1. dia
advertisement
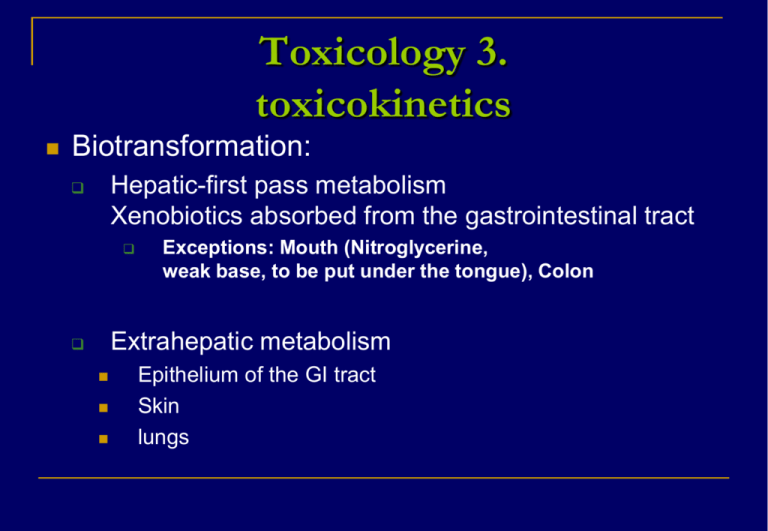
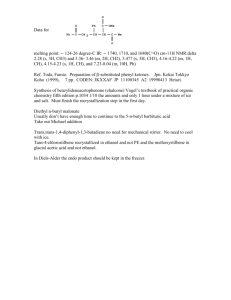
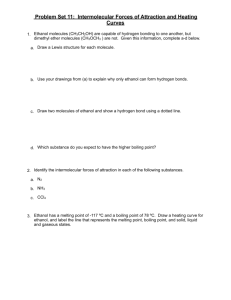
Toxicology 3. toxicokinetics Biotransformation: Hepatic-first pass metabolism Xenobiotics absorbed from the gastrointestinal tract Exceptions: Mouth (Nitroglycerine, weak base, to be put under the tongue), Colon Extrahepatic metabolism Epithelium of the GI tract Skin lungs bioavailability Ratio of the dose reaching the systemic circulation (0-1) Bioavailability depends on oral absorption and the first pass metabolism. Concentration of the molecule in the blood after oral administration/ Concentration of the molecule in the blood after intravenous administration Distribution: Binding to plasma proteins Plasma protein binding: helps the distribution of a xenobiotic and prevents its excretion Reversible/irreversible affinity, Kd= concentration of free xenobiotic x concentration of free binding site/ concentration of occupied binding sites Species differences in binding to plasma proteins Thyroxine is binding to plasma proteins in humans. 2/3 of thyroxine molecules are present in the form of thyroglobulin, the remaining molecules bind to albumins or prealbumins. In rats thyroxine is dissolved in the blood without binding to proteins. Some xenobiotics induce metabolic enzymes and accelerate the elimination of thyroxine. In rats: as the level of thyroxine is reduced, the thyroid gland tries to produce more thyroxine by cell proliferation. This can lead to tumours in the thyroid. In humans: the same xenobiotic will not cause thyroid tumours, because of the protein binding of the thyroxine. Elimination Exretion Biotransformation Ecretion via urine Excretion via the bile Excretion via the lungs Ecretion with mother’s milk, placenta, hair, saliva, tears…etc, Ultra-filtration, passive reabsorption, active tubular secretion Nefron Table: Molecular mass and the route of some biphenyls in rats Route of excretion(%) compound Molecular mass kidney Faeces Biphenyl 154 80 20 4-monochloro-biphenyl 188 50 50 4,4’-dichloro-biphenyl 223 34 66 2,4,5,2’,5’-pentachloro-biphenyl 326 11 89 2,3,6,2’,3’,6’-hexachloro-biphenyl 361 1 99 Reference: H. B. Mattheus in: Introduction to Biochemical Toxicology (1960) Enterohepatic circulation Effects depend on Dose Time period of dosing Other molecules present (induction, inhibitionj) Graded response- measured on a continouos scale Quantal response –measured by counting responders in a group Receptor types Intracellular receptors Cell surface receptors Receptors with enzyme activity Receptors leading to a chain of reactions Receptors triggering a secondary messenger Ion chanels Intracellular receptor Tyrosine kinase: a transmembrane receptor having enzyme activity Receptor with enzyme activity triggering a chain reaction G-protein coupled receptor Ion chanel receptor Toxicodynamics Ethanol Absorption: passive diffusion from the whole length of the GI tract Pow= 0,4898 (logPow= -0,31) Metabolism of ethanol Ethanol Acetaldehyde Alcohol dehydrogenase (SER, MFO) Aldehyde dehydrogenase (2 isoforms, in cytosol or mitochondria) Acetic acid ACSS2 enzyme (Acetyl-coenzymeA synthetase S2, cytosol) Acetyl-coenzyme A Enzymes of the citrate cycle 3 H2O + 2 CO2 Energy : approximately 1300 kJ/mol Elimination of ethanol and its metabolites Ethanol: urine, exhalation, sweat Acetic acid- urine Acetyl-coenzyme A- used for biosynthetic processes, biotransformation, like acetilation or as an energy source in the citrate cycle The elimination rate of ethanol Rate limiting step: oxydation to acetaldehyde Reaction of 0 grade (KM: 80 mg/l, but much higher plasma concentration is frequent) Elimination rate: 10 g ethanol/hour, the elimination of ½ l wine takes 7 hours Acute effects of ethanol g/l For later effects (hangover, intoxication effects) mainly the acetaldehyde is responsible and the free radicals it generates. Free radicals cause oxidative stress and cell death. Two forms of aldehyde dehydrogenase are present in the cytosol or in mitochondria In the white population both forms are active while in 50% of Asiatic people the mitochondial enzyme is missing or has a very low activity. Effects of chronic ethanol exposure free radicals –cell damage Liver –is the main target organ Chronic hepatitis Fatty liver (5%-50% lipid content ) Livercirrhosis Liver tumours Further chronic effects Pancreas Heart Pacreatitis Tumours The performance of the heart is reduced (Chronic cardiomyopathy) Nervous system Tremors, impairment of the sight and the memory willpower, impaired judgment, emotional lability, outbursts of