Evaluation and Treatment of Mood Disorders
advertisement
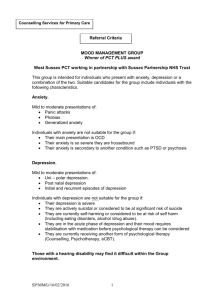
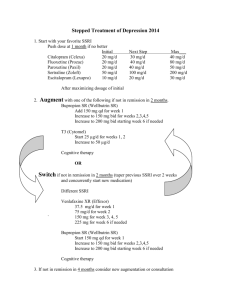
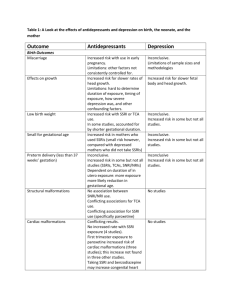
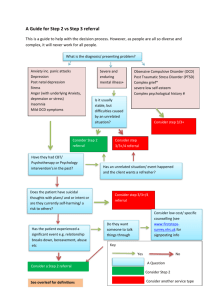
Pharmacology of Antidepressants and Anti-anxiety Agents Aneet Ahluwalia, MD Assistant Professor of Psychiatry and Internal Medicine Case • 47-year-old woman presents to PCP with CC: fatigue. She indicates that she was promoted to senior manager in her company approximately 11 months earlier. Although her promotion was welcome and came with a sizable raise in pay, it resulted in her having to move away from an office and group of colleagues she very much enjoyed. In addition, her level of responsibility increased dramatically. • The patient reports that for the last 7 weeks, she has been waking up at 3 AM every night and been unable to go back to sleep. She dreads the day and the stresses of the workplace. As a consequence, she is not eating as well as she might and has dropped 7% of her body weight in the last 3 months. She also reports being so stressed that she breaks down crying in the office occasionally and has been calling in sick frequently. When she comes home, she finds she is less motivated to attend to chores around the house and has no motivation, interest, or energy to pursue recreational activities that she once enjoyed such as hiking. She describes herself as "chronically miserable and worried all the time." • Her medical history is notable for chronic neck pain from a motor vehicle accident for which she is being treated with tramadol and meperidine. In addition, she is on propranolol for hypertension. The patient has a history of one depressive episode after a divorce that was treated successfully with fluoxetine • CBC, TSH, CHEM 7 WNL. Criteria for Major Depression -SIGECAPS, anhedonia or depressed mood, impairment in functioning Major Depression Epidemiology • Point Prevalence males 2-3 %, females 4-9% • Lifetime Risk males 7-12 %, females 20-25% • Major Depression is 4th leading cause of disability worldwide (this is probably an underestimate) Risk Factors for depression • • • • • • • Family history of mood disorder Previous Episode Stress Emotional trauma Childhood abuse/neglect Elderly (over 65) Marital factors (single, separated, divorced, or unhappily married) Risk Factors for depression-Cont • • • • • • • • Substance abuse Physical illness Heart disease Diabetes Obesity Cancer Menopause Rhematoid arthritis Prevalence of Depression in Medical Illnesses Setting / Disease Outpatient Inpatient Diabetes Stroke Cancer Myocardial infarction Rheumatoid arthritis Parkinson’s disease Prevalence Rate (%) 2-15 12 9-27 22-50 18-39 15-19 13 10-37 Musselman et al., Arch Gen Psych 1998, Biol Psych 2003; Cohen-Cole & Kaufman, Depression 1993 Depression-consequences • • • • • Suicide Suffering Impaired relationships Impaired job/school performance negatively influence other medical conditions and is a risk factor for medical M&M • Co-morbid anxiety is common, and can increase suicide risk Genetics or Environment? • Genetics and Environment both contribute • Commonly accepted theory is that multiple gene loci are implicated, and these loci make people more vulnerable to environmental stressors, leading to increased risk for MDD • Why not one gene? Because depression is a heterogeneous disorder that is not just one entity (different subtypes of depression), with different biological, psychological, and social causes Presentation • Adults can present with various somatic complaints (such as lower back pain, headache, CV, GI, GU) or decreased energy rather then complaints of depression • Elderly can present with cognitive deficits (pseudodementia-poor effort) as well as somatic complaints Treatment • Depression can be treated with psychotherapy, with medication, or with the combination of therapy and medication • For moderate to severe, medication plus therapy is the best option • Placebo response ~0.4 compared