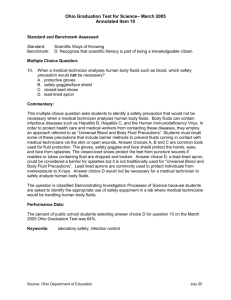
Fluids_and_Electrolytes[1][1]
advertisement
![Fluids_and_Electrolytes[1][1]](http://s3.studylib.net/store/data/009602181_1-340b41f5555e667c0a69d06db7449fa2-768x994.png)
Fluids and Electrolytes David A. Listman, MD St. Barnabas Hospital Pediatric Emergency Medicine Goals and Objectives Understand where fluid and salts are in body Understand and be able to order maintenance fluids Deficit fluids Be familiar with causes and treatment of hypo/ hyper- natremia Provide fluids to patients in special circumstances Body Fluid Composition Total body water (TBW) Intracellular fluid 75-80% of body weight at birth 60% of body weight after 1 year 2/3 of TBW or about 40% body weight Extracellular fluid 1/3 of TBW or about 20% body weight ¾ Interstitial fluid ¼ Plasma Need for Fluid Therapy Maintenance of fluids in patients with insufficient intake (i.e.. NPO) Replacement of already diminished fluid volume (i.e.. dehydration, trauma) Replace ongoing losses (i.e.. GI, renal) Maintenance Fluids Replacement of insensible losses due to heat dissipation Replacement of Urinary Losses Maintenance water needs are related to caloric requirement Maintenance Fluids Caloric requirement 100 kcal/kg/24hr up to 10 kg 1000 kcal + 50 kcal/kg/24hr per kg over 10 up to 20 1500 kcal + 20 kcal/kg/24 hr per kg over 20 Maintenance Fluids Fluid requirement 40 ml/100 kcal/ 24 hr to replace insensible losses 60 ml/100 kcal/ 24 hr to replace urine losses 100 ml/ 100 kcal/ 24 hours total SO: Maintenance Fluids Caloric requirement 100 kcal/kg/24hr up to 10 kg 1000 kcal + 50 kcal/kg/24hr per kg over 10 up to 20 1500 kcal + 20 kcal/kg/24 hr per kg over 20 Maintenance Fluids Fluid requirement 100 ml/kg/24hr up to 10 kg 1000 ml + 50 ml/kg/24hr per kg over 10 up to 20 1500 ml + 20 ml/kg/24 hr per kg over 20 Maintenance Fluids Fluid requirement 100/ 50/ 20 Divided by 24 hours (or 25) 4 / 2/ 1 (cc’s per hour) Maintenance Fluids Few examples: 8 kg 8 x 100 = 800 cc’s/ day 800 / 24 = 33.3 cc’s/ hr or 8 x 4 = 32 cc’s/ hr Maintenance Fluids Few examples: 18 kg 10 x 100 = 1000 8 x 50 = 400 1000 + 400 = 1,400 cc’s/ day 1,400 / 24 = 58.3 cc’s/ hr or 10 x 4 = 40 40 + 16 = 56 cc’s/ hr 8 x 2 = 16 Maintenance Fluids Few examples: 28 kg 10 x 100 = 1000 10 x 50 = 500 8 x 20 = 160 1000 + 500 + 160 = 1,660 cc’s/ day 1,660 / 24 = 69.2 cc’s/ hr or 10 x 4 = 40 40 + 20 + 8 = 68 cc’s/ hr 10 x 2 = 20 8x1=8 Maintenance fluids We’ve got the water, do we need anything else? Is it necessary to replace electrolytes? Recent data shows significant risk of hyponatremia in hospitalized patients Hyponatremia can lead to fluid shift into cells causing cellular (and cerebral) edema Maintenance fluids Daily sodium requirement 2-4 meq / kg / day Daily Potassium requirement 1-2 meq / kg / day This is a flat need per kilo and does not decrease as water needs do Maintenance fluids- sodium This is a flat need per kilo and does not decrease as water needs do So As volume required goes down, sodium needed per liter goes up Maintenance fluids- sodium Some examples- 10 kg child needs 20-40 meq Na+ per day 10 kg child needs 1000 cc’s per day 20-40 meq/ liter 20 kg child needs 40-80 meq Na+ per day 20 kg child needs 1500 cc’s per day 26-53 meq/ liter 50 kg child needs 100-200 meq Na+ per day 50 kg child needs 1800 cc’s per day 55-110 meq/liter Sodium concentrations Normal saline (0.9% NaCl/L) 154 mEq Na+/L 1/2 normal saline (0.45% NaCl/L) 77 mEq Na+/L 1/3 normal saline (0.33% NaCl/L) 57 mEq Na+/L 1/4normal saline (0.2% NaCl/L) 34 mEq Na+/L Ringer’s lactate 130 mEq Na+/L (Contains 4 mEq K+, 109 mEq Cl-, 28 mEq bicarb equivalent all/Liter, and 3 mg/dl of Ca++) What else goes in it? Dextrose 5% dextrose is insufficient to nourish a patient To spare