Journal review July 2007
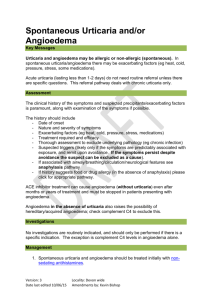
advertisement
Journal review July 2007 Heike Geduld QuickTime™ and a TIFF (LZW) decompressor are needed to see this picture. QuickTime™ and a TIFF (LZW) decompressor are needed to see this picture. Journal Clubs in South Africa • • • Highlight latest research Improve clinical practice Teach principles and practice of EBM Senior staff should have minimal core understanding of principles of research, epidemiology and biostatistics Evaluated 4 JC in Pretoria with Standard Questionnaire - relating to specific articles Mean scores = 42%, 28%, 25%, 15 % HOW WOULD WE SCORE? Recommend a clearly defined curriculum teaching critical appraisal skills, knowledge of basic epidemiology and biostatistics Risk tolerance for the exclusion of potentially life-threatening diseases in the ED American Journal of Emergency Medicine (2007) 25, 540–544 • • • • • • Objective: Given the same pretest probability (10%) for subarachnoid hemorrhage (SAH), pulmonarymembolism (PE), and acute coronary syndrome (ACS), we determined if differences exist in the risk tolerance for disease exclusion according to published guidelines given a negative test result. Methods: Published guidelines that make practice recommendations on the evaluation of ACS, PE, and SAH were sought using the National Guideline Clearinghouse in low-risk settings. Second-order Montem Carlo simulation was performed to determine point estimates and confidence intervals (CIs) for posttest probabilities assuming a pretest probability of 10%. Results: Guidelines recommend that patients with low-risk suspected ACS should undergo stress testing. For SAH, computed tomography (CT) followed by lumbar puncture (LP) is recommended without mention of pretest probability; and D-dimer testing is recommended to exclude PE in lowrisk patients. Test sensitivity for thallium-201 single photon emission computed tomography (SPECT) was 89%, exercise echocardiogram was 85%, D-dimer testing was 95%, and CT/LP for SAH was 100% (as a gold standard) and CT only was 97.5%. Given a negative test result, for PE, posttest probability was 0.5% (95% CI 0.1%-0.9%); for SPECT, 1.1% (SD 0.5%-1.6%); and for exercise echocardiogram, 1.5% (95% CI 0.5%-2.5%) compared with a posttest probability of 0% for CT followed by LP for SAH. Using a CT-only approach gives a posttest probability of 0.2% (95% CI 0.2%-0.4%). Conclusions: Guidelines for suspected PE and ACS allow small but nonzero calculated risk end points in low-risk settings, whereas SAH guidelines afford no misses. Because many gold standard tests are more invasive and can have adverse effects, guideline authors should consider adopting a standard acceptable miss rate as an end point for workups with low clinical suspicion to avoid the overuse of invasive testing. Risk Tolerance • • • • • PE, ACS and SAH all have 10% pretest probability Gold standard testing Pulmonary Angiography for PE, Cardiac Catheterisation for ACS CT Brain plus LP for SAH Risk Tolerance =nonzero post test probability; level of uncertainty after diagnostic testing that symptoms not due to disease • • • Guidelines - PE = risk stratification, D-dimer, V/Q scan, CTPA ACS = risk stratification,ECHO, SPECT SAH = CT brain + LP • • • • Table 1 Expected posttest probabilities given negative testing at a pretest probability of 10% Suspected disease/test Posttest probability (95% CI) SAH CT followed by LP 0% CT only 0.2% (0.0%-0.4%) ACS Exercise echocardiogram 1.5% (0.5%-2.5%) Thallium-201 SPECT 1.1% (0.5%-1.6%) PE D-Dimer 0.5% (0.1%-0.9%) Why are we willing to tolerate higher risks with ACS and PE? • • • • • • • • • • Frequency of presentation - familiarity breeds contempt Higher clinical gestalt Availability of Gold standard testing Invasiveness and risks of invasive testing Testing by ED staff only Unable to risk stratify with SAH Economic factors Patient risk tolerance for investigation Physician risk aversion Test specificity- what to do with false positives Problems - differences in sensitivity of CT with diff times and diff spectrum of SAH What is optimal risk tolerance for disease exclusion? What is standard acceptable miss rate? • Are Antibiotics Necessary After Incision and Drainage of a Cutaneous Abscess? • Annals of Emergency Medicine - Volume 50, Issue 1 (July 2007) Our review of the literature found 5 studies and 1 abstract, spanning a 30-year period, which address the issue of clinical outcomes of abscess incision and drainage with or without outpatient oral antibiotics. Of the 3 randomized trials, 1 lacked a placebo group and was not blinded to either the participants or the investigators; the 2 remaining studies, although double-blind placebocontrolled studies, used small study groups. None of the studies specifically addressed the issue of abscesses with overlying cellulitis. Therefore, our conclusions