Ch 27
advertisement
Reproductive
System
Chapter 27
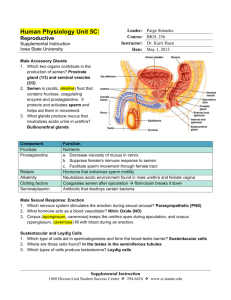
Male Reproductive System
Anatomy
Scrotum
Testes
Penis
Duct
system
Accessory glands & semen
Scrotum
Figure 27.2
Maintains testicular temperature at ~ 3oC lower than core
temperature
Surface area varies in response to external temperature
Testes
Figure 27.3a
Primary reproductive organ of the male:
Produces
sperm & testosterone
Testicular lobules contain coiled seminiferous tubules.
Seminiferous tubules: the location of sperm production
Interstitial cells in the connective tissue around the
seminiferous tubules produce testosterone
Penis
Designed to deliver
sperm into the female
reproductive tract
Penile root
Penile shaft
Glans penis
Figure 27.4
Penis
Corpus spongiosum
midline
& ventral surrounds
urethra; proximally forms the
bulb of the penis; distally
forms glans penis
Corpora cavernosa
paired
dorsal erectile bodies
that terminate proximally in
the crura (crus) of the penis
that are anchored to the
pubic arch
Duct system: male
Epididymus
Vas deferens
Urethra; (three regions)
Prostatic urethra
Membranous urethra
Penile urethra
Duct system:
male
Figure 27.3a
Epididymus: receives immature sperm from the rete testis; as
the sperm move through the epididymus (~20 days) they
become fully motile
Duct system: Male
Figure 27.3a
Ductus (vas) deferens: from the epididymus merges with the
Seminal vesicle duct to form the
Ejaculatory duct which enters the
Prostate & empties into the urethra
Duct system: male
Figure 27.1
Urethra: serves both urinary & reproductive systems
Three regions
Prostatic urethra
Membranous urethra
Penile urethra
Accessory glands – Seminal Vesicles
Figure 27.1
on posterior bladder wall:
make alkaline, seminal fluid containing: fructose,
ascorbic acid, vesiculase (coagulating enzyme) &
prostaglandins:
Seminal fluid: 2/3 of volume of semen
Accessory glands - Prostate gland
Figure 27.1
Surrounds urethra
Produces a milky, slightly acidic fluid
citrate,
multiple enzymes & PSA (prostate specific antigen):
Prostatic fluid: ~1/3 of semen volume
Accessory glands
Figure 27.1
Bulbourethral glands:
Produce a thick clear mucous that neutralizes acidic urine
Semen
Semen:
Milky white mixture of sperm & accessory gland
secretions
Provides:
Nutrients for sperm
Chemical protection / activation
Acts as a transport medium for sperm
Male Sexual Response
Erection: enlargement & stiffening of the penis
Parasympathetic reflex
Triggers
local release of Nitric Oxide causing
Arteriolar dilation & increased blood flow to erectile tissues
Expansion of erectile tissues interferes with veins that
drain the system & maintains erection
Male Sexual Response
Ejaculation: propulsion of semen through the duct
system
SNS discharge causes
Contraction throughout the ductal system
Contraction of bladder sphincter &
Contraction of the bulbospongiosus muscles of the
penis
Male Sexual Response
Refractory period: After ejaculation there is a
refractory period during which a male is unable to
have another ejaculation (minutes hours)
Spermatogenesis
Cell differentiation events that produces male gametes
(spermatozoa)
Spermatogenesis
Diploid (2n):
having
human 2n=46
Haploid:
having
2 of each chromosome type (n)
1 of each chromosome type human n = 23
body cells are diploid (2n)
Gametes are haploid (n)
When 2 gametes fuse at fertilzation, n + n = 2n
diploidy
restored
Comparison of Mitosis & Meiosis
Figure 27.6
Meiosis:
Two consecutive nuclear divisions producing
Four haploid daughter cells
Meiotic Cell Division: Meiosis I
Figure 27.7
Meiosis:
Meiosis I: separates homologous chromosomes into
different cells
(i.e. diploid haploid)