catabolism of glycogen and protein What else goes in it? Potassium Daily requirement 1-2 meq/kg/day Need for Fluid Therapy Maintenance of fluids in patients with insufficient intake (i.e.. NPO) Replacement of already diminished fluid volume or deficit (i.e.. dehydration, trauma) Replace ongoing losses (i.e.. GI, renal) Treatment of volume loss Decrease in extracellular fluid Initial treatment- rapid expansion of ECF Bolus of isotonic fluid (i.e.. NS or LR) Should not include dextrose Repeat bolus as necessary to improve perfusion Replacement of deficit Continue maintenance Frequent reevaluation of Vital sign Electrolytes Urine output and urine specific gravity Treatment of volume loss Decrease in extracellular fluid Initial treatment- rapid expansion of ECF Bolus of isotonic fluid (i.e.. NS or LR) Repeat bolus as necessary to improve perfusion Replacement of deficit Continue maintenance Frequent reevaluation of Vital sign Electrolytes Urine output and urine specific gravity Estimate of Fluid Deficit Subtract pre-illness weight - current weight Calculate using current weight and % dehydration Pre-illness wt (kg) = Current wt (kg) 100 100 - % estimated dehydration Current Weight x % dehydration (slightly underestimates) Estimate of Dehydration Skin Turgor ↓,Tenting Oral Mucosa Tears Fontanelle Heart Rate Blood Pressure Urine OP CNS/ LOC Pulse Quality Skin Mild Moderate Severe Sl Dry Sl ↓ Normal/ Flat Normal/ Sl ↑ Normal Mild Oliguria Very Dry Absent Depressed ↑ Normal/ Sl ↓ Oliguria Irritable/Listless Rapid Cool/ Pale Parched Absent Sunken Normal/Elastic ↓ Alert/ Responsive Full Warm/ Pink Very Marked Tachycardia ↓ Oliguria/ Anuria Minimal/Nonresponsive Rapid/ weak Cool Estimate of Dehydration Mild Moderate Severe <1yr 5% 10% 15% Older 3% 6% 9% Replacement of Deficit Deficit volume Replace ½ over 1st 8 hours Replace ½ over next 16 hours Don’t forget maintenance fluid Replacement of Deficit Example 16 kg child 10% dehydrated Bolus(es) normal saline 20 ml/kg rapidly Maintenance 1,000 + 300= 1,300 / 24 = 54cc/hr Deficit 1,600 ml 800 over 1st 8 hours=100ml /hr 800 over next 16 hours = 50ml /hr Total 154 ml /hr x 8 hours then 104 ml/hr x16 hours Not well approximated by 1 ½ maintenance Need for Fluid Therapy Maintenance of fluids in patients with insufficient intake (i.e.. NPO) Replacement of already diminished fluid volume or deficit (i.e.. dehydration, trauma) Replace ongoing losses (i.e.. GI, renal) Ongoing losses Continued loss in excess of normal maintenance GI loss- vomit/ diarrhea Surgical drains/ NG tube Increased insensible losses- fever Increased urine output Ongoing losses Continued loss in excess of normal maintenance Volume can often be measured NG output Stool Urine Type of fluid needed for replacement Can be measured Can be estimated Oral Rehydration Better than IV if tolerated What makes a good oral rehydration fluid? Proper balance of Na+ and glucose Na+/glucose co-transporter in intestine non ATP dependant Water follows passively Oral Rehydration What makes a good oral rehydration fluid? Proper balance of Na+ and glucose Na+/glucose co-transporter in intestine non ATP dependant 1 : 1 osmolar ratio Na+ 90 meq/l, glucose 111meq/l (2% solution) Some K+ to prevent Hypokalemia Oral Rehydration What makes a good oral rehydration fluid? MMWR November 21, 2003 / 52(RR16);1-16 Oral Rehydration Mild to moderate dehydration Deficit 50-100 ml of ORS/kg body weight during 2-4 hours Maintenance100 ml ORS/kg per day limited volumes of fluid (e.g., 5 mL or 1 teaspoon) should be offered at first, with the amount gradually increased as tolerated. Hypo/ Hypernatremia More to do with water than salt status (usually) Hyponatremia free water excess Hypernatremia Free water deficit Hyponatremia Serum Na+ < 135 