cannot be extrapolated to those cases in which there is a significant degree of overlying cellulitis. Although only 1 study excluded patients with significant comorbidities and immunocompromised conditions, none of the other studies specifically examined the impact of these comorbidities on clinical resolution. Finally, an abscess was not explicitly defined in any of the studies. Despite these limitations, each of the studies concluded that patients treated with incision and drainage alone exhibit resolution of their infection at the same rate as patients who are treated with incision and drainage plus antibiotic therapy. The data also demonstrate that both groups show a greater than or equal to 90% frequency of full resolution without complications. Even when the data from the most relevant and recent study are excluded because it is an abstract, the current literature does not support the routine practice of prescribing antibiotics after incision and drainage of simple cutaneous abscesses, even in high-MRSA-prevalence areas. A conclusive, multicenter, double-blind, randomized, placebo-controlled clinical trial is lacking and sorely needed. Antibiotics after Incision and Drainage • • • • • • • • 1. Cephalosporin given - decreased recurrence in small RCT 2. No difference in RCT 3. No difference in RCT 4. Prospective - <5cms, children, including MRSA, incl comorbidities 5. Large retrospective concordant vs discordant antibiotics, no difference in resolution Used clindamycin, different cephalosporins Most excluded immunocompromised pts Did not address issue of overlying cellulitis Management of haemodynamically stable patients with abdominal stab wounds Emergency Medicine Australasia (2007) 19, 269–275 Objectives: Australasian trauma centres receive relatively low numbers of penetrating injuries from stabbings. There is limited agreement regarding protocols to guide the management of haemodynamically stable patients with penetrating injuries. This has resulted in a wide variation in practice with anecdotally high negative laparotomy rates. The aim of the present study was to review the ED procedures, investigations and disposition of this group of patients. Methods: A retrospective review of all patients presenting with abdominal penetrating injury was undertaken over a 5 year period. Data on demographics, presenting features and management were collected. Results: There were 109 patients who were haemodynamically stable (systolic blood pressure > 90) on arrival to the trauma centre. Diagnostic ED procedures and investigations consisted of wound exploration in 47 (43.1%) patients, focused abdominal sonography in trauma in 44 (40.4%) patients and a CT abdomen in 36 (33.0%) of patients. The sensitivity for focused abdominal sonography in trauma and CT when used together was 77.8%. There were 39 laparotomies performed with a negative laparotomy rate of 23.1%. There were 10 laparoscopies performed, none went on to require a laparotomy. Patients undergoing negative laparotomies spent significantly longer times in hospital than patients managed conservatively or those undergoing laparoscopies. Conclusions: The number of penetrating abdominal injuries remains low. Imaging alone cannot reliably exclude intraperitoneal injury. A greater utilization of ED wound exploration and laparoscopy based on agreed guidelines could improve management. An algorithm for the management of these patients is suggested. Stable Abdominal stabs • • 109 pts over 5 years - ? Major trauma centre Stable - SBP> 90mmHg • Wound exploration = 47 (36 repaired in ED, 2 + laps, 2 - laps, 3 lap scopes, 4 conservative Mx after CT) • No wound exploration = 62 (34 laps 6-) • Wound exploration techniques techniques described in J of E. medicine 1985 • • • • In SA - high incidence few adjunctive tests laparotomy vs lap scope Need for further studies Do Children Require ECG Evaluation and Inpatient Telemetry After Household Electrical Exposures? • [Ann Emerg Med. 2007;49:64-67.] 7 studies –all retrospective reviews 5-164 pts (less than 21 yrs) • THE BOTTOM LINE • Healthy children exposed to common household currents • (120 to 240 V, no water contact), if asymptomatic at ED • presentation and without a ventricular arrhythmia or cardiac • arrest in the field, are at very low risk for developing cardiac • arrhythmias. Patients with a normal initial ECG result do not • develop late dysrhythmias, and those with nonfatal arrhythmias • or nonspecific ECG abnormalities typically resolve • spontaneously within 24 hours. Therefore, this review of • available literature supports the practice of safely discharging • these children without an initial ECG evaluation or inpatient • cardiac monitoring after a common household current exposure. • Our recommendations do not pertain to patients who might • require admission for other injuries. • The value of serum tau