anger… Effects on the development Low birth weight Small head circumference nervous system disorders abnormalities of the hippocampus: learning difficulties Small cerebellum: motion developmental disorders Small corpus callosum, hyperactivity, impulsive behavior Some characteristics of the fetal alcohol syndrome Dose dependent fetal effects: Strong drinking: teratogenic effects Moderate drinking:neurotoxic effects (fetal NOAEL can not be established) Summary of the chronic effects of ethanol Toxic for several organs Carcinogenic (I.A.R.C. Cat1A, ) Neurotoxic Teratogenic Causes of carcinogenesis Physical (ionizing radiation) Chemical (genotoxic and non-genotoxic carcinogens) Biological (viruses, bacteria, endoparasitic insects, etc.) Steps of chemical carcinogenesis Step 1 Initiation Highly electrophilic structures, free radicals, organic cations bind covalently to special nucleophilic binding sites of the DNA and form DNA-adducts (some critical sites: Guanine C8, N2, N3, O6, Timidine, Uracil O2, O4, N3 position). Step 2 Fixation : If repair enzymes cut off the altered parts, then DNA polymerase synthetizes the missing part on the basis of the complementer strand ---the cell remains normal If the mutation takes place in an inactive part of the DNA, this does not change the functions-the-cell remains normal The mutation damages seriously the functions of the cell ---the cell dies, the organism remains healthy if the altered cell survives and divides-the mutation can be fixed. Capacity of DNA repair in some organs Liver: good Kidney: intermediate Brain: practically missing Step 3 Promotion: selective increase of the iniciated cells helped by a repeated effect of a promoter within a critical period of time Not a genetic effect The result is a microscopic neoplasia The promoter effect is dose dependent but there is a limit dose Some promoters Mitogens: substances stimulating cell proliferation (endogenous mitogens, like estrogens or other hormones or exogenous mitogens.) Permanent presence of cytotoxic substances Persisting mechanical effects (irritation) causing cytotoxicity Blood loss in rats is promoting leukemia Inhibition of the carcinogenic process Inhibition of cell division Immune system (macrophags, limphokins) Reduced total energy intake Specific dietary components: Vitamines A, C and E Step 4 Progression For further increase of iniciated cells— often a new mutation is needed. New initiated cell types have to appear which produce angiogenesis factor, helping vascularisation of the microtumour Blood vessels develop in the harmless microtumour ( max.0,5 mm3) and the small tumour starts to grow at an exponential rate. Step 5 Metastases The tumour becomes invasive, the cancer cells disseminate through blood and lymph vessels and new, secunder tumours develop at different parts of the body. Tumour therapy Surgical therapy Radiotherapy Drug therapy Komplex therapy Types of anti-cancer drugs Drugs inhibiting DNA duplication Antimetabolites (Enzyme inhibitors, nucleic acid synthesis inhibitors: methotrexate, antifolates, pirimidin antagonists, dezoxycyitidine analogs, purine antagonists DNA alkylating agents :cyclophosphamide (they prevent cell proliferation, but might have serious effects): Topoizomerase I és II inhibitors ( they inhibit the integration of DNA chains) Agents that affect the regulation of cell proliferation Mitotic spindle inhibitors: Vinca alkaloids, taxanes, vinblastine, vinchristine, taxol, taxotere (inhibiting the development of the mitotic spindle) Hormones and hormone-like compounds, like progesterones, anti-estrogens, aromatase inhibitors, antiandrogens, which inhibit the growth of hormone dependent tumours. Cytokins (interferons, interleukins): inhance the immune response of the host Tyrosine kinase inhibitors: they reduce the viability of tumour cells by inhibiting signal transduction Monoclonal antibodies: they inactivate cell surface receptors 3 Drugs inhibiting vascularisation Avastine, thalidomide Anti-metastasis agents Bisphosphanates: prevent stone metastasis from breast and prostate tumours. Drugs to improve the quality of life of the patient Filgrastine. Enhances the production of white blood cells Erithropoetine alpha: helps the proliferation of erithrocytes Mesna, Amifostine: neutralise the reactive groups of drugs in the healthy tissues. Literature recommended Niesink et al: Toxicology, Principles and applications (1996.) CRC Press, LLC and Open University of the Netherlands ISBN: 0-8493-9232-2 Gyires Klára, Fürst Zsuzsanna: Farmakológia (2007.) Medicina Könyvkiadó Rt., Budapest ISBN: 978 963 226 137 9 (I kötet)