthcare IT • A number of very expensive healthcare IT project difficulties and failures have appeared in the literature in recent years in large part due to organizational change resistance, internal political struggles, lack of expertise in IT implementation processes most suitable for clinical environments, and other sociotechnical issues. – – – – UC Davis: clinical IT project is two years behind schedule, over budget, and a fifth of the budget went to an outside consulting firm [ http://sacramento.bizjournals.com/sacramento/stories/2006/03/06/story3.html?page=1 ] Department of Defense EMR. Medical records system assailed [http://www.heraldnet.com/stories/06/04/08/100bus_philpott001.cfm ]. DOD’s new “state of the art” medical record-keeping system has reduced patient access to many military outpatient clinics and has lengthened workdays for many doctors. Hospital of the University of Pennsylvania. Role of computerized physician order entry systems in facilitating medication errors. Koppel et al., JAMA 2005;293(10):1197-203 [ http://jama.ama-assn.org/cgi/content/abstract/293/10/1197 ] Children's Hospital of Pittsburgh, Department of Critical Care Medicine: Unexpected Increased Mortality After Implementation of a Commercially Sold Computerized Physician Order Entry System [http://pediatrics.aappublications.org/cgi/content/abstract/116/6/1506 ] – – – – – Bay Pines, Florida VA hospital CoreFLS failure - $472 million [http://www.usmedicine.com/article.cfm?articleID=932&issueID=66] United Kingdom NHS initiative [Doctors fear £6bn IT project will be a fiasco. The Guardian, February 8, 2005. [http://society.guardian.co.uk/internet/story/0,8150,1407903,00.html] Cedars-Sinai Hospital, Los Angeles [Doctors pull plug on paperless system. American Medical News, Feb. 17, 2003] Others [website Sociotechnical Issues in Health IT: Common Examples of Health IT Failure] Pharma examples – CRISP project - In the 1990s, [pharma] struggled to erect a modernized clinical data system known as CRISP (Clinical and Regulatory Information Strategic Program), a project that current and former information systems workers came to regard as a $100 million fiasco. "This project ran into a lot of problems," says one former manager who was involved near the beginning of the CRISP project. [http://www.baselinemag.com/article2/0,1397,1608582,00.asp] Electronic Medical Records An electronic medical record (EMR) is a computer-based patient medical record. An EMR facilitates access of patient data by clinical staff at any given location accurate and complete claims processing by insurance companies building automated checks for drug and allergy interactions clinical notes prescriptions scheduling sending to and viewing by labs The term has become expanded to include systems which keep track of other relevant medical information. The practice management system is the medical office functions which support and surround the electronic medical record. According to the Medical Records Institute, five levels of an Electronic HealthCare Record (EHCR) can be distinguished: The Automated Medical Record is a paper-based record with some computer-generated documents. The Computerized Medical Record (CMR) makes the documents of level 1 electronically available. The Electronic Medical Record (EMR) restructures and optimizes the documents of the previous levels ensuring inter-operability of all documentation systems. The Electronic Patient Record (EPR) is a patient-centered record with information from multiple institutions. The Electronic Health Record (EHR) adds general health-related information to the EPR that is not necessarily related to a disease. Clinical decision support systems Four key functions (Perreault & Metzger, 1999) • Administrative: Supporting clinical coding and documentation, authorization of procedures, and referrals. • Managing clinical complexity and details: Keeping patients on research and chemotherapy protocols; tracking orders, referrals follow-up, and preventive care. • Cost control: Monitoring medication orders; avoiding duplicate or unnecessary tests. • Decision support: Supporting clinical diagnosis and treatment plan processes; and promoting use of best practices, condition-specific guidelines, and population-based management. National EMR Initiatives: U.S. • Transforming Health Care: The President’s Health Information Technology Plan – http://www.whitehouse.gov/infocus/technology/economic_policy200404/chap3.html – President Bush has outlined a plan to ensure that most Americans have electronic health records within the