Turning Questions into Trials: Innovation in
advertisement
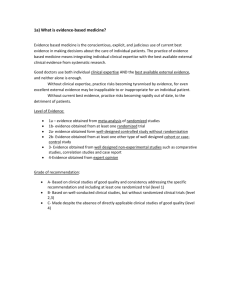
Turning Questions into Trials: Innovation in Surgical Oncology Jennifer E. Rosen MD FACS Assistant Professor of Surgery and Molecular Medicine Boston University School of Medicine Department of Surgery Instructional Innovation Conference March 2nd 2012 Clinical Trials in Surgical Oncology: Part of BUSM Third-Year Surgery Clerkship Core Lectures • Developed in 2006 to educate third-year medical students during their surgical rotation on clinical trials in surgical oncology • 30-35 medical students participate each rotation • Build a clinical trial in class from a problem that the students see on their surgical clinical rotation • in past, asked for written protocols in advance Clinical Trials in Surgical Oncology Objectives 1. Educate students about clinical trials in surgical oncology 2. Familiarize students with core concepts in clinical trials 3. Encourage students’ active learning when encountering problems in clinical care of patients with cancer 4. Introduce students to research ideas 5. Provide students with an opportunity to contemplate their future practice options…academics can be fun! 6. Assess the efficacy of an active-learning class 7. Elicit potential ideas for clinical trials!! Material and Issues Covered • What’s the evidence that supports our clinical practice? • What do you not understand in care or what don’t we do well – is it because you don’t know or because WE don’t know? • Titles for trials! And choosing the principal investigator • Inclusion and Exclusion criteria, compassionate use • Politics of trials • Funding for trials • Institutional Review Boards, ethical and safety issues • Trial design: Phase 0-IV, pre-registration, “Journal of Negative Results,” arms, standard of care, crossover, quality of life • Determination of sample size • Bias, randomization , conflict of interest and blinding • Patient perception of risks and benefits and the concept of informed consent • Outcomes and their measurement…. Knowledge Assessment /Evaluation: Pre- and post-test comparison (n=194) Pre correct Post correct P-value Conclusions? Question1: A Phase I Clinical Trial is designed to assess whether a drug will increase overall survival in patients with cancer. 94.2 99.5 0.002 Already knew this, but still improved Question2: An 85 year old woman has a median life expectancy of one to two more years. 47.6 90 <0.001 Poor knowledge pre lecture, improved Question3: Drug companies are required to report adverse events as they happen in clinical trials to the FDA 79.1 56.4 <0.001 Did worse with lecture! Question4: Informed consent is a legal document admissible in a court of law. 86.9 89.2 0.297 Already knew this, no change Question5: FDA approval is required in order for a drug to be used for patient treatment. 69.4 87.4 <0.001 Poor knowledge pre-lecture, improved Question6: In order to participate in a clinical trial, a patient needs to be seen at a center that offers the trial. 43.4 53.8 0.011 Poor knowledge prelecture, little change Question7: What proportion of cancer patients are enrolled in clinical trials in the United States? 65.1 99.4 <0.001 Fair knowledge prelecture, improved Clinical Trials in Surgical Oncology: Benefits Provides an interactive, first-hand perspective into how clinical trials work and where the ideas for clinical trials come from Enhances communication skills for developing a trial Humanizes the process of research Offers medical students the chance to understand the complexity of answering questions and improving care for patients with cancer Bridges clinical experience, book-based learning and a questioning mind with real-world examples of deficiencies in care (because these are real issues, shows students that these are challenges) Turn INFORMATION into KNOWLEDGE Examples of misconceptions Recognize the ways that context influences perception (example: socially accepted practices; patronage and corruption) Analyze situations to discern degrees of seriousness, potential consequences Recognize areas and reasons why people may disagree Engage in active learning early in the course Why I think it works • Based on their personal experience and confusion or dissatisfaction • Immediacy of engagement – requires no a priori knowledge, little preparation other than an engaged and questioning mind • Active elicitation of participation – if you don’t volunteer, you WILL be called upon • Group thinking but individual contribution • People like hearing what others say, and are curious…but also competitive! • Students discover the basic principles of clinical trials – and the basis for clinical practice – through active question and answer Using this innovation • Other clinical rotations • within Introduction to Clinical Medicine (first year course) • Within graduate medical education (residents, fellows) • Introduce social issues or controversial concepts Future modifications… • Introduce social issues or controversial concepts • Longitudinal follow-up • Return to prepared protocols