UNIT 32 HELENS
advertisement

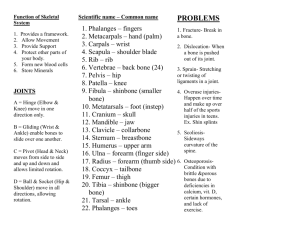
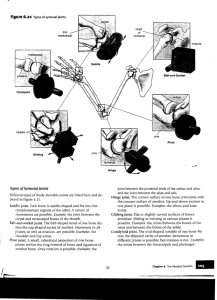
BTEC National Diploma Health Studies Unit 32 Mobility and Exercise for Health and Social Care Assignment Brief 1- Bones and Joints Tutor Name: Matthew Hopton Student Name: _Helen Pitchers Assignment Commencement Date: 15th September 2008 Assignment Completion Date: 12th December 2008 Assignment 1 Criteria to achieve: Pass P1x P2x P3 P4x P5 P6 Merit M1x M2 M3 Distinction D1 D2 Date Achieved Tutor Signature Actual Criteria Achieved: Criteria P1 P2 P4 M1 TASK 1 P1, M1 On the diagram of the skeleton, clearly shade the appendicular skeleton in any colour. (Do not shade the axial skeleton) Label the bones numbered 1-24. Describe how bone shape is linked to bone function in the axial and appendicular skeletons Describe the growth and repair of bones. Analyse factors affecting growth and repair including examples of common homeostatic disorders of the skeleton and joints to help you explain the effects of different influences on skeletal development TASK 2 P2 Draw a diagram of a named synovial joint. Explain the structure and function of the three main types of joints found in the body i.e. fixed, cartilaginous and freely moveable; name at least one example of each type you have explained. Identify the six different types of synovial joint found in the body Describe the functions of the main components of a synovial joint, describe at least two disorders that may affect this joint TASK 3 P4 Describe an exercise which involves a ball and socket joint and a hinge joint (other joints may also be involved) For the exercise described, name the movements involved at the joint(s) you have mentioned. Comment upon factors which affect these movements including the muscles involved. Delivery and Assessment Windows Assignment 1 Start Date Finish Date Hand In Date 15th September 2008 12th December 2008 19th January 2009 Human Skeleton Learning outcomes On completion of this unit a learner should: 1 Understand the anatomy of the musculo-skeletal system 2 Understand mechanisms of muscle contraction 3 Be able to relate balance, posture and body movement to the co-ordinated action of muscles around joints 4 Understand how common injuries and disorders of the musculo-skeletal system relate to structure and function. 1 Understand the anatomy of the musculo-skeletal system Ossification: intramembranous, endochondrial Development of skeleton: skeletal growth — lengthening of bones, closure of epiphyses, development of normal spinal curvatures (cervical, thoracic, lumbar); mineral storage, the dynamic state of bone Types of bone: histology of skeletal tissues — ligaments, tendons, cartilage, bone (compact, cancellous); structure of long bones, flat bones, bone marrow Influencing factors: genetics, age, diet, effect of weight-bearing exercise, disease Names of bones: relationship between structure, shape and function; main identifying features of — mandible and maxillae, bones of cranium, spine, girdles, limbs, chest; function of ligaments Types of joints: - moveable, eg ball and socket, hinge, gliding; synovial capsule, range of movement - immoveable, eg sutures of cranium, face, pelvis - slightly moveable — public symphysis 2 Understand mechanisms of muscle contraction Types of muscle: voluntary (skeletal); involuntary (smooth); cardiac Histological aspects: cell shape and alignment; myofibril ultrastructure — sarcomeres, actin, myosin; neuromuscular junction in voluntary muscle tissue Biochemical aspects: actin, myosin; sliding filament theory — actomyosin, calcium ions, myoglobin; aerobic and anaerobic muscle contraction, fatigue, oxygen debt and recovery Mechanical aspects: movement brought about by contraction of antagonistic muscle groups; isotonic and isometric muscle contraction; stamina, suppleness, musculo-skeletal adaptations to regular exercise 3 Be able to relate balance, posture and body movement to the coordinated action of muscles around joints Named example: one of knee, hip, shoulder, elbow Movements: all those relevant to joint chosen, eg flexion, extension, adduction, abduction, circumduction, principles of antagonistic and synergistic action Muscle groups: eg quadriceps, hamstrings, calf, spinal