to antidepressant response ~0.7 Possible Biological Markers • Decreased BDNF in serum • Low tryptophan, 5HT, and 5HIAA (metabolite of 5HT) in postmortem suicide patients • Polymorphisms of 5HT1a receptors with decreased affinity for 5HT have been shown to increase risk for depression when stressed • We can induce depression by tryptophan restriction (tryptophan is a precursor to 5HT) • Norepinephrine and Dopamine are thought to be low in depression Symptoms clusters and Neurotransmitters General Anxiety, obsessional depressive thoughts Serotonin dysfunction Anhedonia, psychomotor retardation Dopamine dysfunction Panic Gaba dysfunction fatigue, poor concentration Norepinephrine dysfunction Antidepressants/Antianxiety • • • • • SSRIs-prevent reuptake of serotonin (5HT) SNRIs-prevent reuptake of serotonin and NE DNRI-prevent reuptake of NE and D MAOI-prevent breakdown of monoamines 5HT1A partial agonist • • • • BZD/anticonvulsant-increase action of Gaba Antihistamine Block alpha 1, alpha2 agonist Beta blockers Brain Imaging findings in depression • Decreased frontal blood flow (~7 %) • Lower hippocampal volume HPA-hypothalamic pituitary adrenal axis Stress causes a release of CRH, ACTH, and ultimately cortisol. This is beneficial, as we need the increased glucose it causes and increased blood pressure to deal with the stressor at hand. HPA- stress • When exposed to chronic or extreme stress, cortisol, ACTH, and CRH levels are at higher levels, and stay elevated for longer periods of time So what? We’re not endocrinologists • Cortisol and CRH have been shown to cause damage to hippocampal neurons by causing decreased dendritic branching and decrease in pyramidal neuron spines What does BDNF do? • Promotes synaptic plasticity, neuronal growth, neuronal spine formation, especially in hippocampus • Also helps cell survival and resilience • Reduces apoptosis • Shown to be low in patient with depression • Increased BDNF expression in hippocampus of depressed patients treated with antidepressants compared to untreated How do stress and hormones cause these neuronal changes • Stress and glucocorticoids supress expression of Brain derived Neurotropic growth factor. • Decrease in volume of hippocampus is proportional to length of depression • Prozac has been shown to increase hippocampus synaptogenesis in rats after 5 days treatment (?mechanism of action?) Examination of Cues-evolution • LOSSES that cause sadness are of reproductive resources • Money, a mate, reputation, health, relatives, friends…. • These things, in theory, would have increased reproductive success (evolutionarily speaking) LOSS = Signal of Maladaptive Functioning • If Loss triggers sadness • And • If sadness changes our behavior to stop current losses, and prevent future ones…. • Then • That would be useful, indeed! Medical causes of depresion • • • • • • • • Hypothryoidism Stroke Multiple sclerosis hyper/hypo parathyroidism Addisons disease Cushings disease Hypopituitarism Anemia Anxiety Response Cues Panic = fear imminent death Social = fear embarrassment PTSD = emotional memory of trauma OCD = intrusive obsessions GAD = free-floating; no conditioned specific triggers Generalized Anxiety Disorder • prevalence of GAD of 5.1 percent to 11.9 percent. More common in women than men (2 to 1) • One of the most common illnesses you will encounter in primary care as it is common in the medically ill. • Associated with increased health care utilization Generalized Anxiety Disorder aka GAD • Excessive worrying that is difficult to control occurring more days than not for 6 months causing significant distress/impairment "Do you worry excessively about minor matters?