cells still retain 2 copies of each gene
Meiotic Cell Division: Meiosis II
Figure 27.7
Meiosis:
Meiosis II: separates chromatids into separate cells
generates cells with only 1 copy of each gene
Spermatogenesis
Occurs in the seminiferous tubules;
Spermatogonia form epithelial basal layer of cells
Spermatogonia (sperm stem cell)
Divide by mitosis until puberty forming a large
population
Spermatogenesis
At puberty mitotic divisions of spermatogonia form
Two daughter cells with different functions
Type A cells
Type B cells
Spermatocytes to Spermatids
Type A: remains to maintain the spermatogonia stem cell
Type B: primary spermatocyte (2n):
Pushed toward lumen
Meiosis I forming secondary spermatocytes (n) which undergo
Meiosis II forming 4 spermatids (immature sperm)
Spermatogenesis: Spermatids to Sperm
Figure 27.9a
Spermatogenesis: (spermatids sperm) a streamlining
process
Sperm head (filled with DNA)
Acrosome (filled with lysosomal enzymes)
Midpiece (mitochondrial wrapped contractile filaments)
Tail (flagellum)
Spermatogenesis
Sertoli (Sustentacular)
cells:
Divide seminiferous tubule
into 2 compartments;
Isolate
newly formed sperm
from blood:
blood-testis barrier prevents
formation of antibodies
against sperm
Hormonal Regulation: Male
Brain-testicular axis:
Interactions between:
Hypothalamus
Anterior pituitary
Testes
Brain-testicular axis
Hypothalamus Gonadotropin-Releasing Hormone
(GnRH)
GnRHAnterior pituitary secretion of
Leutinizing Hormone (LH a.k.a. Interstitial Cell Stimulating
Hormone: ICSH)
Stimulates interstitial cells to produce testosterone
Follicle
Stimulating Hormone (FSH)
allows spermatogenesis by making cells receptive to testosterone
Brain-testicular axis
Testosterone acts locally as the trigger for
spermatogenesis
Testosterone inhibits:
Release
of GnRH (hypothalamus)
Release of gonadotropins (anterior pituitary)
Inhibin is produced by Sertoli cells when sperm
counts are high; inhibits GnRH & FSH release
Hormonal Regulation of Testicular
Function
Feedback inhibition on
hypothalamus & pituitary
from:
Rising levels of
testosterone
Increased inhibin
Figure 27.10
Brain-testicular axis
Perinatal FSH, LH & testosterone levels:
Near pubertal levels to allow development of
the male reproductive system;
After a few months of age the levels drop to
low levels until onset of puberty
Testosterone mechanism & effects:
Testosterone is synthesized from cholesterol &
exerts effects by activating specific genes
Testosterone targets accessory organs (ducts,
glands & penis) causing them to grow to adult
proportions
Testosterone mechanism & effects:
Testosterone induces:
Secondary sex characteristics:
pubic & axillary hair
voice change
facial hair
thickening of the skin
increased sebum production
increase in bone & muscle mass
Female Reproductive System
Figure 27.11
Anatomy
Ovaries
Duct System:
Fallopian Tubes
Uterus
Vagina & external genitalia
Ovaries
Figure 27.14a
Ovaries: primary female reproductive organ
Ovaries produce the female
Gamete (ova/egg)
Sex hormones (estrogens & progesterone)
Ovaries
Figure 27.14a
Ovaries: paired organ
Found on either side of the uterus
Held in place by ligaments
Ovaries
Figure 27.12
Ovarian follicles within the ovary consist of an:
Oocyte
(immature ovum) encased in one or more layers of
cells
Single layer: follicle cells;
Multiple layers: granulosa cells
Follicles at different stages have different structures
Ovaries
Figure 27.12
Follicle stages & structures:
Primordial
follicle: single layer of follicle cells surrounding
oocyte
Primary follicle: two or more layers of granulosa cells
Secondary follicle: fluid filled spaces appear within granulosa
& merge to form the vesicular follicle.
