pneumonia II
advertisement
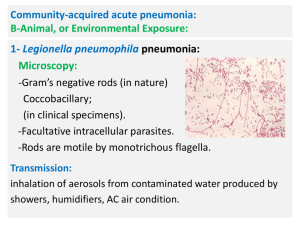
Pneumonia 2 Classification of Pneumonia: Acute Pneumonia: Community acquired: oPerson to person • Classical bacterial pneumonia • Atypical bacterial pneumonia • Viral pneumonia o Animal, or Environmental Exposure. Nosocomial acquired. Chronic Pneumonia. Animal, or Environmental Exposure: o Legionellosis. o Tularemia. o Plague. o Q fever. o Anthrax. Legionnaires' disease ( legionellosis) History: Legionnaires' disease was diagnosed for the first time in 1976 in Philadelphia among attendees of a Legionnaires' convention held in a hotel, 182 attendees contracted the disease and 29 of them died. It had caused several outbreaks. The last one was in November 12 2014 in Portugal , 302 people have been hospitalized and 7 died. • Causative agent: Legionella pneumophila. • Microscopy: - Gram’s negative rod in nature, coccobacilli in clinical specimens. - Facultative intracellular parasites. - Rods are motile by monotrichous flagella. Transmission: o Inhalation of contaminated water aerosols from showers, humidifiers, air condition…..It lives inside the free living protozoa. o No person to person transmission. o It had caused several outbreaks as well as sporadic cases and nosocomial infections. N Pathogenesis: - Engulfment by alveolar macrophages. - Inhibition of phagosome-lysosome fusion. - Replication inside the microphages until it ruptures. - Monocytic and neutrophils infiltration of alveoli; TNF-α, and INF-γ production. - Alveolitis (consolidation) and micro-abscess and cavity formation. - Bronchi are not affected. N Laboratory diagnosis: -Staining of specimens (sputum, bronchial aspirate) by gram stain and Giemsa stain. -Cultured on buffered charcoal yeast extract agar (BCYE; Enriched media: cysteine, iron) for 3- 5 days. -Rapid identification: Immunofluorescent microscopy. PCR. N Pneumonic Tularemia (granulomatous infection): • Causative agent: Francisella tularensis. • Gram negative capsulated coccobacilli with. Facultative intracellular parasite. Obligate aerobic bacteria. Transmission: from animals (rabbit, birds) to man (zoonosis) .Highly infectious. • Arthropods bite; vector (ticks, mites). • Skin penetration; handling infected animal tissues. • Inhalation of infectious aerosols. • No person – person transmission. N Pathogenesis and clinical presentation: N Clinical presentations: • Ulceroglandular tularemia: (the most common presentation). Infection of skin macrophage; ulcerative papule at the site of bite or entry; transmitted to regional lymph nodes; lymphadenitis. • Hematogenous dissemination: to the lungs. liver, spleen, bone marrow. • Pneumonic tularemia: By inhalation or blood dissemination. Infection of alveolar macrophage; granuloma in the lung. Laboratory Diagnosis: Cultured on buffered charcoal yeast extract agar (BCYE) (Enriched media: cysteine, iron). N Pneumonic Plague • Causative agent: Yersinia pestis. Gram negative coccobacilli. In sputum: Gram negative bipolar-stained (safety pin appearance). • Virulence factors: o Capsular antiphagocytic antigens: F1, V, and W. o Lipopolysaccharide (LPS) endotoxin. o Plasminogen activator: degrades fibrin. Transmission: • Vector-borne: insect bite (fleas) from rats. • Skin penetration. • Person-to-person: inhalation of droplets. N Infective dose: 100-500 cells. Incubation: 2-8 days. Three clinical presentations: • Primary: Bubonic plague: Swollen tender regional lymph node (buboes); lymphadenitis (hemorrhagic necrosis). • Septicemic plague: DIC, purpura and ecchymosis. • Pneumonic plague: (Bronchopneumonia): o Primary: Inhalation of droplets. o Secondary: Hematogenous spread. N Black death: ischemic lesion + cyanosis Treatment of Plague: • Pneumonic plague should be treated within 24 hours of appearance of symptoms, (mortality