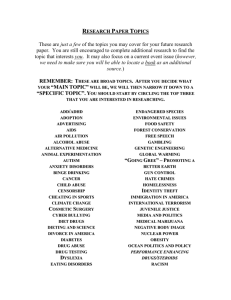
Substance Abuse PPT
advertisement
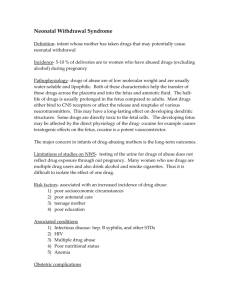
Substance Abuse Disorders Chapter 25 Terms • Use – drinking alcohol, swallows, smokes, sniffs, or injects • Abuse – use for purposes of intoxication or for Rx beyond intended use • Dependence – use despite adverse consequences • Addiction – psychological and behavioral dependence Terms • Withdrawal – Adverse physical and psychological symptoms that occur when stop using. • Detoxification – Process of safely and effectively withdrawing a person from an addictive substance. • Relapse – Recurrence of alcohol- or drug- dependent behavior who had previously been abstinent. DSM-IV Substance Abuse Disorders • alcohol • amphetamines • cannabis (marijuana) • cocaine • hallucinogens • inhalants • nicotine • opioids • phencyclidine • sedativehypnotics • anxiolytics • caffeine DSM-IV Categories – Abuse of a substance – Dependence upon a substance – Induced by intoxication or withdrawal – Table 25.1 Epidemiology: Lifetime Prevalence • Positive lifetime history of heavy alcohol use – 23.4% of US adults • Positive lifetime history for drug use – 15.6% of US adults Epidemiology • African American – lower rates of both licit and illicit substances compared to whites – experience more health and legal problems than other groups – alcohol-related consequences for males is higher than whites • Latino Americans – high use of drug among adolescents (HS students have highest rates of crack-cocaine and heroin use – Differences in prevalence among different groups (Mexican Americans - highest; Cuban Americans - lowest) Epidemiology • Asian and Pacific • data are limited • • • • drunkenness is disgraceful drinking is a male activity seeking help is a sign of weakness Asian “flushing syndrome” • Native Americans • rates among the highest • alcohol plays a in health problems of this group Epidemiology Gender Issues • Incidence rates of substance abuse and dependence – 1.7% per year men – 0.7% per year women • Males - more likely to abuse drugs and alcohol • Women - more likely to abuse prescription drugs • High number of substance abusers have comorbid mental disorders Etiology Biologic – Genetic Influence • Clear evidence that it runs in families • Controversy about specific gene (allele of D2) – Neurobiologic • Through the reward system -- medial forebrain bundle (MFB)-related to cravings • Intoxication increases extracellular dopamine Etiology: Psychological Theories Addictive Personality – – – – – need to feel self-worth need to have control over the environment need to feel intimate contact need to accomplish something need to eliminate pain or negative feelings Behavioral Theories – conduct problems of childhood – relationship between conduct problems, hyperactivity, impulsivity, and future substance abuse Etiology: Social Theories • Peer drug use and affiliation • Poor interaction skills • Certain neighborhood characteristics Alcohol • 90% of Americans have had a drink at some point in their lives • 16% have alcoholism • Body can metabolize 1 oz of liquor per hour - 5 oz glass of wine, 12 oz can of beer (Table 25.4) • Excessive use can adversely affect all body systems (Table 25.5) • Cerebellar degeneration from increased levels of acetaldehyde (byproduct of alcohol metabolism) -- impaired coordination, unsteady gait, fine tremors • REM and chronic sleep disorders • Drinking patterns vary Biologic Response to ETOH • Membranes permeable to K+ and Cl-, and closes Na+ & Ca++ channels depression of CNS, adrenergic activity BP and HR • Acetaldehyde is a by-product of alcohol metabolism. Large amounts of acetaldehyde combine with dopamine and serotonin to produce a substance that is highly addictive Response to ETOH: Alcohol Tolerance • Rapid metabolism and sedation, motor, and anxiolytic effects • Higher levels of BAL before intoxication • Locus ceruleus -- inhibits action of ethanol and instrumental in tolerance • During withdrawal, locus ceruleus is hyperactive noradrenergic activity and CNS stimulation Alcohol Withdrawal Syndrome • Changes in VS – BP and HR • Diaphoresis • Adverse GI effects • CNS side effects – – – – – – anxiety restlessness hand tremors or “shakes” disorientation confusion delirium tremens (DTs) Delirium Tremens • • • • • • • • • • • 10 or more years of drinking Tachycardia Sweating Hypertension Irregular tremor Searing Hypertension Tremor Delusions Vivid hallucinations Resolves in 3-4 days Alcohol-Induced Amnestic Disorders • History of many years of drinking • Over age of 40 • Onset -- sudden or insidious Alcohol-Induced Amnestic Disorders: Wernicke’s Syndrome • Reversible, caused by diet deficiency of thiamine • Marked diplopia (palsy of the 3 and 4 cranial nerves), hyperactivity and delirium (cortical brain and thalamic lesions), coma Alcohol-Induced Amnestic Disorders Korsakoff’s Psychosis • Follows Wernicke’s enceophalopathy • Loss of recent memory and confabulation • Vulnerable to others Psychopharmacology Acute Symptoms of Withdrawal • Benzodiazepines to produce sedation and reduce anxiety symptoms • Diazepam 5-10 mg every 2-4 hours • Librium 25-100 mg every 4 hours Pharmacology & Nutrition • Disulfiram (Antabuse) – Agonist – Inhibits ALDH metabolism and causes nausea and hypotension, severe can cause death – Occurs 10-20 minutes after ingestion – Adjunct treatment • Naltrexone (Trexan) – Narcotic antagonist – Reduces cravings for alcohol • Nutrition and vitamins Cocaine • 1.5 million Americans use cocain • Men have a higher rate than women • Stimulant -- made from leaves of coca plant • Sudden burst of alertness, energy, and selfconfidence • High lasts 10-20 minutes, then let down • Crack cocaine -- street drug form, highly addictive Biologic Effects of Cocaine • Increases the release and blockage of the reuptake of norepinephrine, serotonin and dopamine • Dopamine -- euphoria and psychotic symptoms (prolactin levels-contributes to sexual dysfunction and secondary sexual characteristics) • Norepinephrine -- tachycardia, hypertension, dilated pupils, and body temp • Serotonin -- sleep disturbances, anorexia • Long term use -- depletion of dopamine Cocaine • Intoxication – CNS stimulation followed by depression – Increasing doses -- restlessness tremors and agitation convulsions CNS depression – Death -- respiratory failure • Withdrawal – Norepinephrine depletion causes person to sleep 12-18 hours – Then, sleep disturbances with rebound REM, anergia, decreased libido, depression, suicidality, anhedonia, poor concentration and cocaine craving Treatment of Cocaine Craving • Antidepressants • Anticonvulsants • Dopamine agonists Others • Amphetamines -- Stimulant – block reuptake of norepinephrine and dopamine, not as strong effect on serotonin (as cocaine does) – Effect peripheral nervous system • Cannabis -- Relaxant – Stored in fat tissue for weeks – Amotivational syndrome • Hallucinogens -- LSD – Phencyclidine (PCP) angel dust – awareness and detachment – hallucinations/destructive behavior (adrenergic ) Opiates -- Narcotics • Any substance that binds to the opioid receptor • Cause CNS depression, sleep or stupor, and analgesia • Major -- heroin, codeine, and meperidine • Act on Delta and Mu receptors and depress the CNA • Types – agonist -- increases CNS effects – antagonist -- block CNS effects – mixed agonist-antoagonist • Effects of opiates – pleasure – relief of pain • Cause tolerance and physical dependence Opiate Treatment • Antagonist -- block CNS effects, Naloxone (Narcan) • Detox -- gradual reduction over several days • Methadone maintenance treatment – Opiate that satisfies craving, but no subjective high (See Table 25.7) • Naltrexone -- see Drug Profile Other Substances • Sedatives-Hypnotics and Anxiolytics – Abuse of prescription drugs – See Table 25.8 • Inhalants – Cause euphoria, sedation, emotional lability, impaired judgment – Result in respiratory depression – Found in common household products • Nicotine • Caffeine Nursing Management Assessment • Denial • Countertransference (Table 25.11) • Codependence (Figure 25.2) – Maladaptive learned pattern of coping – Roles in family • • • • • • Chief enabler Dependent Hero Scapegoat Lost child Mascot Nursing Diagnoses • • • • Risk for Injury Disturbed Thought Processes Anxiety Risk for Ineffective Management of Therapeutic Regimen, Ineffective Denial • Altered Nutrition Motivation for Change • Key predictor of whether an individual will change their substance abuse • Involves recognizing problem, searching for a way to change, and then changing • Motivational interviewing seeks to elicit selfmotivational statement from patients, supports behavioral change, and creates a discrepancy between the patient’s goals and continued alcohol and other drug use. Guidelines for Therapeutic Relationship • Encourage honest expression of feelings • Listen and express caring • Hold individual responsible for behavior • Provide consequences for negative behavior and talk about specific, objectionable actions • Do not compromise own values, monitor reaction • Communicate to team Reality Confrontation • Therapeutic strategy that promotes the person’s experience of the natural consequences of one’s behavior. • Learning from previous behavior • Guidelines for establishing interactions (See Table 25.10 and Therapeutic Dialogue) Special Considerations • HIV and substance abuse – high risk for HIV among IV drug users – dual diagnosis of chemical dependency and HIV requires extremely careful assessment, intervention – patients often experience intense feelings of uselessness • Harm-reduction strategies – community health intervention replacing moral and criminal approach -- needle exchange programs, designated driver Special Considerations (cont) Pregnancy and substance abuse • Detrimental effects on pregnancy • Several clinical issues facing mothers • • • • • • • • feelings of guilt and shame difficulties being a single parent care and responsibility of raising children early sobriety lack of access to treatment facilities anger and blame from caregivers need for parenting skills potential for child abuse and neglect lack of medical and other health care services Interventions • • • • • • • 12-step program (Table 25.13) Cognitive therapy Psychoeducation groups Behavioral interventions Group therapy and early recovery Individual therapy Family therapy Interventions • Nursing Care Plan 25.1 • Depend upon the stage of treatment