next 10 years. The President believes that better health information technology is essential to his vision of a health care system that puts the needs and the values of the patient first and gives patients information they need to make clinical and economic decisions – in consultation with dedicated health care professionals. • Office of the National Coordinator for Healthcare IT (ONCHIT)established April 2004 – http://www.hhs.gov/healthit/ National EMR Initiatives: U.K. • National Programme for IT in the NHS – http://www.connectingforhealth.nhs.uk/ – The National Programme for IT, delivered by the new Department of Health agency NHS Connecting for Health, is bringing modern computer systems into the NHS to improve patient care and services. Over the next ten years, the National Programme for IT will connect over 30,000 GPs in England to almost 300 hospitals and give patients access to their personal health and care information, transforming the way the NHS works. – Described as “the world’s biggest government IT project” What is Medical Informatics? • Medical Informatics studies the organization of medical information, the effective management of information using computer technology, and the impact of such technology on medical research, education, and patient care. • Formal, NIH-sponsored field on which NIH has provided many millions of dollars in training grants for ~ the last two decades. • Not as visible as should be to healthcare. Nearly invisible to pharma. Why? NIH training programs in Medical Informatics http://www.nlm.nih.gov/ep/GrantTrainInstitute.html 1-Harvard-MIT Division of Health Sciences & Technology, 2-Yale University, 3-Columbia University, 4-University of Pittsburgh, 5Johns Hopkins University, 6-Medical University of South Carolina, 7-Vanderbilt University, 8-Indiana University - Purdue University at Indianapolis, 9-University of Wisconsin Madison,10-University of Minnesota Twin Cities, 11-University of Missouri Columbia, 12-Rice University, 13-University of Utah, 14-University of California Irvine, 15-University of California Los Angeles, 16-Stanford University, 17-Oregon Health & Science University,18-University of Washington (training is provided by other universities via internal funds as well). The Informatics Subspecialties Why is good clinical IT difficult? • Lindberg: “Computer Failures and Successes”, Southern Medical Bulletin 1969;57:18-21 – • Nemeth & Cook: “Hiding in Plain Sight”, Journal of Biomedical Informatics 38 [2005], 262–263 – • Computer experts per se have virtually no idea of the real problems of medical or even hospital practice, and furthermore have consistently underestimated the complexity of the problems…in no cases can [building appropriate clinical information systems] be done, simply because they have not been defined with the physician as the continuing major contributor and user of the information. Just beneath the apparently smooth-running operations [of healthcare] is a complex, poorly bounded, conflicted, highly variable, uncertain, and high-tempo work domain. The technical work that clinicians perform resolves these complex and conflicting elements into a productive work domain. Occasional visitors to this setting see the smooth surface that clinicians have created and remain unaware of the conflicts that lie beneath it. The technical work that clinicians perform is hiding in plain sight. Those who know how to do research in this domain can see through the smooth surface and understand its complex and challenging reality. Occasional visitors cannot fathom this demanding work, much less create IT systems to support it. Wears & Berg: “Still Waiting for Godot”, JAMA Vol. 294 No. 2, July 13, 2005 – Throwing IT at a health care system to remedy high medication error rates will not be effective unless the organizational reasons for those failures also are addressed. These reasons are hidden in the "messy details" of clinical work: complexity; uncertainty; conflicting goals; gaps in supplies, procedures, and coordination; brittleness of tools and organizational routines. Why is Medical Informatics important? • Clinical IT and its environment are core competence • Recognition that organizations are simultaneously social (people, values, norms, cultures) and technical (tools, equipment, technology). These elements are deeply interdependent and interrelated. Good design and implementation is not just a technology issue but also one of jointly optimizing the combined sociotechnical systems. • Medical Informatics training recognizes these issues and trains