“ GAD 3 of the following symptoms Restlessness easy fatigued or poor sleep difficulty concentrating Irritable muscle tension GAD • Usually fairly chronic • Hereditary component—shared neuroticism, depression and GAD • Learned behaviors • Environmental triggers • GAD in adult life is associated with a higherthan-average number of traumatic experiences and other undesirable life events in childhood GAD -treatment • Therapy and meds both effective as is the combination • SSRIS first line, other agents helpful as well such as SNRIs and BZDs • Adjunctive treatment –accupuncture, yoga can be helpful Panic disorder --classic, discrete episodes of intense fear that begin abruptly and last for several minutes to an hour. --often have chest pain, feeling of rapid heartbeat, or shortness of breath – frequently precipitating an emergency room visit. --recurrent, unexpected panic attacks, and one month or more of either worry about future attacks or consequences, or a significant maladaptive change in behavior related to the attacks, such as avoidance of the precipitating circumstances, agoraphobia can occur. Treatment for Panic • Meds and Therapy are both equally effective, combo is slightly better • SSRIS first line, BZDs as well and SNRIs OCD OCD Obsessions contamination pathological doubt aggressive impulses somatic concerns need for symmetry sexual impulses OCD Compulsions cleaning washing checking excessive ordering/arranging counting repeating collecting OCD 2-3% Americans (or 1 in 50) Men=women Onset generally in adolescence or early adulthood Chronic waxing and waning course Fist line treatments are SSRIs and CBT Selection of Medication • Family History of response • Past treatment response • Specific symptoms (with anxiety SSRI, Low energy SNRI or WB) • Medication interactions • Medical conditions • Side effect profile • *important to educate about SE, what to expect, and length of time for response to increase compliance (don’t sensitize them) SSRIs prevent reuptake of serotonin Take 2-6 weeks for full effect, usual length of treatment at least 3-6 months 5HT1 - fights depression 5HT2 - tremors, sweating, decreased libido, activation 5HT3 – nausea, diarrhea (ondansetron blocks this receptor) SSRIS • Some DDIs- tramadol, mepiridine, dextromethorpan, linezolid, tamoxifen, clopidogrel Fluoxetine=Prozac -10-80 mg titrate to effect -Long half life -activating and ass with weight loss -start at 10 & increase to 20 after ~1 week -Inhibits 2D6 raising levels of beta blockers, also lowers level of active metabolite of clopidigrel, avoid with tamofixen Citalopram and Escitalopram • Citalopram is a mixture of 2 enantiomers while escitalopram is just the more active enantiomer • 5 mg escitalopram=10 mg citalopram • Maximum mean prolongations in the QTc intervals were 8.5 and 18.5 ms for 20 and 60 mg citalopram, respectively Sertaline=zoloft • Start 25 and increase to 50. 200 mg max • Effective, generic • Most studied SSRI in pregnancy and breast feeding and 1st line • Inhibits 2D6--Increased beta blocker, decreased active metabolite of tamofixen, decreased levels of active metabolite of clopidogrel • More nausea/diarrhea than other SSRIS? Paroxetine=Paxil • Most sedating, most weight gain, worst discontinuation syndrome • Start at 10 mg and titrate up • Has anticholinergic and antihistaminergic activity • DDIs - can increase beta blockers and lower levels of active metabolite of tamoxifen Fluvoxamine-luvox • Marketed for OCD • Not used as often • 50-300 mg SSRI possible side effects • • • • • • • • • • • • • Appetite loss or Increase Weight gain, weight loss Nausea, Diarrhea Decreased libido, delayed ejaculation or anorgasmia (10-30 %) Akasthisia –inner restlessness (rare, usually at start) Fatigue, sleepiness or sleeplessness (can use Benzos or newer sleep medications as needed short term) Long term use can cause apathy at high doses Can cause hypomania or mania in bipolar patients Dry mouth Hyponatremia/SIADH (rare) Vivid dreams Increase in suicidal ideation in adolescents QT prolongation Rare serious side effects • Serotonin syndrome- rare, presents with high fevers, sweating, diarrhea, myoclonus, hyperreflexia, muscle rigidity, tachycardia, hypertension, elevated CK, nausea. • Risk factors: combining SSRI and MAOI, using higher doses and multiple