rate approaches100%). Inhalation anthrax: Wool sorter's disease: • Causative agent: Bacillus anthracis Gram positive aerobic spore-forming bacilli. • Transmission: inhalation of spores. Clinical presentation of inhalation anthrax: Inhalation anthrax; hemorrhagic mediastinal lymphadenitis: not a true pneumonia: alveolar macrophages transfer the spores to the mediastinal and peribronchial lymph nodes. Anthrax meningitis; in 50% of inhalation cases; extensive hemorrhage in the leptomeninges; darkred appearance on autopsy “Cardinal’s cap” . Treatment: -Only if multiple intravenous antibiotics and passive vaccine administered prophylactically after spore exposure. Hospital-acquired Pneumonia (Nosocomial) Nosocomial pneumonia: pneumonia acquired during or after hospitalization (at least 72 hour after admission) Who are at Risk? • Patients on mechanical ventilation (ICU). • Immunocompromised patients. • Other factors: malnutrition, heart and lung diseases. Causative agents: Aspiration of oropharyngeal and GIT flora & hospital bacteria: methicillin resistant S. aureus (MRSA), Pseudomonas, Enterobacter, Klebsiella, Serratia, VRE and Acinetobacter (person-to person). Chronic Pneumonias (coccidioidomycosis, histoplasmosis) Chronic granulomatous pneumonia: o Bacterial granulomatous pneumonia Mycobacterium tuberculosis. • Acid-fast bacilli (Mycolic acid waxy capsule). • Cultured on Lowenstein-Jensen agar. • Stained by Z.N stain. • Fungal granulomatous pneumonia: Endemic in America. • Coccidioidomycosis. • Histoplasmosis. • Blastomycosis. • Paracoccidioidomycosis Coccidioidomycosis: Caused by dimorphic fungi :Coccidioides immitis. • In the environment; they are molds with hyphae and arthroconidia (the infective stage). • In the tissues, a large structure called spherule filled with endospores (the diagnostic stage). Pathogenesis and tissue damage: - Arthroconidia engulfment by alveolar macrophage; spherule. - T cell mediated immunity and macrophage activation. N Clinical presentations: o Asymptomatic or mild flu like illness. o Acute pulmonary infection; fever, dry cough and chest pain (self-limited illness). o Chronic pulmonary infection with cavitation; in a small number of people. o Chronic meningitis. o Disseminated infection: in cell-mediated immune deficiencies (e.g. AIDS): cutaneous or systemic infection. Histoplasmosis: • Causative agent: the dimorphic fungus Histoplasma capsulatum (non-capsulated). • Pathogenesis and tissue damage: -Inhalation of microconidia (infective stage); engulfed by alveolar macrophage. -Transferred into yeast form (diagnostic) that modulate the phago-lysosomal pH. -T cell mediated immunity; killing of yeast by macrophage; Granuloma formation. N • Depending on pathogenic dose and T-cell mediated response: • Patchy pneumonitis. • Mediastinal lymphadenopathy • Chronic cavitary pulmonary histoplasmosis, in patients with chronic obstructive pulmonary disease (COPD). • Acute disseminated histoplasmosis: in immunocompromised: hepatosplenomegaly, mucus membrane ulcers, sepsis, and DIC. N Diagnosis: Microbiology Lab: Tuberculate macroconidia. Histology Lab: Macrophage with yeast cells. Fungal Pneumonia in AIDS patients • B - Cryptococcosis • A - Pneumocystis pneumonia: (The most common). -Caused by Pneumocystis jiroveci (P.carinii). -Yeast lacking ergosterol in cell membrane and so can not be treated by amphotericin. -Encysted forms infects alveoli; exudate; blocks gas exchange. -Treatment: Sulfamethoxazole and trimethoprim. Cysts of Pneumocystis carinii ; Sliver stain. N B- Cryptococcosis: Causative agents: Cryptococcus neoformans. -Yeast transmitted to man from birds (pigeon). Capsulated microbe. -Pneumonia and meningitis in Immunocompromised host. The Budding capsulated yeast Cryptococcus neoformans as shown in India ink wet mount .