Screening and Assessment Nutrition 527
advertisement
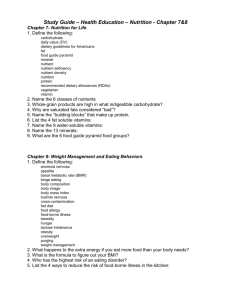
Nutrition Screening and Assessment Nutrition 526: 2010 Steps to Evaluating Pediatric Nutrition Problems • Screening • Assessment – Data collection – Evaluation and interpretation – Intervention – Monitor – reassessment Nutrition Screening: Purpose • To identify individuals who appear to have or be at risk for nutrition problems • To identify individuals who require further assessment or evaluation Screening: Definition • Process of identifying characteristics known to be associated with nutrition problems – ASPEN, Nutri in Clin Practice 1996 (5):217-228 • Simplest level of nutritional care (level 1) – Baer et al, J Am Diet Assoc 1997 (10) S2:107-115 Examples of Screening risk factors • Anthropometrics: weight, length/height, BMI • Growth measures < than 5th %ile • Growth measures > than 90th %ile • Alterations in growth patterns – Change in Z-scores – Change 1-2 SD – Change percentiles • Medical and developmental Conditions • Medications • Improper or inappropriate food/formula choices or preparation • Psychosocial • Laboratory Values Examples of Screening risk factors • Jayden: – PG – Weight gain – Nutritional Practices • Barbara: – – – – Breastfeeding Weight changes Dietary practices Infant feeding practices • Mark – Newborn – Weight loss – Breastfeeding • Jake – 10 month old – Hct: 29 Assessment – Systematic process – Uses information gathered in screening – Adds more in depth, comprehensive data – Links information – Interprets data – Develops care plan – monitor – Reassess Process • Identify Problem or risk • Identify Etiology • Determine intervention • Monitor and Reevaluate Goals of Nutrition Assessment • To collect information necessary to document adequacy of nutritional status or identify deficits • To develop a nutritional care plan that is realistic and within family context • To establish an appropriate plan for monitoring and/or reassessment NCP: Nutrition Care Process • Provides a framework for critical thinking • 4 Steps – Assessment – Diagnosis – Intervention – Monitoring/Evaluation NCP • Assessment – Obtain, verify, interpret information – Data used might vary according to setting, individual case etc… – Questions to ask • Is there a problem? • Define the problem? • Is more information needed? NCP • Diagnosis – Identification or labling of problem that is within RD practice to treat • Examples: – Inadequate intake – Inadequate growth Examples of Nutrition Diagnosis Options • Altered GI Function • Altered nutrition related laboratory values • Decreased nutrient needs • Evident malnutrition • Inadequate proteinenergy intake • Excessive oral intake • Increased energy expenditure • • • • Increased nutrient needs Involuntary weight loss Overweight/obesity Limited adherence to nutrition related recommendations (vs food and nutrition related knowledge) • Underweight • Food and medication interactions NCP: • Diagnosis written as a PES statement Problem/Etiology/Signs and symptoms “Must be clear and concise. 1 problem one etiology” Examples of Screening risk factors • Jayden: – PG – Weight gain – Nutritional Practices • Barbara: – – – – Breastfeeding Weight changes Dietary practices Infant feeding practices • Mark – Newborn – Weight loss – Breastfeeding • Emma – 12 months – Weight @ 95th percentile – Diet information • Jake – 10 month old – Hct: 29 NCP Process Jayden, Barbara, Mark, Emma, Jake NCP • Intervention – Etiology drives the intervention • Monitoring and Evaluation Challenges and Pitfalls Challenges Nutrient needs influenced by: genetics, activity, body composition, medical conditions and medications Individuals anthropometric date influenced by: genetics, body composition, development, history Challenges • Identification of etiology • Weighing risk vs benefit • Supportive of: – Family – Individual – Development/temperament Challenges • Information – Availability – Accurate – Representative – complete • Goals and expectations – Available – Evidence bases – applicable Comprehensive Nutrition Assessment • Collection of Nutritional data • Interpretation of data – Linking information • Goals and expectations • Individual data • evidence – Asking questions • individualized intervention • monitoring outcomes of intervention Potential Pitfalls Excuses Assumptions Faulty reasoning Incorrect or inaccurate information Not evidence based Biased Information Collected: Current and Historical • • • • • • • Growth Dietary Medical history Diagnosis Feeding and developmental information Psychosocial and environmental information Clinical information and appearance (hair, skin, nails, eyes) • Other (laboratory) Assessment Tools Nutrition Assessment • Tools of Assessment – Growth • Measurements • Growth charts • Absolute size (percentile) • Pattern • Body composition – Water, bone, muscle, fat – Intake – Additional information – Intake • Food record, food recall, analysis – Additional information • • • • • • Medical, Development Social Laboratory Other anthropometrics etc • Who is the regulator of growth? • Who regulates Intake? • What do measurements mean? – Weight – Weight gain – Lab values – Intake information Growth Growth • Growth is a dynamic process defined as an increase in the physical size of the body as a whole or any of its parts associated with increase in cell number and/or cell size • Reflects changes in absolute size, mass, body composition Growth • A normal, healthy child grows at a genetically predetermined rate that can be compromised by imbalanced nutrient intake Growth Assessment • Progress in physical growth is one of the criteria used to assess the nutritional status of individuals Absolute size • Absolute size • Body composition • Growth/changes over time Absolute size Other Anthropometrics • Upper arm circumference, triceps skinfolds • Arm muscle area, arm fat area • Sitting height, crown-rump length • Arm span • Segmental lengths (arm, leg) All have limitations for CSHCN, but can be additional information for individual child Body Mass Index for Age • Body mass index or BMI: wt/ht2 • Provides a guideline based on weight, height & age to assess overweight or underweight • Provides a reference for adolescents that was not previously available • Tracks childhood overweight into adulthood Guidelines to Interpretation of BMI • Underweight –BMI-for-age <5th percentile • At risk of overweight –BMI-for-age 85th percentile • Overweight –BMI-for age 95th percentile Interpretation of BMI • BMI is useful for – screening – monitoring • BMI is not useful for – diagnosis Who might be misclassified? • BMI does not distinguish fat from muscle – Highly muscular children may have a ‘high’ BMI & be classified as overweight – Children with a high percentage of body fat & low muscle mass may have a ‘healthy’ BMI – Some CSHCN may have reduced muscle mass or atypical body composition Nutrient Analysis • • • • • • • Fluid Energy Protein Calcium/Phosphorus Iron Vitamin D Other Nutrient Needs • Recommendations established for over 43 essential and conditionally essential nutrients Basis of recommendations • Basis • Physiology – GI – Renal • Growth and Development – Preventing deficiencies – Meeting nutrient needs • • • • Water Energy Vitamin D Iron Dietary Information • Collect data • Nutrient Analysis • Comparison with recommendations, guidelines, evidence • Link with additional information • Interpret Dietary Information • • • • • • Family Food Usage 24 hour recall Diet history 3-7 day food record or diary Food frequency Other Information – Food preparation, history, feeding observation, feeding problems, likes/dislikes, feeding environment Approaches to Estimating Nutrient Requirements • Direct experimental evidence (ie protein and amino acids) • extrapolation from experimental evidence relating to human subjects of other age groups or animal models – ie thiamin--related to energy intake .3-.5 mg/1000 kcal • • • • • Breast milk as gold standard (average [] X usual intake) Metabolic balance studies (ie protein, minerals) Clinical Observation (eg: manufacturing errors B6, Cl) Factorial approach Population studies Dietary Reference Intakes (DRI) (including RDA, UL, and AI) are the periodically revised recommendations (or guidelines) of the National Academy of Sciences Comparison of individual intake data to a reference or estimate of nutrient needs • DRI: Dietary Reference Intakes – expands and replaces RDA’s – reference values that are quantitative estimates of nutrient intakes for planning and assessing diets for healthy people • AI: Adequate Intake • UL: Tolerable Upper Intake Level • EER: Estimated Energy Requirement DRI • Estimated Average Requirement (EAR): expected to satisfy the needs of 50% of the people in that age group based on review of scientific literature. • Recommended Dietary Allowance (RDA): Daily dietary intake level considered sufficient by the FNB to meet the requirement of nearly all (97-98%) healthy individuals. Calculated from EAR and is usually 20% higher • Adequate intake (AI): where no RDA has been established. • Tolerable upper limit (UL): Caution agains’t excess DRI • Nutrition Recommendations from the Institute of Medicine (IOM) of the U.S> National Academy of Sciences for general public and health professionals. • Hx: WWII, to investigate issues that might “affect national defense” • Population/institutional guidelines • Application to individuals. DRI’s for infants • Macronutrients based on average intake of breast milk • Protein less than earlier RDA • AAP Recommendations – Vitamin D: 200 IU supplement for breastfed