crossdisciplinary specialists accordingly. Curriculum example: – Fundamental of computer science Medical language and terminology systems Modeling of medical observations and data Medical coding systems Medical knowledge structures Information organization and flows in medical practice Quantitative models for medical decision making Clinical decision support Medical image processing User interfaces and ergonomics in healthcare Health information systems architecture Security and confidentiality Ethical and legal issues in electronic medical records Organizational and sociological issues in clinical IT projects Metrics and methods for evaluating healthcare information systems Cost and investment issues in healthcare IT Pharma takes note of provider side EMR efforts Nov. 2005: Exploring the Opportunity for Collaboration with Drug & Device Firms in Accelerating IT Adoption by Hospitals & Physicians http://exlpharma.com/events/ev_brochure.php?ev_id=17 Speaking Faculty: Landen Bain, Healthcare Liaison, CDISC Michael Barrett, Managing Partner, CRITICAL MASS CONSULTING Brian Chadwick, Partner, LOOKLEFTGROUP Sue Dubman, Director of Applications for the Center of Bioinformatics, NATIONAL CANCER INSTISTUTE Robert N. Hotchkiss , MD , Director, Clinical Research, HOSPITAL FOR SPECIAL SURGERY Charles Jaffe, MD, Vice President, Life Sciences, SAIC Bill Johnson, President, WILLIAM S. JOHNSON CONSULTING Les Jordan, Life Sciences Industry Technology Strategist, MICROSOFT Stan Kachnowski, PhD, Professor, Health Information & Public Policy, COLUMBIA UNIVERSITY Becky Kush, PhD, President, CDISC Jim Langford, President, DATALABS Gary Lubin, Co-Founder, MERCK CAPITAL VENTURES Somesh Nigam , PhD, Information Management Director, Pharma R&D IM, JOHNSON & JOHNSON PRD Jerry Schindler, DrPH, President, CYTEL RESEARCH Steve Schwartz, Senior Vice President, Business Development, ALLSCRIPTS Martin Streeter, Partner, LOOKLEFTGROUP Barbara Tardiff, MD, MBA, Executive Director, Research Information Services, Clinical & Regulatory Information Services, MERCK & CO., INC. Cara Willoughby, Consultant, Scientific Communications/Regulatory, ELI LILLY AND COMPANY KEYNOTE PRESENTATION Improving Patient Care while Optimizing Efficiency: Outlining the Potential Benefits from Merging Patient Care and Drug Development Efforts Barbara Tardiff, MD, MBA Executive Director, Research Information Services, Clinical & Regulatory Information Services MERCK & CO., INC. HOSPITAL PERSPECTIVE: The Challenges and Limitation of Merging Electronic Health Information Robert N. Hotchkiss, MD Director, Clinical Research HOSPITAL FOR SPECIAL SURGERY STANDARDIZATION EFFORTS: Interchange Standards: The Key to Linking Healthcare and Clinical Research Information Rebecca Kush, PhD, President, CDISC Landen Bain, Healthcare Liaison, CDISC Sue Dubman, Director of Applications for the Center of Bioinformatics, NCI Gartner Predicts 2006: Life Science Manufacturers Adapt to Industry Transitions http://www.gartner.com/DisplayDocument?doc_cd=134309 • The swift and severe judgment in favor of the plaintiff in the first Merck Vioxx trial sent a shock wave through the biopharma industry. It shows that biopharma manufacturers must do more to ensure that healthcare providers and the public have an accurate, ongoing assessment of medication risks. Biopharmas must also ensure that information on these risks is communicated promptly in an open, understandable manner. Posting clinical trial information on a web site is one step towards greater transparency, but does not provide information in a way that [easily] enables ... comparisons of benefits and risks. • ... It is still well recognized that all the possible side effects of a medication cannot be uncovered using [only] a randomized sample of study subjects. The true test of [long-term] safety and efficacy can only be determined when trial data is combined with other sources of information such as clinical encounters, adverse events (MedWatch) or observational studies (National Registry of Myocardial Infarction). • In the future, it is hoped that the EMR system will capture point-of-care information in a standardized format that can be used for drug surveillance. Today, biopharmas must be content with these other available, if imperfect, information stores. Gartner Predicts 2006 (cont.) • Biopharmas ... should look at risk from multiple perspectives ... they must also get actively involved in defining the electronic health and medical record so that it will contain the type of information required to make better safety assessments in