protein for the diagnosis of intracranial injury in minor head trauma American Journal of Emergency Medicine (2007) 25, 391–395 Abstract Objective: Tau protein localizes in the axons of neuron cells, and it is released secondarily from the central nervous system because of hypoxia and trauma. In the present study, it was aimed to investigate the value of serum tau protein levels in diagnosing intracranial pathologies in minor head trauma. Methods: Patients were categorized into 2 groups: those without intracranial lesions in head CTs (group1) and those with lesions in head CTs (group 2). Serum tau protein levels were determined. Results: Group 1 (n = 55) median serum tau protein level was 16.29 pg/mL (2.12-215.97 pg/mL) and group 2 (n = 33) median serum tau protein level was 18.39 pg/mL (2.19-714.47 pg/mL). Statistical analysis revealed no significant difference between the 2 groups for tau protein values, sex, age, mechanism of trauma, and Glasgow Coma Scale score. Conclusion: It is suggested that serum tau protein has limited value in minor head trauma. • Angiotensin II Receptor Blocker-Associated Angioedema: On the Heels of ACE Inhibitor Angioedema Abstract Angioedema and cough are known side effects of angiotensin-converting enzyme (ACE) inhibitors. Angiotensin-converting enzyme is a potent inhibitor of kinase II, which facilitates the breakdown of bradykinin. An increase in bradykinin levels results in continued prostaglandin E2 synthesis, vasodilation, increased vascular permeability, and increased interstitial fluid. In contrast, the angiotensin II receptor blockers (ARBs) do not increase bradykinin levels. Angioedema as a complication of ACE inhibitor therapy is not widely recognized; this complication is even less recognized with second-line ARBs. We report angioedema associated with losartan (an ARB) in a patient who had experienced angioedema secondary to enalapril (an ACE inhibitor). Almost half of patients with ARBassociated angioedema also had developed angioedema while receiving ACE inhibitor therapy. Clinicians should exercise caution when using ARBs in patients with a history of angioedema secondary to ACE inhibitors. ARBs and Angiodema Can angiotensin receptor antagonists be used safely in patients with previous ACE inhibitor-induced angioedema? Drug Saf. 2002;25(2):73-6 Angioedema is an uncommon but potentially life-threatening adverse event associated with ACE inhibitor therapy which is believed to be due to potentiation of the vascular effects of bradykinin. Angiotensin receptor antagonists were not expected to produce angioedema, as they do not inhibit the catabolism of bradykinin. However, it is now apparent that angioedema is occasionally associated with angiotensin receptor antagonist therapy and may be more likely to occur in patients who have previously experienced angioedema while receiving ACE inhibitors. Angiotensin receptor antagonists cannot be considered to be a safe alternative therapy in patients who have previously experienced ACE inhibitor-associated angioedema. [Ann Emerg Med. 2007;49:717.] A 19-year-old unrestrained male driver was being pursued by police and struck a telephone pole at a high rate of speed. A 20-minute foot chase ensued. Once apprehended, he complained of back pain, was pale, was diaphoretic, and had 1 episode of bloody emesis. On physical examination, he had a respiratory rate of 16 breaths/min, pulse rate of 86 beats/min, blood pressure of 134/76, and oxygen saturation of 98% on a nonrebreather facemask. He was uncooperative and agitated and complained only of back pain. On auscultation of his chest, his breath sounds were clear bilaterally. He had midthoracic spine tenderness and diffuse abdominal tenderness to palpation. A supine chest radiograph (Figure 1) was performed • IMAGES IN EMERGENCY MEDICINE • DIAGNOSIS: • Deep sulcus sign. First described by Gordon, the deep sulcus sign may be the only evidence of a pneumothorax on a supine chest radiograph. A deepening of the costophrenic angle occurs when air tracks anteriorly and caudally along the pleural space when the patient is lying supine. • The arrows in Figure 2 highlight the hyperlucent area that is shown as an anterior pneumothorax, which is revealed in Figure 3, the computed tomography scan of the chest obtained immediately after the chest radiograph. • Figure 4 shows that the findings resolved after placement • of the chest tube. • False-positive examples of the deep sulcus sign have been described in patients with chronic obstructive pulmonary disease and those receiving mechanical ventilation with high tidal volumes. • • • • REFERENCES 1. Gorden R. The deep sulcus sign. Radiology. 1980;136:25-27. 2. Kong A. The deep sulcus sign. Radiology. 2003;228:415-416. 3. Tocino I, Armstrong JD. Trauma to the lung. In: Imaging of Diseases of the Chest. St. Louis, MO: Mosby; 2000:770-771. THE END