infants and infants taking <500 cc infant formula – Iron: Iron fortified formula (4-12 mg/L), Breastfed Infants supplemented 1mg/kg/d by 4-6 months Other Guidelines • • • • AAP Bright Futures Educational or Professional teaching Public Policy Guidelines – Consider source – Consider Purpose – ? How apply to individual Examples • • • • • Baby cereal at 6 months Juice Introduction of Cows milk to infants Weight gain in pregnancy Family meals Factors that alter Energy needs • • • • • Body composition Body size Gender Growth Genetics • Ethnicity • Environment • Adaptation and accommodation • Activity/work • Illness/Medical conditions Energy • Correlate individual intake with growth Medical Information Medical Information and History • Conditions that may impact growth, nutritional status, feeding • Medications that may impact nutrient needs, absorbtion, utilization, or tolerance • Illness, treatments, proceedures Medical Conditions • • • • • • • • • • Congenital Heart Disease Cystic Fibrosis Liver disorders Short gut syndrome or other conditions of malabsorbtion Respiratory disorders Neuromuscular Renal Prematurity Recent illness Others Drug-Nutrient Interaction • • • • • • Altered absorbtion Altered synthesis Altered appetite Altered excretion Nutrient antagonists Tolerance Feeding and Developmental Information Feeding and development • • • • • Feeding Interactions Feeding Relationship Feeding Skills Feeding Development Feeding Behaviors • What factors influence food choices, eating behaviors, and acceptance? Feeding • • • • • Delays in feeding skills Feeding intolerance Behavioral Medical/physiological limitations Other Sociology of Food • • • • • Hunger Social Status Social Norms Religion/Tradition Nutrition/Health Psychosocial and environmental information Psychosocial and Environmental Information • Family – Constellation – Dynamics – Views – Resources – other • Socioeconomic status – employment/education/income/other • Beliefs – Religious/cultural/other Clinical and Laboratory assessment Clinical Assessment • • • • • • • General appearance Temperature Color Respiratory/WOB Skin/hair/nails/membranes Output (urine and stool) Other Clinical signs of Nutrient deficiency Energy FTT, cacexia Protein Slow growth, edema, impaired wound healing Calcium Seizures, rickets, decreased bone density, tetany Phosphorus Seizures, decreased bone density, rickets, bone pain, decreased cardiac fx Vitamin D Decreased bone density, osteopenia, rickets Vitamin A Dry scaly skin, FTT, xeropthalmia,, dry mucus membranes Zinc FTT, edema, impaired wound healing, alopecia, acrodermatitis enteropathica Iron Pallor, tachycardia, FTT Essential fatty acid Scaly dermatitis, poor growth, alopecia Vitamin C Swollen joints, impaired wound healing, swollen bleeding gums, loose teeth, petechia fluid Weight loss, decreased UOP, dry mucus membranes, altered skin turgor, sunken fontanel, tachycardia, altered BP Laboratory Assessmet • Laboratory tests can be specific and may detect deficiencies or excess prior to clinical symptomotology. • Useful for assess status, response to tx, tolerance • Validity effected by handling, lab method, technician accuracy, disease state, medical therapies • Complements other components of process Examples of Laboratory Tests Iron Hct, HgB, ferritin*, ZPPH* Protein/Energy Albumin, Transthyretin, RBP, other Bone Ca, Ph, Alk Pho, Vit D Vitamins Minerals Fluid Electrolytes, BUN, urine/serum osm, spec gravity Linking Information Assessment Process • Linking information collected with: – – – – Goals/expectations Reference data/standards Evidence individual • Asking questions Case Examples Yes No Not sure or don’t know growth diet Medical, developmental, feeding Social, environmental clinical laboratory Interpretation: Asking Questions Is there a problem? Was there a problem? Does information make sense? What are goals and expectations? What is etiology of the problem? Intervention Weighing Risks and Benefits • Identify etiology • Identify contributing factors • Support feeding relationship • Consider psychosocial factors, family choice and input • Weigh risk v.s. benefit Etiology: Contributing factors Inadequate Intake Fluid, energy Medical BPD, reflux, frequent illness Feeding relationship Stress, history Psychosocial Weighing Risks and Benefits • Adequate intake vs feeding relationship • Concentrating formula vs fluid status • impact on tolerance, compliance, errors, cost • solution to problem vs exacerbating problem Summary: Screening Assessment Diagnosis Intervention Monitoring and reevaluation Summary • Identify Problem or risk • Identify Etiology • Determine intervention • Monitor and Reevaluate Summary: Assessment Process • Collect data • Interpret data – Link information – Compare to references, standards, expectations – Ask questions