the future. • Biopharmas that ignore the opportunity to use analytical tools to proactively review contradictory sources of study information (for example, pre- and post-approval clinical data sets, as well as registries) will miss essential signals regarding product safety. Yet today, only a small percentage of biopharmas routinely utilize personnel with medical informatics backgrounds to search for adverse events in approved drugs. Case Study • What you didn’t want to know about clinical information technology in large medical centers … • Compare issues to your own project difficulties The often divergent goals of three main groups within a medical center From Sittig DF, Sengupta S, al-Daig H, Payne TH, Pincetl P. The role of the information architect at King Faisal Specialist Hospital and Research Centre. Proc Annu Symp Comput Appl Med Care. 1995;:756-60 The Three Stakeholder Groups in More Detail Administration (purchasers) • CEO • COO • CFO • Gen Counsel • CIO • IT staff • Consultant Information Technology (implementers) • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine (users) The undesired dynamics Administration • CEO • COO • CFO • Gen Counsel • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine Medical Informatics as Intermediary Administration • CEO • COO • CFO • Gen Counsel MI • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine The desirable dynamics Administration • CEO • COO • CFO • Gen Counsel MI • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine Medical Informatics role • Responsible for helping these three groups understand they are all working toward the same goal, and ensuring medical center personnel collaborate efficiently and productively. • Understanding and work with the stakeholder drivers (motivators) and dynamics (interactions) in detail will help the MI proactively intervene and avoid retrospective correction after problems have arisen. Observed Drivers: Health System Administration Chief Executive Officer (CEO) Chief Financial Officer (CFO) Chief Operating Officer (COO) General Counsel Institutional reputation Board issues Internal relationships Financial issues Up-front costs (capital & expense) Secondary dollars (longer-term clinical revenue/technologic expense) “Return on investment” Skepticism Operational changes (in processes) Managerial control Staffing Costs Liability / litigation on: Clinical issues Information security Observed Drivers: Information Technology (MIS) Chief Information Officer (CIO) IT Staff Consultants Budget - effects on other projects, especially MIS (management information systems) “Plug and Play” - ease of implementation, human resource s IT control - territoriality IT reputation - insecurity in new clinical domain Fear - clinical environments are alien to MIS Hands-on technology issue s Job stability Revenue Client satisfaction Future engagements Observed Drivers: Clinicians Clinical Leadership (Chief of Staff, VP for Medical Affairs, Department Chairs, Nursing VP) Clinicians (primary users) Service Line Administrator Change to clinician workflow Complaints Care issue s Usefulne ss of system (dataset issue s, adaptability - opposite of plug and play) Work changes / time issue s Effects on care quality Liability “Grading” & physician practice reporting Income Effects on busine ss development Institutional reputation Clinician relations Case highlights - Invasive Cardiology • 6,000 procedures/year. EDC system sought for new device and modality trials and evaluation, PI, benchmarking, operations reporting, inventory. • In house development/customization ruled out by CIO - turnkey policy - despite clinician judgment. • 2 year analysis, market investigation, K-T, business process as for accounting system. Skepticism/fear/delay • Vendor product acquired but sat unused for almost a year before operationalization was considered skepticism by CIO, COO, clinicians • Only .75 FTE's assigned. MIS person chosen had no experience working in tough, high-volume, critical care areas. Scared. Beginnings of conflict • A Steering Committee was initiated, led by cardiac services executive relatively unfamiliar with IT • CIO, IT staff adamant that vendor product should not be modified even though clinicians wanted the data and workflow components of the package to be adjusted to their busy clinical environment and customs (rather than the other way around). • MIS department began to blame the physicians for being "non-cooperative" with them, stubborn, unable to finalize decisions about the package, and responsible for lack of project