Sepsis
advertisement

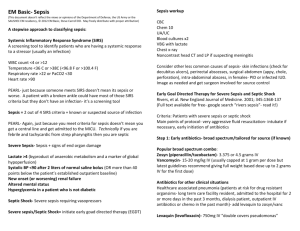
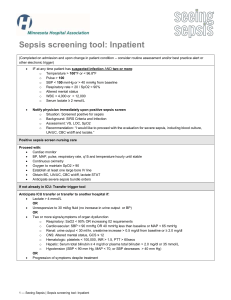
Sepsis Sepsis “A little less conversation, a little more action please” Aims of this session • To use Surviving Sepsis guidelines as a framework • To focus on practical interventions that can improve outcome in the septic patient • To encourage you to think like intensive care doctors • To be as interactive as possible At the end of this session you will be able to • Define and use important terminology • Identify features of organ failure • Prioritise urgent interventions in the septic patient • Describe an effective fluid challenge • Demonstrate how CVP can be used to guide fluid resuscitation • Explain ScvO2 and how it can indicate tissue dysoxia Definitions • Systemic Inflammatory Response Syndrome (SIRS) • Sepsis • Severe Sepsis • Septic Shock ‘SIRS’ ‘SIRS’ • 2 or more of the following: – Temp >38ºC or <36ºC – HR >90 beats/min – RR >20 breaths/min or PaCO2 <4.5kPa – WBC >12,000 or <4000 cells/mm3, or >10% immature (band) forms ‘Sepsis’ ‘Sepsis’ • SIRS in the presence of proven or suspected infection ‘Severe Sepsis’ ‘Severe Sepsis’ • Sepsis associated with hypotension, hypoperfusion and/or organ-dysfunction ‘Septic Shock’ ‘Septic Shock’ • Sepsis with hypotension despite adequate fluid resuscitation • May be ‘vasodilatory’ and/or ‘distributive’ shock • Include all patients on vasopressors or inotropic support Organ Failure • • • • • • CVS RS Renal Hepatic CNS Haematological Prognostic effects of organ dysfunction in severe sepsis Prevalence of hospital mortality associated with severe sepsis Case 1 You are called to Resus to review an 78 year old female who presented with confusion, fever and rigors. She is unable to give a history. Her observations on admission are 38.30c, BP 70/35 Pulse 120 RR 30 What are your thoughts? What would you like to do next? Case 2 A ICU nurse asks you to urgently see an elective cardiac patient who has just arrived from theatre, ventilated but has had no medical handover His obs are T35.5, BP 80/50, P100, CVP 10, SpO2 99 on 40% O2 Why is this patient hypotensive? Case 3 The A&E SpR calls to discuss the case of a 50 year old overweight, hypertensive, diabetic female with upper abdominal pain and shock. The surgeons have just started an AAA repair in theatre. Obs: T35, BP 90/40, P100, RR36, SpO2 unrecordable • What is the differential diagnosis? • What would you like to do next? How do we manage sepsis and septic shock? 1) Investigate and treat sepsis • • • Try and find and treat source Early blood cultures Start antibiotics asap ideally within 1 hour and after cultures taken 2) Assess extent of end organ hypoperfusion and improve oxygen delivery (early goal directed therapy) Oxygen delivery What does it mean? Oxygen delivery What does it mean? Delivery (DO2) = O2 content x cardiac output = ([Hb] x SpO2 x 1.34) x (HR x SV) Oxygen content = [Hb] x SpO2 x 1.34 Cardiac output = HR x SV Fluid Challenge What is the difference between an infusion and a challenge? Fluid Challenge What is the difference between an infusion and a challenge? 250 to 500 ml colloid (or blood products) 500 to 1000ml Hartmann’s [NOT 5% dextrose] As fast a possible (with pressure bag) You at the bedside Fluid Challenge Aim is to improve SV (and hence CO) by increasing preload Frank-Starling mechanism Markers of perfusion What are they? Markers of perfusion What are they? • Clinical signs – Warm skin, conscious level, u/o • Haemodynamic variables – CVP • Bloods – Serum Lactate – ScvO2 CVP What does it mean? CVP What does it mean? Starling’s Law Estimate of LVEDV (i.e. preload) Not always a good correlation with volume-responsiveness However if low strongly suggestive of hypovolaemia Lactate What does it mean? Lactate What does it mean? • Increased production (anaerobic glycolysis) – Tissue hypoperfusion – Tissue dysoxia • Reduced metabolism – Hepatic – Renal • <1 is normal, 1-2 is a concern, >2 is bad, >4 is very bad ScvO2 What does it mean? ScvO2 What does it mean? • Balance between oxygen delivery and consumption (VO2) • Fick principle • ScvO2 = SaO2 - VO2 CO • Target > 70% ScvO2 What can I do if it’s low? ScvO2 What can I do if it’s low? Delivery = [Hb] x SpO2 x 1.34 x HR x SV ScvO2 What can I do if it’s low? Delivery = [Hb] x SpO2 x 1.34 x HR x SV Fluid optimise Transfuse packet cells HCt > 30% Inotropes Surviving Sepsis targets of fluid resuscitation What are they? • • • • • • • SBP MAP CVP U/o Lactate ScvO2 HCt Surviving Sepsis targets of fluid resuscitation What are they? • • • • • • • SBP > 90 MAP > 65 CVP 8 - 12 U/o > 0.5 ml/kg/hr Lactate < 1 ScvO2 >70 HCt > 30 Further Management What else can be done? Further Management What else can be done? • • • • • • • Low tidal volume ventilation Steroids in septic shock Activated Protein C Glycaemic control Stress ulcer prophylaxis Thromboprophylaxis Sedation scoring / holds etc. Any Questions? Take Home Message(s) • Early intervention saves lives • Send cultures immediately • Give antibiotics early (<1 hour on ICU, <3 hrs A&E) • Aggressive targeted fluid resuscitation on the spot (early goal-directed therapy) • CVC / ScvO2 if shocked / Lactate > 4 • Involve surgeons/radiologists early (source control) At the end of this session you are now able to • Define and use important terminology • Identify features of organ failure • Prioritise urgent interventions in the septic patient • Describe an effective fluid challenge • Demonstrate how CVP can be used to guide fluid resuscitation • Explain ScvO2 and how it can indicate tissue dysoxia