Ovaries
Figure 27.12
Follicle stages (cont):
Vesicular
(Graafian) follicle: bulges from the ovary surface &
will rupture at ovulation releasing the oocyte
Corpus luteum: follicle remnant after rupture that forms the
glandular corpus luteum
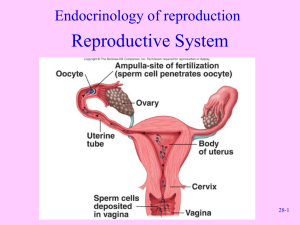
Female Duct System
Figure 27.14a
Fallopian tubes: uterine tubes, oviducts
Infundibulum:
open funnel shaped structure with finger-like
projections (fimbriae) that drape over ovary
Ampulla: widened region arching over ovary (the usual site
of fertilization)
Isthmus: narrowed region where tube enters upper region of
uterus
Female Duct System - Uterus
hollow, thick walled, pear shaped, muscular organ that
receives, retains & nourishes a fertilized ovum
Uterine support comes from the mesometrium, the
lateral cervical ligaments, the uterosacral ligaments &
the round ligaments
Female Duct System: Uterine Wall
Endometrium: mucosal lining of columnar epithelium
Myometrium: muscular middle layer: interlaced bundles of
smooth muscle
Perimetrium: outer covering of visceral peritoneum
Female Duct System: Uterine Wall
endometrium is a dynamic layer of
epithelium with two layers
Stratum functionalis: undergoes
cyclic changes in response to
ovarian hormones & is shed during
menstruation
Stratum basalis: deeper layer that
forms a new stratum functionalis
after menstruation
Figure 27.15
Vagina
Figure 27.14a
female organ of copulation & birth canal
Vagina
Figure 27.14a
3 layers
Mucosa: stratified squamous epithelium with rugae (ridges)
Muscularis: smooth muscle
Adventitia: fibroelastic connective tissue
Vagina
Figure 27.14a
Environment:
In adults, vaginal pH is decreased
Helps to prevent infection
Also hostile to sperm
In adolescents, vaginal pH is increased
More alkaline environment presents an increased risk for
Sexually Transmitted Disease
Vagina
Proximal end of the vagina:
Surrounds the cervix of the uterus
Forming a recess (fornix) around the cervix;
Distal end forms the vaginal orifice with mucosal
hymen (in virginal females)
External Genitalia
Figure 27.16
Mons pubis: rounded fat pad overlying the pubic symphysis
Labia
Labia majora: two fatty skin folds with hair (homologous to
scrotum)
Labia minora: two smaller, hairless skin folds (homologous
to the male ventral penis)
External Genitalia
Figure 27.16
Vestibule = the recess surrounded by the labia minora includes:
Urethral opening
Vaginal orifice
Vestibular gland orifices
External Genitalia
Clitoris:
Small, protruding structure:
Composed of erectile tissue (penis homolog)
Hooded by anterior folds of the labia minora (prepuce of
clitoris)
Perineum: diamond shaped region from pubic arch to coccyx &
laterally to the ischial tuberosities
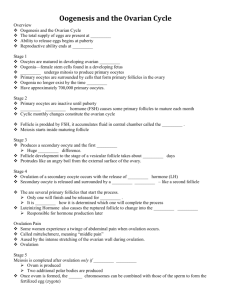
Oogenesis
Figure 27.20
maturation process for the ovum (egg);
Oogonia: fetal stem cells (diploid) start meiosis to
become primary oocytes.
Oogenesis
Figure 27.19
Oogenesis
Figure 27.19
Two routes for secondary oocyte:
If
fertilized - secondary oocyte expels second polar body
(nonviable) & rapidly completes Meiosis II
If unfertilized - secondary oocyte deteriorates
The Ovarian Cycle:
28 Days
Follicular phase: days 1-14
Luteal phase: days 14-28
Follicular phase:
Figure 27.20
Days 1 -14
Primordial follicle matures to form a primary follicle
Follicular cells proliferate forming granulosa cells
which regulate / stimulate oocyte maturation
Follicular phase:
Figure 27.20
Days 1 -14 (cont)
Connective tissue condenses around the follicle forming:
The theca folliculi; theca & granulosa cells produce estrogens
Granulosa cells produce:
A transparent membrane (zona pelucida) around the oocyte
Clear liquid forms the antrum (cavity) of the secondary follicle
Follicular phase:
Figure 27.20
Days 1 -14 (cont)
Antrum expands until the oocyte is isolated on a stalk
within the follicle
Now ~1in. in diameter the vesicular follicle bulges from
the surface of the ovary; the oocyte is surrounded by a
capsule of granulosa cells (corona radiata)
Follicular phase:
Figure 27.20
Day 14
Ovulation: the vesicular follicle wall ruptures, expels
the secondary oocyte with its corona radiata
Luteal phase:
Figure 27.12
Figure 27.20
Days 14-28
The ruptured follicle collapses & remaining theca &
granulosa cells enlarge & form an endocrine gland:
the corpus luteum
Luteal phase:
Figure 27.12
Figure 27.20
Days 14-28 (cont)
The corpus luteum secretes progesterone & some
estrogen
If
no fertilization occurs the corpus luteum degenerates to
form the corpus albicans (scar)
If fertilization occurs the corpus luteum persists until the
placenta takes over hormone production (~3 mos.)
