Preoperative Care of Pulmonary Patients: An evaluation for
advertisement
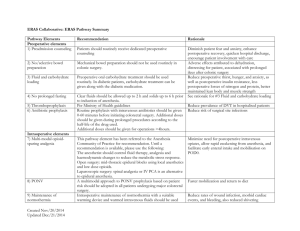
reoperative Care of Pulmonary Patients: An evaluation for postoperative pulmonary complications Anakapong Phunmanee MD. Associated Professor Department of Medicine, Faculty of Medicine, Khon Kaen University Topics • The concepts for performing effective consultation • Factors related to PPCs • Preoperative pulmonary evaluations • Risk indices for preoperative assessment • Risk reduction strategies • Preoperative care of pulmonary patients: An example The concepts for performing effective consultation • • • • • • • • Prompt response (within 24 hours) Focus on central issue Identified critical recommendations Make specific and limit number of recommendations(<5) Use definitive language Direct verbal contact Specific drug dosage, route, frequency Frequent F/U and progress note Cohn SL. UptoDate 2002 The ideal medical consultation • • • • Informs without patronizing Educated without lecturing Directs without ordering Solves the problem without making referring physician appear to be “stupid” Bates RC, et al. Med Econ 1997 “ Referring physician and the consultant both have responsibilities to fulfill in order to maximize the effectiveness of the consultation in improving the patient care” Cohn SL. UptoDate 2002 The role of preoperative medical consultation • Identifying and evaluation the medical status • Provide a clinical risk profile • To optimize the medical condition in attempt to reduce risk of PPCs Postoperative pulmonary complications (PPCs) • Common complications, ¼ of death related to PPCs • Incidence and prevalence vary – Population – Type of surgery – Definition of complications Brooks-brunn JA .Heart Lung 1995 Factors related to PPCs • • • • Patients-related risk factors Operation-related risk factors Anesthetic-related risk factors Risk factors related to postoperative care Patient-related risk factors: Aging Postoperative pneumonia (OR) > 80 YRs 70-79 YRs 60-69 YRs 50-59 YRs < 50 YRs 0 1 2 3 4 5 6 7 Arozullah AM,et al. Ann Intern Med 2001 Ann Surg 2000 Patient-related risk factors: General health Postoperative pneumonia (OR) Total depend Partial depend ASA >,=2 CVA Obesity 0 1 2 3 4 5 6 7 Arozullah AM,et al. Ann Intern Med 2001 Ann Surg 2000 Patient-related risk factors: Immune status Postoperative pneumonia Steroid use Postoperative pneumonia and respiratory failure Alcoholic > 2 drink/day Within 2 wks Postoperative pneumonia IDDM 0 1 2 3 4 5 6 7 Arozullah AM,et al. Ann Intern Med 2001 Ann Surg 2000 Operation-related risk factors Postoperative respiratory failure (OR) AAA-repair Thoracic Upper abdomen Neck Neurosurgery Vascular 0 1 2 4 6 8 10 12 14 16 Arozullah AM,et al. Ann Intern Med 2001 Ann Surg 2000 Influence of surgical site on rate of PPCS Laparoscopic Upper Abdomen Lower abdomen Tarhan 1973 13 7 10 Garcey 1979 25 0 19 Garribaldi 1981 17 5 40 Study SSA club 1994 0.3 Phillips 1994 0.4 Brooks 1997 28 Thoracic 15 Smetana GW, et al New Engl J Med 1999 Mortality for lung resection 12 % Mortality 10 8 6 4 2 0 wedge resection segmental resection lobectomy pneumonectomy Multicenter study 12,00 patients , thoracotomies usually CA Mitsudomi T, et al. J Surg Oncol 1996; 61:218-22 Anesthetic-related risk factors General anesthesia (thoracic, Ab, Vascular) Operation time >3 hrs 0 1 2 3 4 5 6 7 Smetana GW, et al New Engl J Med 1999 Neuromuscular block and PPCs: Long acting VS shorter acting Incidence of Complication 18 16 14 12 10 8 6 4 2 0 long acting* Shorter acting** Incidence of residual NMB 26*, VS 5.3** Berg H, et al Acta Anaesthesiol Scand 1997 Risk factors related to postoperative care • NG tube – Postoperative NG tube not significant associated with PPCs – Empty GI tract may decrease