Cystic Fibrosis
advertisement

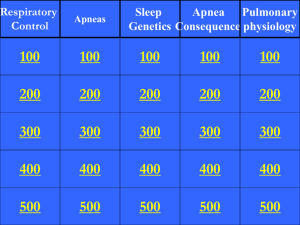
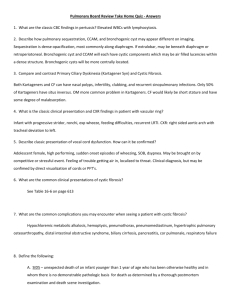
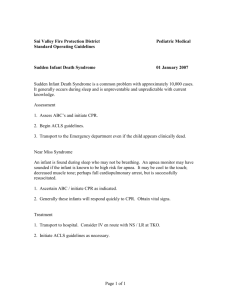
What are the odds of a healthy sibling of someone with CF being a carrier? A. 1/2 B. 2/3 C. 1/3 D. 3/4 Most common life-shortening genetic disease among white North americans • 1/3300 • Carrier 1/30 African Americans • 1/17,000 Asian • 1/35,000-50,000 AR CF gene • CFTR – epithelial chloride channel • Abnormally viscid and poorly hydrated secretions Most common • Delta-F508 mutation Median age of survival • 35.1y Exocrinopathy • Inspissation of abnormally thick secretions Lungs Pancreas Lungs • Impaired airway clearance • Retention of bacteria Chronic infection Chronic inflammation • Gradual decline in function • Accounts for majority of deaths Pancreas • Obstruction of ducts Dietary fat and protein not broken down Autodigestion Scar tissue Exocrine deficiency • 40-50% of newborns with CF • Hypoproteinemia • Fat soluble vitamin deficiencies Meconium ileus • 5-10% • Intestinal obstruction of the newborn Distention Bilious vomiting Failure to pass meconium • Xray Dilated loops Ground glass or soap bubble Meconium Ileus • Barium or water-soluble contrast enema Small distal colon • Prenatal rupture Abdominal calcifications Poor weight gain Loose, foul-smelling bulky stools Voracious appetite Rectal prolapse • 5% Chronic productive cough Chronic wheezing Digital clubbing Recurrent PNA Recurrent sinus disease Nasal polyps • 20% Persistent symptoms • Loose, productive cough May have blood-tinged sputum May signify acute infection • Tachypnea • Dyspnea • Diffuse crackles • Digital clubbing • Barrel chest A patient with known CF presents to the ER with the complaint of acute onset of chest pain and shortness of breath. CXR is pictured. What is the diagnosis? A. Pneumonia B. Pneumomediastinum C. Pneumothorax D. Bronchiectasis E. Cor pulmonale Hypochloremic metabolic alkalosis Hemoptysis Pneumothorax Pneumomediastinum Hypertrophic pulmonary osteoarthopathy Distal intestinal obstructive syndrome Biliary cirrhosis Pancreatitis Cor pulmonale Respiratory failure NBS • Elevation of serum trypsinogen Sweat Test • Gold standard • >60 mEq/L • 40-60 mEq/L Repeat Genetic Testing Acute • Aminoglycoside and a PCN derivative that attacks pseudomonas • At CHNOLA Ceftaz Timentin + Tobramycin Timentin + Gentamicin • Consider aerosolized Abx Chronic • Enzymes • ADEK • Treatments Bronchodilators Pulmozyme • Aggressive vibratory CPT You are counseling a new mom in the hospital before she brings her healthy, term newborn baby home. The mother asks about the benefit of using an over-the-counter apnea monitor that she saw at Babies-R-Us. What do you tell her? A. A home apnea monitor is of no value in preventing SIDS B. You highly suggest it, since home apnea monitors have been proven to prevent SIDS C. The best thing she can do for her baby is to lay the infant prone while sleeping D. She is worrying over nothing, her baby is not at risk for SIDS Definition • Unexpected death • <1y • Otherwise healthy • Negative autopsy 0.2/1000 live births Leading cause of death after neonatal period Peak at 2-4 months Rare after 6 months Cause • Final common pathway Long-QT IEM Smothering • Apnea hypothesis discarded Home apnea monitor is of no value in preventing SIDS • True cause unknown Risk Factors • Parental smoking • Prone sleep position • Overheated room • Co-sleeping • Low income families • Cold weather • Young parents Prevention • Back to sleep • Parental smoking outside the home and not in the car Definition • Witnessed event • Frightening to observer • Combination of . . Apnea Color change Change in tone Choking or gagging • Intervention Peaks at 2-3 months • Risk reduced after 6 months Causes • GER Single most common cause • Sepsis/Meningitis • IEM • Seizure • Pertussis • RSV • CHD • Poisoning • Child abuse Work Up • ECG • Lytes • Glucose • Ammonia • Blood culture • CBC • Blood gas • Tox • Head CT • Sleep study • pH probe A one month old infant with Pierre-Robin sequence has arrived to your clinic for follow up after discharge from the NICU 1 week ago. The mother is concerned because although the apnea monitor has not gone off, he does not appear to be getting any air in on some of his breaths while asleep. What do you tell the mother? A. If the apnea monitor has not gone off, there is no apnea and she should not worry. B. He most likely has central apnea. C. He most likely has obstructive apnea. D. He should be emergently evaluated for pulmonary HTN Definition • Absence of airflow ≥20 secs OR • Apnea associated with cyanosis or bradycardia Periodic Breathing • Recurrent brief pauses <20 sec • May be brief drop in HR but no bradycardia Types • Central • Obstructive Most common • Mixed NORMAL UPPER AIRWAY ANATOMY Obesity GER Sickle cell anemia Laxity of the supraglottic structures Marked adenoidal or tonsillar enlargement ABNORMAL UPPER AIRWAY ANATOMY Crouzon syndrome Apert syndrome Down syndrome Treacher Collins syndrome Pierre Robin sequence Arnold-Chiari malformation Prader-Willi Mobius syndrome Dwarfism Symptoms • FTT • Hyperactivity Diagnosis • Sleep study Further Work Up • Pulmonary HTN Cardiac Echo ECG Management • Apnea monitor Will not help since chest wall moves • Correct underlying disorder • CPAP Risk Factors • Seizure disorders • CNS pathology Arnold-Chiari IVH • Prematurity • Congenital Hypoventilation Syndrome Ondine’s curse Work Up • Responses to hypercapnia or hypoxia • CXR • EEG • Head CT • pH probe • Bronchoscopy Causes • Incoordination of swallowing • GER • More common in patients with neurologic impairment Complications • Mixed restrictive- obstructive pulmonary disease • Difficult to control asthma Suspect • Poorly controlled asthma despite aggressive management Risks • Delayed gastric emptying • GER • Achalasia Diagnosis • Modified barium swallow Thin vs paste vs solid Phases of the swallowing cycle • Salivagram Tube fed individuals Diagnosis • Gastric emptying scan Reflux (insensitive) Delayed gastric emptying • Bronchoscopy with BAL Lipid-laden macrophages Inspection ≥ 6 years Account for • Variability in • • • • • performance Age Height Weight Sex Race Use • Establishing severity • Guiding choice of therapy • Measuring response to therapy You are seeing a patient in the ER who is in moderate respiratory distress. You strongly suspect there is an aspirated foreign body based on your physical exam and some preliminary studies. Who do you call?? A. B. C. D. Pulmonary for flexible bronchoscopy Surgery for open removal Surgery for rigid bronchoscopy No one, you should do a blind finger sweep Indicated • Stridor • Unexplained or chronic cough or wheeze • Suspected airway malformations or compression • Atelectasis • PNA Isolating organisms Contraindicated • Foreign body Better visualization of distal airways and upper lobes NOCTURNAL POLYSOMNOGRAPHY Sleep stage Movement of chest Abdomen Electromyogram of diaphragm Arterial saturation Heart rate End-tidal CO2 Eye movements PNEUMOGRAM Chest wall movement Air flow by nasal thermistor Heart rate Arterial saturation Central apnea and bradycardia Limitations (Reasons to order Co-Oximetry) • Carboxyhemoglobin Carbon monoxide Pulse ox will overestimate the level of oxyhemoglobin • Methemoglobin Inconsistent and unreliable values Non-cardiac cause of cyanosis “chocolate” colored blood • Impaired perfusion