Delirium PPT
advertisement

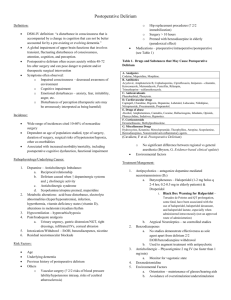
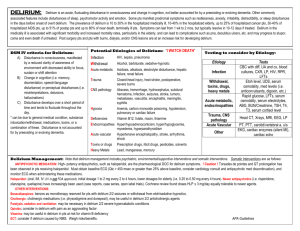
Delirium Lea C. Watson, MD, MPH Robert Wood Johnson Clinical Scholar UNC Department of Psychiatry Nurse pages med student: “..Mr. Smith pulled out his NG tube and can’t seem to sit still. Last night after his surgery he was fine, reading the paper and talking to his family…today I don’t even think he knows where he is… can you come see him?” Med student says: “…sounds like DELIRIUM- good thing you called- I’ll be right there.” Delirium • A sudden and significant decline in mental functioning not better accounted for by a preexisting or evolving dementia • Disturbance of consciousness with reduced ability to focus, sustain, and shift attention 4 major causes • • • • Underlying medical condition Substance intoxication Substance withdrawal Combination of any or all of these Patients at highest risk • Elderly – >80 years – demented – multiple meds • • • • Post-cardiac surgery Burns Drug withdrawal AIDS Prevalence • • • • Hospitalized medically ill Hospitalized elderly Postoperative patients Near-death terminal patients 10-30% 10-40% up to 50% up to 80% Clinical features Prodrome Fluctuating course Attentional deficits Arousal /psychomotor disturbance Impaired cognition Sleep-wake disturbance Altered perceptions Affective disturbances Prodrome • Restlessness • Anxiety • Sleep disturbance Fluctuating course • Develops over a short period (hours to days) • Symptoms fluctuate during the course of the day (SYMPTOMS WAX AND WANE) – – – – – Levels of consciousness Orientation Agitation Short-term memory Hallucinations Attentional deficits • Easily distracted by the environment • May be able to focus initially, but will not be able to sustain or shift attention Arousal/psychomotor disturbance • Hyperactive (agitated, hyperalert) • Hypoactive (lethargic, hypoalert) • Mixed Impaired cognition • • • • Memory Deficits Language Disturbance Disorganized thinking Disorientation – Time of day, date, place, situation, others, self Sleep-wake disturbance • Fragmented throughout 24-hour period • Reversal of normal cycle Altered perceptions • Illusions • Hallucinations - Visual (most common) - Auditory - Tactile, Gustatory, Olfactory • Delusions Affective disturbance • • • • • • Anxiety / fear Depression Irritability Apathy Euphoria Lability Duration • Typically, symptoms resolve in 10-12 days - may last up to 2 months • Dependent on underlying problem and management Outcome • May progress to stupor, coma, seizures or death, particularly if untreated • Increased risk for postoperative complications, longer postoperative recuperation, longer hospital stays, longterm disability Outcome • Elderly patients 22-76% chance of dying during that hospitalization • Several studies suggest that up to 25% of all patients with delirium die within 6 months Causes: “I WATCH DEATH” • • • • • • I nfections W ithdrawal A cute metabolic T rauma C NS pathology H ypoxia • • • • • D eficiencies E ndocrinopathies A cute vascular T oxins or drugs H eavy metals “I WATCH DEATH” • Infections: encephalitis, meningitis, sepsis • Withdrawal: ETOH, sedative-hypnotics, barbiturates • Acute metabolic: acid-base, electrolytes, liver or renal failure • Trauma: brain injury, burns “I WATCH DEATH” • CNS pathology: hemorrhage, seizures, stroke, tumor (don’t forget metastases) • Hypoxia: CO poisoning, hypoxia, pulmonary or cardiac failure, anemia • Deficiencies: thiamine, niacin, B12 • Endocrinopathies: hyper- or hypoadrenocortisolism, hyper- or hypoglycemia “I WATCH DEATH” • • Acute vascular: hypertensive encephalopthy and shock Toxins or drugs: pesticides, solvents, medications, (many!) drugs of abuse – • anticholinergics, narcotic analgesics, sedatives Heavy metals: lead, manganese, mercury Drugs of abuse • • • • • • Alcohol Amphetamines Cannabis Cocaine Hallucinogens Inhalants • • • • Opiates Phencyclidine (PCP) Sedatives Hypnotics Causes • 44% estimated to have 2 or more etiologies Workup • • • • • History Interview- also with family, if available Physical, cognitive, and neurological exam Vital signs, fluid status Review of medical record – Anesthesia and medication record review temporal correlation? Mini-mental state exam • Tests orientation, short-term memory, attention, concentration, constructional ability • 30 points is perfect score • < 20 points suggestive of problem • Not helpful without knowing baseline Workup • • • • • Electrolytes CBC EKG CXR EEG- not usually necessary Workup • • • • • Arterial blood gas or Oxygen saturation Urinalysis +/- Culture and sensitivity Urine drug screen Blood alcohol Serum drug levels (digoxin, theophylline, phenobarbital, cyclosporin, lithium, etc) Workup • • • • • Arterial blood gas or Oxygen saturation Urinalysis +/- Culture and sensitivity Urine drug screen Blood alcohol Serum drug levels (digoxin, theophylline, phenobarbital, cyclosporin, lithium, etc) Workup • Consider: - Heavy metals - Lupus workup - Urinary porphyrins Management • Identify and treat the underlying etiology • Increase observation and monitoring – vital signs, fluid intake and output, oxygenation, safety • Discontinue or minimize dosing of nonessential medications • Coordinate with other physicians and providers Management • Monitor and assure safety of patient and staff - suicidality and violence potential - fall & wandering risk - need for a sitter - remove potentially dangerous items from the environment - restrain when other means not effective Management • Assess individual and family psychosocial characteristics • Establish and maintain an alliance with the family and other clinicians • Educate the family – temporary and part of a medical condition – not “crazy” • Provide post-delirium education and processing for patient Management • Environmental interventions - “Timelessness” - Sensory impairment (vision, hearing) - Orientation cues - Family members - Frequent reorientation - Nightlights Management • Pharmacologic management of agitation - Low doses of high potency neuroleptics (i.e. haloperidol) – po, im or iv - Atypical antipsychotics (risperidone) - Inapsine (more sedating with more rapid onset than haloperidol – im or iv only – monitor for hypotension) Management • Haloperidol and inapsine have been associated with torsade de pointes and sudden death by lengthening the QT interval; avoid or monitor by telemetry if corrected QT interval is greater than 450 msec or greater than 25% from a previous EKG Management • Benzodiazepines - Treatment of choice for delirium due to benzodiazepine or alcohol withdrawal Management • Benzodiazepines - May worsen confusion in delirium - Behavioral disinhibition, amnesia, ataxia, respiratory depression - Contraindicated in delirium due to hepatic encephalopathy What we see…common cases • Homeless male, hx. ETOH abuse, 2 days post-op • 82 year-old women with UTI • Burn victim after multiple med changes • Mildly demented 71 year-old after hip replacement Summary • Delirium is common and is often a harbinger of death- especially in vulnerable populations • It is a sudden change in mental status, with a fluctuating course, marked by decreased attention • It is caused by underlying medical problems, drug intoxication/withdrawal, or a combination • Recognizing delirium and searching for the cause can save the patient’s life