serotonergic medications (meperidine, tramadol)—also can cause seizure • Dextromethorphan not contraindicated, but does increase serotonin levels • Treatment involves IV fluids and Benzos, dantrolene can also be used. • Perfect patient for SSRI • Depression and anxiety patient in initial casethough consider tramadol decrease or cessation SNRIs • Work by blocking reuptake of 5HT and NE • Can be more activating due to NE aspect • Norepinephrine aspect may be helpful for chronic pain • Dose dependent increase in BP in ~10% can be 10 mm • Similar side effects to SSRIs but can have more GI upset Venlafaxine • Venlafaxine-effexor 37.5mg-300, at lower doses more serotonergic, at higher doses more noradrenergic • Significant discontinuation syndrome Duloxetine • 20 - 60 mg • Also approved for fibromyalgia and diabetic neuropathy • not as severe discontinuation as venlafaxine • DDIs - can increase beta blockers and lower levels of active metabolite of tamoxifen SNRI Perfect patient • Depressed patient with anxiety symptoms, low energy level, and chronic pain—diabetic neuropathy or FMG Bupropion • Bupropion (wellbutrin) NE and Dopamine reuptake inhibitor, 50-300 mg • Works well for low energy (can augment SSRI), avoid in highly anxious patients • Also used for smoking cessation • Low incidence of sexual dysfunction • Lowers seizure threshold (dose related), relative contraindication with epilepsy and bullemia, anorexia • DDIs - can increase beta blockers and lower levels of active metabolite of tamoxifen DNRI patient • Low energy depression, wants to quit smoking, limited physical symptoms of anxiety, wants to avoid sexual side effects, pt. overweight DDIs • Tamofixen is metabolized by 2D6 into active metabolites • Plavix is metabolized by 2C19 into active metabolites Psychiatry and Medicine • paroxetine, bupropion, fluoxetine, sertraline, duloxetine inhibit 2D6-- to be avoided with tamoxifen (2D6) • These same medications increase levels of many other medications including beta-blockers. • fluoxetine, sertraline inhibit 2C19 --avoid with clopidogrel mirtazapine • Good for anxiety/depression • Blocks PRE synaptic alpha 2-adrenoceptors = increasing synaptic 5HT and NE • Blocks POST synaptic 5-HT 2 (less sexual SE) and H1 histamine receptors (Sedating, increased appetite and weight gain) • 5HT3 antagonist like ondansetron • 7.5-30 mg, dose inversely proportional to sedation Ideal mirtazapine patient • On Chemotherapy for colon cancer-depressed, anxious, nauseus, decreased appetite, weight loss, poor sleep Trazadone Trazadone- Very sedating, often used to treat insomnia, works as antidepressant at higher doses, low sexual side effects Antihistaminergic effect helps sleep • Priapism (1/1000-1/5000) due to alpha 1 blockade • Used as an adjunct to SSRIs for sleep Tricyclic Antidepressants • Prevent reuptake of 5HT and NE, helpful in chronic pain • Very effective, but not as well tolerated as SSRIs • Alpha 1 blockade cause orthostatic hypotension and dizziness • Anticholinergic (blocks muscarinic receptors causing dry mouth, blurred vision, urinary retention, constipation) • Antihistaminergic (blocks H1 causing sedation and increased appetite/weight gain) Tricyclic Antidepressants • Use blood levels to monitor response and compliance • Can be lethal in overdose (2-3 grams) due to prolongation of QT interval (treated with bicarbonate) Tricyclic Antidepressants Tertiary amines • Imipramine • Amitryptiline • Clomipramine • Doxepin Secondary amines Desipramine Nortryptiline Protryptiline less sedating less hypotension less anticholinergic Discontinuation syndrome • TCA : cholinergic rebound (sweating, N/V/D) • SSRI : agitation, nightmares, anxiety, dizziness, parasthesias (paroxetine worse than other SSRIs) • SNRIS: venlafaxine and cymbalta can have worse discontinuation than SSRIs • Prevention-slow taper MAOI • Monoamine Oxidase Inhibitors (MAOIs) • MAO-A --- metabolizes 5HT and NE selectively --- metabolizes certain amines, linked to blood pressure • MAO-B --- protects neurons by metabolizing certain amines such as protoxins into toxins that may cause neuronal damage MAOIs MAOIs inhibit MAO in CNS, gut (leads to increased tyramine absorption which acts as false neurotransmitter and elevates BP) hypertensive crisis Avoid aged cheese/wines/tyramine foods 2 weeks to replenish MAO supply Interactions: =, serotonin syndrome w/ SSRI/TCA- DC SSRI 2-5 wks before starting MAOI (DC MAOI 2 wks before starting SSRI), opioids (autonomic instability, delerium, death), sympathomimetics, oral hypoglycemic potentiation MAOIs • Classic MAOIs--irreversible and nonselective • (MAO-A and B enzyme activity can not be restored unless new enzyme is synthesized) • Phenelzine, Tanylcypromine, Isocarboxazid • Reversible and selective inhibitors of MAO-A (RIMAs) • Moclobemide (antidepressant action) Selegiline (now has a transdermal patch which at the low dose 6 mg, has no diet restrictions) What not to do You are starting a pt. being treated for MRSA/gram positive drug resistant infection on an SSRI—what medication should you make sure they are not taking? Linezolid is an MAOI What can you do? Pt. with depression on celexa has a cough and asks what he can take for his cough. What shouldn’t he take? dextromethorphan Be aware 55 year old with chronic back pain currently taking gabapentin, and norco alternating with tramadol PRN. What DDI should you be aware of before starting SSRI/SNRI? Tramadol has SNRI activity—higher risk for serotonin syndrome and seizure PTSD: medications SSRIs: ameliorate re-experiencing, avoidance, hyperarousal Alpha-adrenergics: prazosin helps with nightmares Beta- blockers Can use other medications as well such as mood stablizers and antipsychotics, evidence not as good, lamotrigine has been shown to be beneficial Alpha 1 blockade • Prazosin has been helpful in nightmares in PTSD, start at 1 mg and titrate up as tolerated – SE: sedation, orthostasis Sedative-Hypnotics GABA-ergic Effects on GABAA Cl- Ion Channel • GABA: Opens Cl¯ channel • Binding sites: •BZD, only w/GABA •Enhance GABA affinity •Barbituate, +/- GABA •Prolong channel open time •EtOH binding, +/- GABA • Enhance GABA affinity • Other binding sites •non-BZD zolpidem/zoleplon, picrotoxin, anti-convulsants Sedative-Hypnotics Benzodiazepines • TYPE I (BZ1/omega1) – Primarily in cerebellum – Anxiolytic properties – Less sedative properties • TYPE II (BZ2/omega2) – Located in cortex, hippocampus, spinal cord – NO anxiolytic properties – Sedative & muscle-relaxant properties of BZD • TYPE III (omega3) – Located in peripheral tissue (kidney) – NO anxiolytic properties – ? Other properties BZD Receptor Activity FULL AGONIST ANXIOLYTIC PARTIAL AGONIST ANXIOLYTIC ANTAGONIST NO CLINICAL EFFECT SED-HYPNOTIC MYORELAXANT ANTICONVULSANT AMNESTIC DEPENDENCY Can cause convulsion PARTIAL INVERSE AGONIST FULL INVERSE AGONIST PROMNESTIC PROMNESTIC ANXIOGENIC ANXIOGENIC PROCONVULSANT CONVULSANT Sedative-Hypnotics BZD differences BENZODIAZEPINES • • • • • • • • • • • • • • triazolam/Halcion 0.125-0.25 mg/d (short) alprazolam/Xanax 0.75-4 mg/d (short) oxazepam/Serax 30-120 mg/d (short) chlorazepate/Tranxene 15-60 mg/d (intermediate) lorazepam/Ativan 1-10 mg/d (intermediate) estazolam/Prosom 0.5-2 mg/d (intermediate) temazepam/Restoril 15-45 mg/d (intermediate) clonazepam/Klonopin 0.5-5 mg/d (intermediate) chlordiazepoxide/Librium 10-100 mg/d (long) diazepam/Valium 2-40 mg/d (long) flurazepam/Dalmane 15-45 mg/d (long) quazepam/Doral 7.5-15 mg/d (long) prazepam/Centrax 20-60 mg/d halazepam/Paxipam 60-160 mg/d BZDs are Evil • Abuse potential Decreased when properly prescribed and supervised • Dependence May occur at usual doses taken beyond several weeks • Withdrawal May occur even when discontinuation is not abrupt (e.g. by 10% Q3D); more likely after long-term treatment Symptoms: tachycardia, HTN, mm cramps, anxiety, insomnia, panic attacks, memory/concentration impairment, perceptual disturbances, derealization, hallucinations, hyperpyrexia, SZ. Most