Gonadotropins, Hormones, & the Ovarian &
Uterine Cycles
Figure 27.22a, b
Hormonal Regulation:
During puberty GnRH (& thus
FSH/LH) production
increases until the adult cycle
is achieved:
First menses = menarche
Figure 27.22a, b
Hormonal Interactions:
Day 1
Day 1: GnRH levels rise stimulating anterior pituitary
release of FSH & LH
FSH & LH stimulate follicle growth & maturation;
LH stimulates theca cells to produce androgens
which diffuse into the follicle & are converted to
estrogens by granulosa cells
Feedback Mechanisms in Ovarian Function
Figure 27.21
Hormonal Interactions:
Rising estrogen levels provide negative feedback to
the anterior pituitary
Inhibiting release of FSH/LH but encouraging storage
of FSH/LH
Within the ovary estrogen intensifies the effect of FSH
enhancing estrogen production
Hormonal Interactions:
As estrogen continues to rise it exerts a positive
feedback on the adenohypophysis resulting in a burst
of LH
Figure 27.21
Hormonal Interactions:
Day 14
LH surge prompts maturation of the primary follicle to
form the secondary oocyte & triggers ovulation
Figure 27.21
Hormonal Interactions:
At ovulation, estrogen levels decline
LH surge also transforms the ruptured follicle into a
corpus luteum
Stimulates production of progesterone & estrogen
Figure 27.21
Hormonal Interactions:
Rising progesterone & estrogen exert negative
feedback of FSH/LH release
Figure 27.21
Feedback Mechanisms in Ovarian Function
Figure 27.21
Hormonal Interactions:
Day 27
After the corpus luteum stops functioning the decline
in hormone levels allows
{Day 1} Increased GnRH (FSH/LH)
Gonadotropins, Hormones, & the Ovarian &
Uterine Cycles
Figure 27.22c, d
The Uterine Cycle
Days 1-5
Menstrual phase: uterus sheds stratum functionalis of
endometrium.
Hormone levels are at their lowest
GnRH & FSH begin to rise
The functionalis layer detaches from the stratum
basalis & is passed through the vagina (3-5 days of
bleeding)
The Uterine Cycle
Days 6-14
Proliferative phase: Endometrium rebuilds itself.
Estrogen induces progesterone receptors in the
endometrial cells;
The proliferative phase ends with ovulation &
associated rise in LH
The Uterine Cycle
Days 15-28
Secretory phase: endometrium is prepared for
implantation of the embryo.
Progesterone acts on the endometrium
Spiral arteries enhance blood supply
The functionalis is converted into a secretory
mucosa (secretes glycogen)
The Uterine Cycle
Days 15-28
As progesterone levels rise, LH levels decline:
If fertilization has not occurred the progesterone
level declines (corpus luteum degenerates) & the
endometrium degenerates.
If fertilization has occurred: Ch 28
Menstrual cycle
Gonadotropins, Hormones, &
the Ovarian & Uterine Cycles
FSH, LH, Follicle, Uterus
Figure 27.22 a,b,c, d
Estrogen mechanism & effects:
Estrogen induces:
Secondary sex characteristics:
Growth of the breasts
Increased deposits of subcutaneous fat
Widening & lightening of the pelvis
Female sexual response
Clitoris, vaginal mucosa & breasts become engorged
with blood
Clitoral & Nipple erection
Increased vestibular gland activity lubricates the
vestibule
Female orgasm
No ejaculation
Muscle tension increases throughout the body
Pulse & BP rise
Uterus contracts rhythmically
No refractory period
Sexually Transmitted Disease
Gonnorrhea: Neisseria gonnorrhea
Invades the mucosa of the reproductive tracts:
Congenital blindness
Male: urethritis, painful urination
Female: variable symptoms: may lead to PID (pelvic
inflammatory disease) & sterility
Sexually Transmitted Disease
Syphilis: Treponema pallidum:
Primary: Initial presentation of chancre at the site of
infection;
Painless,
heals spontaneously;
Congenital death
Secondary: pink skin rash, fever & joint pain
Tertiary: destructive lesions (gumma) in CNS, blood
vessels, bone & skin
Sexually Transmitted Disease
Chlamydia: Chlamydia trachomatis;
Congenital: conjunctivitis blindness, pneumonia
Male: urethritis, testicular pain, urogenital
inflammation, arthritis
Female: 80% no symptoms; PID may lead to sterility
Final Freebie
All somatic body cells = diploid
_______ogonia = diploid
Primary ___cyte = diploid
Secondary ___cyte = haploid
Gamete (Sperm/ova) = haploid
Structure of Lactating Mammary Glands
Figure 27.17
Development of Internal Reproductive
Organs
Figure 27.24
Development of Internal Reproductive
Organs
Figure 27.24
Development of Internal Reproductive
Organs
Figure 27.24
Development of Internal Reproductive
Organs
Figure 27.24
Development of Internal Reproductive
Organs
Figure 27.24
Development of External
Genitalia: Male
Figure 27.25a
Development of External Genitalia: Male
Figure 27.25b
Development of External
Genitalia: Female
Figure 27.25a
Development of External Genitalia: Female
Figure 27.5c
Development Aspects: Descent of the
Gonads
Figure 27.26a
Development Aspects: Descent of the
Gonads
Figure 27.26b
Development Aspects: Descent of the
Gonads
Figure 27.26c