Extubation Criteria
advertisement
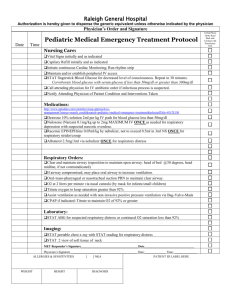
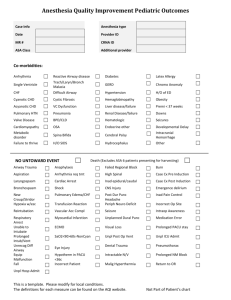
Extubation Criteria J. Prince Neelankavil, M.D. Case 71 y.o. male s/p laparascopic surgery presents to the PACU intubated. Pt. remained intubated secondary to residual neuromuscular blockade H/O HTN, DM When should we extubate? General Principles Why was the patient intubated in the first place? Inadequate oxygenation/ventilation/airway protection. Patient should have adequate respiratory drive, respiratory muscle strength, cough reflex to clear secretions, laryngeal function and clearance of sedative and neuromuscular blocking medications. Adequate Gas Exchange? Adequate arterial partial pressure of oxygen: [PaO2/FIO2] ratio > 150-200 Appropriate pH (pH >7.25) and arterial partial pressure of carbon dioxide during spontaneous ventilation Pass a Breathing Trial? 30–120 minute spontaneous breathing trial with low level of CPAP (e.g. 5 cm H2O) or low level of pressure support (e.g. 5-7 cm H2O) Show gas exchange (ABG), hemodynamic stability, and subjective comfort Pass These Numbers? RR < 35 Vital capacity > than 10 mL/kg NIF > -20 Tidal Volume > 5mL/kg Minute ventilation < 10L/min Thoracic compliance > 25 mL/cm H2O Able to Protect Airway? Appropriate level of consciousness Adequate airway protective reflexes (cough, swallow, vocal cord movement) Adequate managed secretions All Systems Go? Hemodynamic Stability (+/- 20%) Nutritional status allowing for respiratory muscle strength Risk Factors for Failed Extubation ICU patient Age > 70 or < 24 months Hemoglobin <10 mg/dL Longer duration of mechanical ventilation Medical or surgical airway condition Frequent pulmonary toilet Loss of airway protective reflexes What do you need to extubate? Oxygen source Suction Oral/Nasal airways Face masks Endotracheal tubes LMA Pulse ox Cardiac Monitors CO2 detectors Ambu bags What did we do before we extubated our patient? Ensured proper equipment needed for reintubation Monitoring BP, HR, Sat, RR Used a twitch monitor to demonstrate no fade on TOF/sustained tetany Turned off the propofol sedation What did we do before we extubated our patient? We did not quantitatively evaluate his tidal volume, thoracic compliance, pH, NIF, breathing trial, etc… We qualitatively evaluated several things 1. Stable hemodynamics 2. Able to protect airway 3. Able to exchange gases Stable Hemodynamics His preoperative BP and HR were 134/77 and 68 Prior to extubation his BP and HR were 126/72 and 61 Able to protect airway Patient was gagging on the ETT and would gag when we suctioned him Patient was coughing Able to exchange gases Patient was spontaneously breathing for 30 minutes Good ventilatory effort Maintained oxygen saturation Case Our patient was extubated and had an uneventful PACU stay. Another satisfied customer References American Association for Respiratory Care (AARC). Removal of the endotracheal tube--2007 revision & update. Respir Care 2007 Jan;52(1):81-93 Nir Hoftman, M.D.’s PACU extubation criteria