Common in hospitalized children Kidneys unable to dilute urine and excrete free water Hyponatremia Measure serum Osm to confirm low serum Osm before aggressive treatment Normal or high serum Osm with pseudohyponatremia Hyperglycemia Hyperlipidemia Hyperproteinemia Hyponatremia True hyponatremia causes influx of water into cells Cellular swelling Cerebral edema Exacerbated by hypoxia Hyponatremia Symptoms Headache, nausea, vomit, behavioral changes Seizures, resp arrest, dilated pupils, decorticate posturing Hyponatremia Causes of SIADH CNS Pulmonary Meningitis CNS neoplasm Hydrocephalus Pneumonia Asthma TB Positive Pressure Ventilation Pneumothorax Drugs Vincristine, cyclophosphamide Carbamazepine Hyponatremia Post-operative Multi-factorial Volume depletion Stress ADH Hypotonic fluids Hyponatremia Water intoxication Newborns Fed dilute formula or water supplement Decreased ability to maximally concentrate urine Hyponatremia- treatment If neurologic signs/ seizure Hypertonic 3% saline (514 meq/l) 1 ml/kg/hr should raise Na+ by 1 meq/l Goals Raise Na+ by 1 meq/hr until Symptoms resolve Serum Na+ has risen 20-25 meq/l Serum Na+ 125-130 meq/l or or Hyponatremia- treatment Asymptomatic Restrict free water intake Avoid hypotonic fluids Hyponatremia Recent evidence suggests use of isotonic rather than hypotonic fluids in post-op, gastroenteritis prevents hyponatremia. Hypernatremia Serum Na+ >145 meq/l Debilitated patients Neurologically impaired patients Ineffective breastfeeding Inability to access sufficient free water Inability to maximally concentrate urine Hypernatremia Clinical manifestations Water moves from intracellular to extracellular space Maintenance of ECF volume so classic signs of volume depletion are absent Agitation, irritability, coma Hypernatremia Clinical manifestations Water moves from intracellular to extracellular space Cell shrinkage Brain cell volume decreases If acute and rapid can lead to Intracranial hemorrhage Venous sinus thrombosis Over short time brain cells increase intracellular Na+, K+, amino acids, unmeasured organic substances Not easily decreased so rapid rehydration will cause cerebral edema Hypernatremia Treatment Correct serum Na+ and water deficit Free water deficit = 4ml x lean body weight (kg) x (serum Na+ – desired Na+ ) Add maintenance fluid and correct slowly At least 48-72 hours if serum Na+ > 170 Various Causes of Volume Loss Trauma- when is it time for blood 20 ml’s/kg NS or LR x 2 Then whole blood or PRBC’s Diabetes IDDM what is the cause and presentation Not enough insulin produced Break down of fats and protein in response to low insulin levels How does it present? What are the fluid and electrolyte abnormalities? Glucose Sodium Potassium Phos pH Diabetes Very hyperosmolar Pseudohyponatremia Initial Boluses to restore intravascular volume Slow deficit replacement to prevent cerebral edema Constant infusion of insulin regardless of blood glucose Add IV glucose if necessary Diabetes • Usual fluids – – Initial bolus(es) of Normal Saline After 1st hour • • • Insulin infusion usually 0.1 units / kg/ hour ½ NS with 20KCL and 20 K Phos at maintenance plus slow deficit replacemement Once sugar falls – 2 bags • • • • ½ NS with 20KCL and 20 K Phos D10 ½ NS with 20KCL and 20 K Phos Total of these 2 infusions to equal maintenance plus slow deficit replacement Can titrate to provide anywhere from no dextrose to D10 without changing electrolytes depending on the CBG’s Burns Tremendous fluid losses Parkland formula 4 ml/ kg/ % BSA burns (2nd and 3rd degree)/ 24 hours half over first 8 hours ½ over next 16 hours in addition to maintenance Summary Provide water, sodium, glucose and potassium to patients who have a variety of disturbances of fluid and sodium balance