aspiration outweigh risk of ineffective coughing and oropharygeal aspiration • Pain control – Adequate pain control improving outcomes – Epidural analgesia seem to be better outcomes than standard opioid analgesia Preoperative pulmonary evaluations • • • • • • History and physical examination Chest radiography Arterial blood gas analysis Pulmonary function test Quantitative lung scan Exercise test Chest radiography Two potential indication 1. To identified abnormalities correcting, modification cancellation surgery 2. Serve as a base line finding The value of an abnormal CXR before surgery 60 Abnormal Normal 50 40 30 20 10 0 Makee 1987 Wiencek 1987 Charpak 1988 Tape 1988 Bouillot 1996 Silvestri 1999 Smetana GW, et al Med Clin N Am 2003 The abnormal CXR and aging 50 45 40 35 30 25 20 15 10 5 0 < 60 >60 Silvestri L, et al Eur J Anaesthesiol 1999 Recommendation for preoperative CXR • Age > 50 years • Known pre-existing cardiopulmonary diseases • S/S like hoods of cardiopulmonary disease Smetana GW, et al Med Clin N Am 2003 Arterial blood gas • Small study series identified Hypercarbia(PaCO2>45) risk for PPCs Milledge JR, et al. BMJ 1975 Stein M, et al. JAMA 1962 • Recent systematic review by Fisher BW, et al 2002 dose not find hypercarbia useful predictor for PPCs Spirometry Pulmonary function testing (PFTs) and PPCs • ACP guideline 1990 – Lung resection 40% PFTs do not meet – Coronary artery bypass surgery guideline – Upper abdominal surgery with smoking or dyspnea Improving adherence – Lower abdominal surgery if unexplained ordering PFTs saving pulmonary diseases with prolong extensive surgery 29-100 million Dollar/Yr – Head, neck, orthopedic surgery with unexplained pulmonary diseases Anonymous. Ann Intern Med 1990; 112:793-4. Use of preoperative spirometry to predicted PPCs Jacob 1997 Bando 1997 Kocabas 1996 Kroenke 1993 Kispert 1992 Swensson 1991 Fogh 1987 Appleberg 1974 Stein 1970 Collin 1968 0 1 2 4 6 8 10 12 14 16 Adapt from Smetana GW,et al. New Engl J Med 1999;340:937-944. PFTs and PPCs • Case-control study, elective abdominal surgery: – CXR highly associated with PPCs (OR 5.8) – Abnormal PE associated with PPCs – Whereas PFTs were not predictive Lawrence VA, et al. Chest 1996;110:744-50. PFT Diagram in Preoperative Evaluation FEV1 >2 L MVV >50% DLCO >60% PFT(FEV1,MVV,DLCO) Cleared for any resection PPO-FEV1 >1.3 Cleared for any resection FEV1 > 2 L MVV<50% DLCO <60% FEV1 <2 L High risk consider exercise test Perfusion Scanning PPO-FEV1 PPO-FEV1 <0.8 Consider “Lesser” resection Non surgical therapy PPO-FEV1 >0.8, <1.3 High risk consider exercise test Preoperative PFTs : Summary • Thoracic surgery • Upper abdominal surgery with respiratory symptoms remain unexplained after careful evaluation • Routine PFTs should not ordered solely without clinical assessment Arozullah AM. Med Clin N Am 2003; 87: 153-173 uantitative lung scan Interpretation of quantitative lung scan Exercise testing • Assessing the risk in pts undergoing thoracotomy is controversial • Acceptable value; maximum oxygen consumption > 15 ml/kg/min Risk indices for preoperative assessment Pneumonia Risk (total point) Predicted Prob. pneumonia (%) Respiratory Failure (total point) Predicted Prob. Res. failure (%) 1 0-15 0.2 0-10 0.5 2 16-25 1.2 11-19 2.2 3 26-40 4.0 20-27 5.0 4 41-55 9.4 28-40 11.6 5 >55 15.4 >40 30.5 Risk class Arozullah AM,et al. Med Clin N Am 2003 ตัวอย่ างการประเมินโดยใช้ Risk indicies • • • • • ผูป้ ่ วยชายอายุ 60 ปี (9) ต้องเข้ารับการผ่าตัดมะเร็ งปอดระยะIIa (14) มีประวัติสูบบุหรี่ 30 pack/year จนหยุดสู บมา 4 สัปดาห์ (3) ได้รับการวินิจฉัยเป็ น COPD (5) รวมได้คะแนน 31 จากตาราง risk class 3 ซึ่ง predicted prob. pneumonia 4%, respiratory failure 11.6 % Limitation of risk indicies • Developed from male, high co morbid level