Causes of Secondary Amenorrhea
advertisement
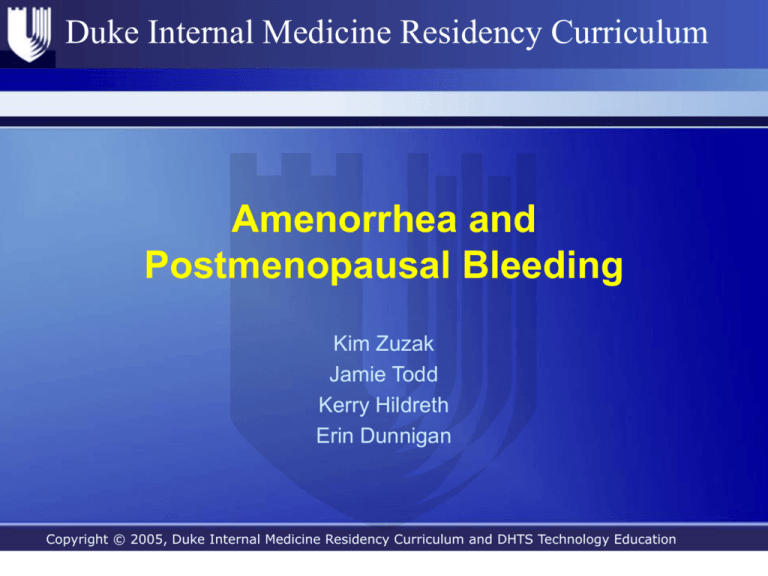
Duke Internal Medicine Residency Curriculum Amenorrhea and Postmenopausal Bleeding Kim Zuzak Jamie Todd Kerry Hildreth Erin Dunnigan Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Duke Internal Medicine Residency Curriculum Objectives • Amenorrhea – Definition and classification – Causes – Algorithm for approach to diagnosis, treatment • Postmenopausal bleeding – Definition – Causes – Approach to diagnosis Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #1 HPI: 32yo F history of HTN presents with absence of menses for 4 months. She is concerned that something is “terribly wrong”. Her cycles were previously normal and she has not been sexually active for several years. On further history and ROS she states she has felt quite jittery lately and feels that her concentration is impaired. She admits to slight weight loss. Meds: HCTZ 25mg po daily PE: T 37.0, BP 132/70, P 112 and regular Thin, but well nourished female who appears anxious and fidgety CV – tachycardic, but regular, no murmurs Pulmonary and abdominal exam unremarkable Neuro – normal with the exception of brisk DTRs Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #1Question The most likely cause of the patient’s amenorrhea is? A) Polycystic ovarian syndrome B) Hyperprolactinemia C) Hyperthyroidism D) Asherman’s syndrome E) Anxiety disorder Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #1 Answer The most likely cause of the patient’s amenorrhea is? A) Polycystic ovarian syndrome B) Hyperprolactinemia C) Hyperthyroidism D) Asherman’s syndrome E) Anxiety disorder Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Amenorrhea: Definitions and Classifications • Primary amenorrhea – No menarche by age 16 – Due to congenital or karyotype abnormalities – Uncommon, generally present to pediatricians • Secondary amenorrhea – Absence of menses for 3 months in setting of previously normal menstruation – Absence of menses for 9 months in setting of oligomenorrhea Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Secondary Amenorrhea • Pregnancy (most common) • Thyroid disease • Hyperprolactinemia • Normogonadotropic amenorrhea (outflow tract obstruction or hyperandrogenic anovulation) • Hypergonadotropic hypogonadism • Hypogonoadotropic hypogonadism Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Secondary Amenorrhea: Hyperprolactinemia • Prolactin <100mcg/L – – – – – Medications Breastfeeding or breast stimulation Substance abuse (cocaine, opiates) Altered metabolism (renal or liver failure) Ectopic production (renal cell or bronchogenic carcinoma, teratoma) • Prolactin >100mcg/L – Pituitary adenoma – Empty sella syndrome Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Secondary Amenorrhea: Normogonadotropic • Hyperandrogenic anovulation – – – – – – Polycystic ovarian syndrome Androgen secreting tumor Congenital adrenal hyperplasia Acromegaly Cushing’s disease Exogenous androgens • Outflow tract obstruction – Asherman’s syndrome • Intrauterine scarring from infection or curettage – Cervical stenosis Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Secondary Amenorrhea: Hypergonadotropic • Menopausal ovarian failure • Premature ovarian failure (increased FSH & LH) – – – – – – Autoimmune Chemotherapy Idiopathic Mumps Pelvic radiation Genetic Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Secondary Amenorrhea: Hypogonadotropic • • • • • • • • Anorexia or bulimia nervosa Excessive exercise Excessive weight loss Excessive psychosocial stressors Sheehan’s syndrome Chronic illness CNS tumor Cranial radiation Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Secondary Amenorrhea Secondary Amenorrhea, Negative betaHCG Check TSH and Prolactin Prolactin <100mcg/L Prolactin >100mcg/L Abnormal TSH Normal Prolactin Consider alternate causes of hyperprolactinemia MRI to evaluate for pituitary adenoma Thyroid disease Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Secondary Amenorrhea Secondary Amenorrhea, Negative betaHCG Check TSH and Prolactin Both Normal Progesterone challenge Withdrawal Bleed Normogonadotropic Hypogonadism No Withdrawal Bleed Estrogen/progesterone challenge Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Secondary Amenorrhea Estrogen/progesterone Challenge Withdrawal Bleed No Withdrawal Bleed Check FSH/LH FSH>20 and LH>40 Outflow Obstruction FSH and LH <5 Hypergonadotropic Hypogonadism MRI for pituitary adenoma If negative, then Hypogonadotropic Hypogonadism Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Estrogen/Progesterone Challenge • Use Medroxyprogesterone acetate (provera) for progesterone withdrawal bleed. 10mg po daily x 7-10 days. (other options include norethindrone, progesterone im, progesterone gel) • Use combined oral contraceptive for combined estrogen/progesterone challenge. Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #2 62yo F with a history of diabetes mellitus presents to her PCP with vaginal bleeding. She went through menopause at age 51 and has never been on HRT. She is now surprised to note that she has had intermittent spotting over the past month. It does not seem related to intercourse and she denies any trauma. Her last pap smear was 6 months ago and showed no atypia. Meds: Metformin, Lisinopril, ASA, Atorvastatin PE: T 37.0 BP 140/82 P 72 BMI 32.2 Pelvic with normal vaginal mucosa, no adenexal mass, cervix appears normal, no blood at the os Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #2 Question The most appropriate next step in diagnosing the etiology of this patient’s vaginal bleeding would be? A) Perform a cervical biopsy B) Proceed to hysteroscopy C) Check PTT and PT D) Proceed to transvaginal ultrasound E) Schedule an endometrial biopsy Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Case #2 Answer The most appropriate next step in diagnosing the etiology of this patient’s vaginal bleeding would be? A) Perform a cervical biopsy B) Proceed to hysteroscopy C) Check PTT and PT D) Proceed to transvaginal ultrasound E) Schedule an endometrial biopsy Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Postmenopausal Bleeding: Definitions • Postmenopausal bleeding – Patients not on HRT: • Any bleeding ≥ 12 months after last menses – Patients on HRT: • Any unexpected bleeding ≥ 12 months on HRT Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Postmenopausal Bleeding • • • • • Endometrial cancer Atrophy Endometrial hyperplasia Endometrial polyps Hormone effect • ~90-95% of cases are due to benign causes Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Causes of Postmenopausal Bleeding: Endometrial Cancer • Most common gyn cancer in women > 45 • ~5-10% of cases of postmenopausal bleeding • Risk factors – – – – – Nulliparity Age Diabetes mellitus Obesity Tamoxifen use Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum More Common Causes of Postmenopausal Bleeding • Atrophy is most common cause: ~ 40-60% of cases • Mechanism: Hypoestrogenism leads to endometrial/vaginal atrophy. This leads to a thin surface susceptible to bleeding. • Endometrial hyperplasia (~10%) – Caused by exposure to unopposed estrogen – Presence of atypia correlated with progression to endometrial cancer • Endometrial polyps (~12%) – Estrogen responsive – More common peri or early menopause • Hormone effect (~7%) – Pattern depends on regimen used Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Postmenopausal Bleeding • Transvaginal ultrasound – Endometrial thickness ≤ 5 mm • LR+ 2.8 (95% CI 1.66-4.55) • LR- 0.18 (95% CI .07-.46) – – – – Endometrial thickness > 5mm Increased echogenicity Persistent bleeding Inadequate visualization Endometrial Biopsy Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Postmenopausal Bleeding • Endometrial Biopsy – – – – Allows tissue sampling Simple procedure; no anesthesia Samples 5-15% of endometrial surface May miss small lesions Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Evaluation of Postmenopausal Bleeding • If TVUS and biopsy non-diagnostic: • Refer to Gynecologist – Saline infusion sonohysterography • TVUS after infusion of saline into endometrial cavity • Good for visualizing small lesions • No tissue obtained – Hysteroscopy • Direct visualization → directed biopsy • Good for small, focal lesions – MRI • Good for identifying fibroids, adenomyosis Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum Please click here to complete the course evaluation. Click Next arrow to continue to Reference pages. Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum References • • • • • Albers JR; Hull SK. Abnormal uterine bleeding. Am Fam Physician. 2004 Apr 15;69(8):1915-26. Goldstein RB; Bree RL; et al. Evaluation of the woman with postmenopausal bleeding: Society of Radiologists in UltrasoundSponsored Consensus Conference statement. J Ultrasound Med. 2001 Oct;20(10):1025-36. Review. Goodman A. Evaluation and management of uterine bleeding in postmenopausal women. UpToDate online 2006. Karlsson B; Granberg S; et al. Transvaginal ultrasonography of the endometrium in women with postmenopausal bleeding--a Nordic multicenter study. Am J Obstet Gynecol 1995 May;172(5):1488-94. Dijkhuizen FP; Brolmann HA; et al. The accuracy of transvaginal ultrasonography in the diagnosis of endometrial abnormalities. Obstet Gynecol 1996 Mar;87(3):345-9. Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services Duke Internal Medicine Residency Curriculum References • • • Martin, KA. The normal menstrual cycle. UptoDate. Mar 3 2004. Retrieved Sept 2 2006. http://www.utdol.com/utd/content/topic.do?topicKey=r_endo_f/2305&type =A&selectedTitle=1~60 Master-Hunter, T and Heiman, DL. Amenorrhea: evaluation and treatment. Am Fam Physician 2006;73:1374-82. Beckman, CRB et al. Obstetrics and Gynecology. Lippincott Williams and Wilkins. New York, NY. 2002. Copyright © 2005, Duke Internal Medicine Residency Curriculum and DHTS Technology Education Services