Infection Control - ClinicalLabPracticumHSII
advertisement

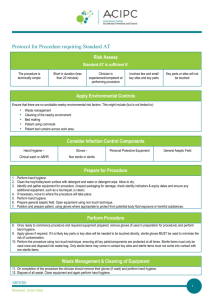
Infection Control Practicum in HS II – Medical Assisting Standard Precautions • Sometimes called “Universal Precautions” • Used to break the chain of infection • Pathogens spread by blood and body fluids – Hepatitis B (HBV) – Human Immunodeficiency Virus (HIV) OSHA • Passed regulations in 1991 requiring all healthcare facility employers to – Determine which employees will have exposure to blood and body fluids – Provide HBV vaccine free to employees with exposure risk (or signed refusal) – Provide personal protective equipment (PPE) such as gloves, gowns, lab coats, masks, and face shields OSHA – Provide adequate handwashing facilities and supplies – Ensure clean and safe work environment – Follow decontamination protocol for contaminated surfaces – Dispose of infectious wastes correctly – No eating, drinking, smoking, handling contact lenses, applying lip balm, etc. in risk area OSHA – Provide color-coded containers labeled for sharps and other infectious wastes – Post signs in work areas where there is exposure risk – Provide medical evaluation and follow-up for employees who’ve had an exposure incident – Provided training about the regulations to all employees at no cost during working hours Standard Precautions • Rules developed by the CDC and FDA 1. All body fluids should be considered potentially infectious 2. All patients should be considered potential sources of infection 3. Wash hands before AND after any patient 4. If any surface comes in contact with blood or body fluids, wash immediately and thoroughly. Standard Precautions 5. Wash hands after removing gloves 6. Wear gloves whenever contact with blood or body fluids is possible 7. Change gloves after contact with each patient 8. Gloves should not be reused 9. Gowns should be worn during any procedure with risk of splashing blood or body fluids Standard Precautions 10. Masks and protective eyewear to be worn during procedures that may produce blood or body fluids 11. Extreme care should be taken while handling sharp objects. (Do not bend, break, or recap needles. Dispose of them in a puncture-resistant container.) 12. Spills or splashes of blood or body fluids should be wiped up immediately. Wear gloves, and use a disinfectant solution. Standard Precautions 13. Mouthpieces or resuscitation devices should be used to avoid the need for mouthto-mouth resuscitation. 14. Know the requirements for disposal of waste materials and dispose of wastes in the proper container. 15. Report any cut, injury, needle stick, or splashing of blood or body fluids immediately. Sterilizing with an Autoclave • Uses steam under pressure or gas • Destroys ALL microbes, pathogenic and nonpathogenic- including spores and viruses • Before wrapping, instruments must be cleaned • Wraps must allow for penetration of steam – Muslin – Autoclave paper – Special plastic or paper bags – Autoclave containers Sterilizing with an Autoclave • Indicators are used to ensure articles have been sterilized – Autoclave tape, sensitivity marks on bags or wraps, indicator capsules – Indicator will change appearance when sterile • Autoclave must be loaded correctly • Amount of time depends on the article to be sterilized – usually 15 – 30 minutes • If wrap becomes torn or wet, it is contaminated • Expires in 30 days Disinfection • Chemicals are frequently used for aseptic control • They do NOT kill spores & viruses so it’s NOT sterilization • Used to disinfect instruments that don’t penetrate human body tissue: – Dental instruments – Percussion instruments – thermometers Disinfection • Examples – – 90% isopropyl alcohol – Formaldehyde – alcohol – 10% bleach solution – Lysol – Zephiran • Boiling water disinfects but does not sterilize • Satisfactory for home care where instruments/supplies used for one person only • Usually 15 – 30 minutes Disinfection • Ultrasonic unit – used in dental and medical offices to disinfect • Uses sound waves to produce millions of microscopic bubbles – Cavitation – bubbles hit instrument and explode, driving cleaning solution into article Sterile Technique - Principles • Surgical Asepsis – procedures that keep an object or area free from living organisms • Sterile – free from all organisms, including spores and viruses • Contaminated – organisms/pathogens are present – A clean, uncluttered work area necessary when working with sterile supplies Sterile Technique - Principles • Sterile field – sterile area – never reach across a sterile field – reach in from the side • Never turn your back on a sterile field • 2 inch border of sterile field is considered contaminated • Common techniques – Drop technique – Mitten technique – Transfer forceps Sterile Technique - Principles • Keep sterile field dry (pathogens travel through wet) and be careful when pouring fluids • Be sure sterile field is open and ready before putting on sterile gloves • Sterile gloves are contaminated on the inside – once on, keep hands away from body and above waist • When in doubt, consider it contaminated Opening Sterile Packages • Check to be sure the sterile package has not expired • Open the distal end and pull it away from you, reaching around the package, not across • Open the sides without touching the inside wrapper • Pull the bottom down toward you • Drop technique • Mitten technique • Transfer forceps