may not generalized to healthy population • Hospital based study from Veterans Hospital Arozullah AM,et al. Ann Intern Med 2001 Ann Surg 2000 Risk reduction strategies(1) • Smoking cessation at least 8 weeks • Perioperative lung expansion maneuver – Incentive spirometry – Chest physical therapy – Intermittent positive pressure breathing (IPPB) – Continuous positive airway pressure (CPAP) Preoperative smoking cessation and PPCs % Complication 60 50 40 30 20 10 0 Stop >2 mth Stop<2 mth Stop>6 mth Never smoke Prospective study 200 patients, CABG Warner MA,et al. Mayo Clin Proc 1989 Preoperative smoking cessation and PPCs % Complication 60 50 40 30 20 10 0 Current <2wks Recent2-4wks Exsmoke Never smoke Retrospective study 288 patients, pulmonary surgery Nakagawa M, et al Chest 2001;120:705-10 Paradoxical increase PPCs after short-term abstinence • Sicker pts tend to quit smoking closer to surgery • Stop smoking decrease irritation decrease stimulus for cough Still have bronchial hypersecretion increase sputum retention Bluman LG, et al. chest 1998 Warner MA, et al. Mayo Clin Proc 1989 Short term smoking cessation • Decrease carboxyhemoglobin and nicotine level Improved mucocilliary function and upper airway hypersensitivity Buist AS, et al. Am Rev Respir Dis 1976 Camner P, et al. Chest 1973 Kamban JR,et al. Anesth Analg 1986 Risk reduction strategies(2) • Smoking cessation at least 8 weeks • Perioperative lung expansion maneuver – Incentive spirometry – Chest physical therapy – Intermittent positive pressure breathing (IPPB) – Continuous positive airway pressure (CPAP) Perioperative lung expansion maneuvers • A meta-analysis evaluating: upper abdominal surgery – Incentive spirometry (IS) – Deep breathing exercise (DB) – Intermittent positive pressure breathing (IPPB) • Similar in efficacy • Better than no respiratory therapy Thomas JA, et al. Physical Therapy 1994; 74:3-10. Perioperative lung expansion maneuvers: Summary • No specific lung expansion maneuver is clearly superior • CPAP may be benefit in patients unable to perform DB or IS • Initiative lung expansion maneuver preoperatively is more effective in reducing PPCs than postoperatively Arozullah AM. Med Clin N Am 2003; 87: 153-173 Risk-reduction strategies: preoperatively • Encourage smoking cessation at least 8 weeks • Delay operation if respiratory infection is present, productive cough (several weeks) • Education lung expansion maneuvers • Maximize pulmonary function – – – – Bronchodilator Inhaled corticosteroid Theophylline Antibiotic Smetana GW, et al. New Engl J Med 1999; 346: 937-944. Risk-reduction strategies: Intraoperatively • • • • Limit duration of surgery to <3 hours Use spinal or epidural anesthesia Avoid pancuronium Use laparoscopic procedure when possible Smetana GW, et al. New Engl J Med 1999; 346: 937-944. Risk-reduction strategies: postoperatively • • • • Adequate pain control Early ambulation Use lung expansion maneuver Maximized pulmonary function (medication) To The last Smetana GW, et al. New Engl J Med 1999; 346: 937-944. Preoperative Care of Pulmonary Patients: Example(1) • • • • Male 60 yrs. Dx: NSCLC stage Ib , RUL Underlying COPD Assessment – Not urgent surgery, high benefit – Risk ; elderly, COPD – History / Physical examination – Laboratory Spirometry of the patient PreRX(%) Post – RX(%) 55 60 FEV1 (L) 1.31(48) 1.39(53) 5 FVC (L) 2.40(66) 2.50(69) 4 FEF25- 75% 0.43(15) 0.6(22) 22 FEV1/FVC %CHG (%) (L/min) Further evaluation • PPO-FEV1 RUL = 24.7% LL = 55% RLL= 20.3% RUL : RLL= 0.55: 0.45 Preoperative Care of Pulmonary Patients: Conclusion • Many factors related to PPCs • Working as a team plays major roles • Assessment of the risks ,do appropriated testing and modifying are the keys of preoperative caring Thank you Go Back