common in Panic DO • Rebound anxiety Return of target symptoms, with increased intensity BZDs Are Not Evil • • • • • • • • Rapid anxiolytic effect (30 mins) No worsening of anxiety at initiation (like SSRI’s can) Improve sleep onset and subjective quality Extensive evidence of efficacy in MOST anxiety disorders (less true for OCD, and not so true for PTSD) Relatively safe in OD (winning favor over barbituates in 60’s) Can Use 2-4 weeks to cover anxiety exacerbation caused by antidepressant initiation Use PRN before exposure to a feared situation Long term augmentation or mono-therapy is usually reserved for treatment-resistant (to other anxiolytics) buspirone (5HT1A partial agonist) Pharmacodynamics/Pharmacokinetics Onset of action: weeks (vs. days) BID or TID dosing NO sedation NO performance impairment NO cross-tolerance with BZD’s (BUT response less favorable if pt recently taken BZD ie. WD sx) • NO tolerance or withdrawal (compare w/ BZD and AD’s) • NO abuse potential; safe in OD • Demonstrated efficacy in GAD (to • • • • • BZD); • also augments MDD, OCD; useful in aggression/agitation • Strong 3A4 inhibitor buspirone Adverse Effects • • • • • Nausea Headache Insomnia, nervousness Restlessness Dizziness, lightheadedness • All minimized by slow ascending regime (by 10mg q week) clonidine/Catapres guanfacine/Tenex Alpha 2 agonist Useful in blocking NE aspects of anxiety: tachycardia, dilated pupils, sweating, tremor; same for detox from ETOH/barbs/heroin/BZD Less powerful in blocking emotional aspects of anxiety Beta blockers • For performance anxiety, block post synatpic noradrenergic receptors—helps physical symptoms of anxiety (racing heart, trembling) OFF Label • Zolpidem (an imidazopyridine); zaleplon (a pyrazolopyrimidine) – Bind near GABA site – Use: mostly insomnia – Caution: tolerance to effect is common, sleep behaviors Melatonin can help sleep, Ramelteon • Trazadone (brand name Desyrel) – Dosing 50-100mg tid, maximum 400mg/day – Cautions: postural hypotension; priapism Off Label • Sedating Antihistamines – Examples • • Diphenhydramine (Benadryl) Hydroxyzine (Atarax, Vistaril), 25-100mg/dose, up to 400mg/day – Benefits: less-addictive, virtually no side effects • • • Quetiapine and other new generation anti-psychotics 25-100mg/dose, bid-tid – Uses: use as a anti-anxiety or sedative is off-label – Benefits: non-addictive(?); no affinity at BZD-sites; 5-HT activity, possible anti-depressant qualities – Cautions: metabolic syndrome; tolerance to sedation; black box in elderly; orthostasis Chlorpromazine (brands: Thorazine – 25-50mg tid – Benefits: non-addictive, no metabolic syndrome, PO and IM – Cautions: Ach, EPS (low risk) Off label • TCA’s (e.g., amitriptyline, nortriptyline, imipramine, doxepin) – – – – Use low doses 10-25mg tid; or 25-100mg qhs Uses: sleep Benefits: non-addictive Cautions: cannot use PRN, cardiac adverse effects, lethality • Barbituates • Wellbutrin-NE/DE RUI -- bupropion can be activating, not used often for anxiety – Phenobarbtial, butalpital – Addictive, very long acting – In some common meds, e.g., fioricet A word on… ANTICONVULSANTS • Related to BZDs and GABA – Most seem to potentiate GABA – Some may act on intracellular calcium channels – Some block NMDA/glutamate (block excitatory NT, enhance inhibitory effect) – Sedation, Withdrawal, dizziness– renally cleared • Gabapentin (Neurontin): At least 1 RCT shows effectiveness in panic disorder and Social anxiety • Lamotrigine (Lamictal): At least 1 RCT shows effect in PTSD • Pregabalin (Lyrica): – Many controlled RCTs with effect in GAD – At least one RCT for pregabalin in Social phobia Anticonvulsants • Gabapentin and pregabalin-renally excreted no hepatic metabolism. Side effects include sedation and dizziness and edema. Tolerance, withdrawal, and dependence are possible but less common than BZD • Topiramate and zonisamide- carbonic anhydrase inhibitors associated with weight loss • Divalproex—monitor hepatic function, increased weight