Peds GI, Altered Fluid
advertisement
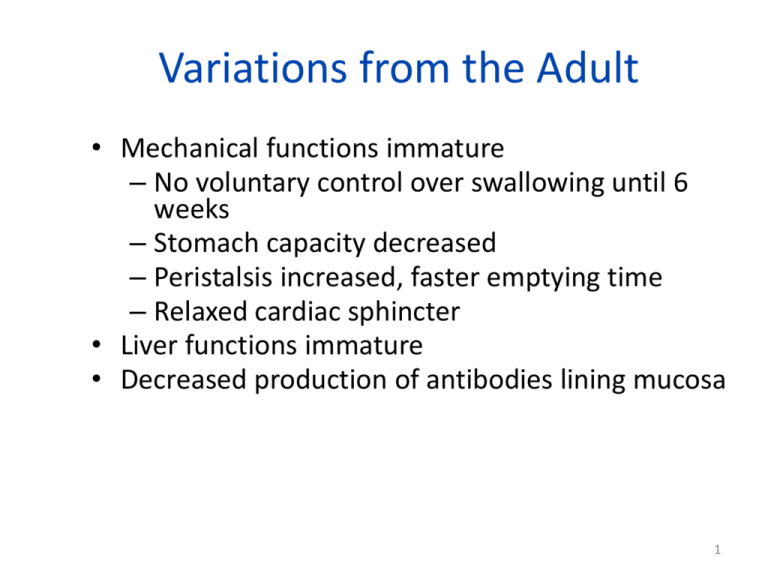
Variations from the Adult • Mechanical functions immature – No voluntary control over swallowing until 6 weeks – Stomach capacity decreased – Peristalsis increased, faster emptying time – Relaxed cardiac sphincter • Liver functions immature • Decreased production of antibodies lining mucosa 1 Variations from the Adult (cont) • Digestive processes not mature until toddlerhood – Gastric acidity low until school age – Decreased saliva & ability to digest starches • No voluntary control of elimination until myelinization of spinal cord. 2 Categorization of Conditions • • • • • Developmental (congenital) Problems w/motility Inflammation or infections Obstructive disorders Malabsorption conditions 3 Fluid & Electrolyte Differences • • • • • Percent body water /total body weight Infant higher percentage fluid ECF Greater insensible loss Renal function immature Infants unable to communicate thirst 4 Maintenance Fluid Requirements per 24 hours • ≤ 10 Kg: 100 ml/kg/day • 11-20 kg: 1,000 ml + 50 ml/kg/day • >20 kg: 1500 ml + 20 ml/kg/day 5 Minimum Urine Output • Infants, toddlers – >2-3 ml/kg/hr • Preschool, young school-age – >1-2 ml/kg/hr • Older school-age & Adolescent – 0.5-1 ml/kg/hr 6 Etiology of Fluid Imbalances (the “related to”) • Imbalance of intake vs output • Result: fluid volume deficit or fluid volume excess • Secondary to therapy or disease process – All organ systems can be cause 7 Types of Dehydration • Isonatremic • Hyponatremic • Hypernatremic • Normal serum Na = 135-145 mEq/L F 8 Key Factors in Diagnosing Dehydration • • • • History of acute or chronic fluid loss Serum electrolyte values Clinical manifestations Weight of the child F9 Clinical Manifestations • • • • • • • Level of consciousness Urine output Weight Pulse Cap refill Respirations Skin turgor 10 F Clinical Manifestations (cont) • • • • • • • Mucous membrane Blood pressure Fontanel Thirst Sunken eyes No tears “toxic looking” 11 Cleft Lip and Palate • CL: the lip does not completely form during fetal development • CP: Nonunion of the tissue & bone hard/soft palate during embryologic development. 12 Problems: cleft lip/palate • • • • Feeding difficulties Speech & language difficulties Ear infection and hearing loss Dental problems 13 Surgical Management • Cheiloplasty: correction of cleft lip – Functional & cosmetic – age 3-6 mo (McKinney) – “rule of 10s”: 10 weeks, 10 lbs, Hgb of 10 g/dL • Palatoplasty: cleft palate repair – 6 mo to 2 yrs (most: 1 year) – Before speech – Able to take liquids from cup 14 Nursing management: preop • Feed in upright position • Burp frequently, w/ periods of rest • Large-holed nipple or rubber-tipped syringe • Finish feeding w/H2O • Small, frequent feedings • Emotional support 15 Nursing Diagnoses – Pre-op Post-op cleft lip • Patent airway • Assess for hemorrhage • Protect the operative site !!! – No pressure on cheeks – No prone position – Elbow restraints • Pain relief • Feed when awake • Keep site clean – prevent infection 17 Post-op cleft palate Immediate post-op goals • Airway – OK to be on side or abdomen – drain secretions • Pain • Prevent injury to suture site 18 Instructions to Mother Risk for injury to surgical site • Progress diet • Only cups for liquids • Provide soft toys • Elbow restraints • Cleanse mouth after eating • No rough play 19 Long-term care CP Team approach • Hearing evaluation • Speech & language therapy • Dentist, orthodontist • Plastic & maxilofacial surgeon • Social worker 20 Other Developmental Gastrointestinal Defects • Esophageal atresia with tracheoesophageal fistula • Imperforate anus • Gastroschisis • Omphalocele • Umbilical or diaphragmatic hernia F 21 GER • Physiologic • Functional – Painless, frequent emesis after meals – No failure to thrive – 40% asymptomatic by 3 months – 70% asymptomatic by 18 months – Medical management very effective 22 Therapy for Gastroesophageal Reflux Disease • • • • • • • Diet Positioning Lifestyle change Acid-suppressant therapy Prokinetic therapy G-tube Surgery – Nissen Fundiplication F 23 Constipation and Encopresis [information only] • Definitions • Common causes of constipation – dietary transition – voluntary withholding • Emotional issue • Treatment 24 Inflammatory or Infectious Conditions • • • • • • Necrotizing Enterocolitis (NEC) Appendicitis Inflammatory bowel disease Viral gastroenteritis Hepatitis Parasites 25 Appendicitis - diagnosing • History – Pain, then vomiting • Ultrasound • CT 26 Treatment • Uncomplicated: may watch – Rehydration, Antibiotics prior to surgery • Complicated – Surgery – Non-operative: fluid replacement, IV antibiotics, analgesics 27 Interventions Uncomplicated Appendicitis Pre-op • • • • • • VS Comfort measures No enemas, laxatives No heat to abdomen IV fluids, abx Monitor for perforation Post-0p • • • • • Laparoscopic Pain control C & DB Early ambulation NPO until bowel function returns 28 CMs of perforation: Sudden relief from pain, then increased pain Rigid abdomen Early shock Infants: refusal to eat, behavior changes Danger: peritonitis 29 Appendicitis: perforation &/or abscess Surgical or medical management Percutaneous drainage of abscess NG tube IV fluids and Antibiotics Drains Pain med: ATC Routine post-op: C&DB, move Monitor for sepsis, abscess 30 Obstructive Disorders • Hypertrophic Pyloric Stenosis • Hirschprung’s Disease • Intussusception 31 Hypertrophic Pyloric Stenosis F Post-op Pyloromyotomy • Nursing priorities –Hydration status –Pain –Infection 33 Hirshprung’s Disease Typical Presentation • 2 1/2 week old child • Poor weight gain • 38 weeks gestation • Easily takes 2-3 oz of formula • Has frequent vomiting after feeds, some bile-stained • Constipation • Dx: rectal biopsy 34 Celiac disease: definition • Immune-mediated disease induced by ingestion of defined proteins in subjects who are genetically predisposed • EBP: exclusive 6 month breast feeding delays onset of sx. 35 Patho: Celiac Disease F Celiac Disease – Assessment “classic” • • • • • • Symptoms 3-6 mo after gluten introduced Steatorrhea Abdominal distention, vomiting, anorexia Growth retardation, muscle wasting Anemia During crisis: severe dehydration 37