progress. Conflicts increase • Cardiac services administrator blamed for "not controlling the doctors.” Pushed for install. • Unstable platform, kept crashing, losing data. • Attempted install in the cath lab went so poorly, and was so misaligned with needs, expectations, work flow, and the tremendous patient responsibilities, that the demoralized and frustrated cath lab staff demanded in a hostile tone that the MIS people "get out of our cath lab!" • Loud complaints to Chairs, Sr. VP Med Affairs, CEO • Large political battle in high revenue area (25%) Medical Informatics as intermediary • Consultant called in; unable to resolve problems (fear of being tough). • COO / CFO skeptical of benefits of project altogether, wanted to kill project, $500K already spent, relations disrupted • Medical Informaticist hired by CEO/Sr. VP to mediate / resolve issues • MI investigates: finds many changes needed, creates 10-point plan and phased timeline oriented to clinical realities Remediation begins • Move to stable platform suitable for cath lab environment resisted by CIO & IT staff due to resources involved, but pushed through by informaticist through persuasion of key stakeholders, especially CEO, COO, Sr. VP • Informaticist created collaborative and participatory work team environment, a non-traditional methodology in MIS but crucial for clinical computing settings (Participatory Design of Information Systems in Healthcare, Sjoberg C, Timpka T: Journal of the Amer. Medical Informatics Assoc. 1998;2:177-183). • New IT “can-do’s” hired, increased independence from central IT control, again through persuasion Remediation continues • Cardiologists given major input to steering committee and workgroups and report development • MI identified criticality of data remodeling for the cardiologist's needs - and led the effort (IT personnel or clinicians alone could not do) – core competency of MI. • New data model crafted collaboratively, consistent w/lab practices and national standards but far surpassing the latter to meet day-to-day needs. ACC dataset problems identified. • Dictation allowed to supplement case report generation so clinicians not “boxed-in” Rapid improvement • Clinicians, service administrator, COO representative allowed to define statistical reports and definitions/terminology. • Meet desire for research data, performance improvement, operations improvement while allaying fears of inaccurate “report cards.” • Agile methodologies (e.g., iterative and incremental development) approach was SOP. Not as possible in pharma due to validation and other regulatory requirements, but some degree of avoidance of “process zealotry” and “methodological fanaticism” possible and advantageous • System in use within 6 months by 75% of staff, enthusiastic committee meetings Success • System allowed improved scheduling, lab operations and staffing planning, outcomes assessment, participation in national initiativesAmerican College of Cardiology (ACC), Society for Thoracic Surgery (STS), and Genentech National Registry of Myocardial Infarction (NRMI). • Received recognition for excellence by national cardiology figures, and JCAHO. Source of conflict became source of pride. • Trust built with clinicians allowed inventory module to be rapidly implemented (months) • $1 million savings realized the following year. Conclusions • Clinical IT projects are complex social endeavors in unforgiving clinical settings that happen to involve computers, as opposed to information technology projects that happen to involve doctors. • An understanding of the internal personnel dynamics by the medical informaticist is an important asset towards facilitating success. • This understanding and experience should be [is] portable to pharma and can be of great value in eClinical initiatives and in collaborations with the provider side. Additional Reading • Organizational Aspects of Health Informatics: Managing Technological Change. Nancy M. Lorenzi, Robert T. Riley (Springer-Verlag, 1995). • Advance for Health Information Executives: “Medical Informatics, Friend or Foe”, Robert Gianguzzi, May 1, 2002, p. 37-38 Dean Sittig, Director of the national Clinical Informatics Research Network (CIRN) for Kaiser Permanente: "There are many different constituencies, and hence views, which must be considered when attempting to develop an integrated clinical information management system in any large medical center ... we believe that without a full-time, on-site [medical informaticist], the difficulty of the task increases to the point of becoming nearly impossible."