muscles, gluteals, pectorals, abdominals, shoulder, arm Principles of levers: parts of a lever — effort, fulcrum, load; classes of lever — first class, second class, third class; examples of levers in the body, eg nodding of head, straightening of bent arm, standing on tiptoe Proprioception: spindle receptors in tendons, joints and muscles, proprioception reflexes, balance, visual input 4 Understand how common injuries and disorders of the musculoskeletal system relate to structure and function Injuries: sprain, muscle strain, fracture, dislocation, osteoarthritis, back pain, paralysis Disorders: kyphosis, scoliosis, lordosis; osteoporosis Grading criteria To achieve a pass grade the evidence must show that the learner is able to: P1 describe the structure and development of bone and the skeleton and the factors that influence it P2 explain the structure and functioning of different types of joints P3 describe the structure and contraction of different types of muscle tissue P4 explain the role of muscle groups and the principles of levers in bringing about movement around a named moveable joint P5 explain the concept of proprioception in relation to maintaining balance, posture and locomotion P6 explain common injuries and disorders in relation to musculo-skeletal structure. To achieve a merit grade the evidence must show that, in addition to the pass criteria, the learner is able to: M1 explain the effect of different influencing factors on skeletal Development M2 compare the characteristics of two types of muscle in relation to their structure and functions in the body M3 explain interactions of muscle groups in maintaining posture and in locomotion of the whole body. To achieve a distinction grade the evidence must show that, in addition to the pass and merit criteria, the learner is able to: D1 analyse how musculo-skeletal functioning is affected by exercise and how exercise helps maintain healthy functioning of the musculo-skeletal system D2 use knowledge of the structure and functioning of the musculo-skeletal system to analyse the impact of common musculo-skeletal disorders on mobility and locomotion. In this assignment I am going to describe how bone shaped is linked to bone function in the axial skeleton. I am also going to discuss the repair and growth of bones as well as stating the main joints in the body. Axial bones http://www.aclasta.co.nz/images/aclasta_skeleton_1.gif The craniumThe cranium is comprised of twenty two interlocking cranial and facial bones. The cranium is there to protect the brain. The cranial plates and bones are held together by joints, the joins do not allow movement apart from the jaw bone and mandible. The Spine The vertebral column also known as the spine has thirty three specialized bones, these are called vertebrae. These provide form for the rest of the body and protect the spinal cord. There are twelve thoracic vertebrae, forming from the back of the ribcage. The sternumThe sternum also known as the breastbone is there as a organ protector. It defends the heart, lungs and bits of your major arteries form external forces. The sternum provides stability to the ribs that are attached to it. The ribsThe ribs are flat bones which form a protective shield around your internal organs. There are a total of twenty four ribs, twelve on each side of the body. The first set of seven ribs are called true ribs. These connect in the back to the spine and connect in the front to the sternum. The next ribs are called false ribs which connect to the back of the spine. The last ones are called floating ribs, and these two pairs of ribs are attached to the spine like all the others except these ribs ‘float’ in front without being attached to the sternum or any other rib. Axial bones are named because they form the axis of the body. They are associated with the general nervous system and protect delicate organs such as the heart and the brain. Appendicular bones basically connect to the axial bones. These bones are not designed for protection there function is movement. Appendicular bones The shoulder bone – The shoulder bone makes a girdle to connect your arms to the sternum and rib cage for stability and support. Everyone has two clavicles known as collar bones that attach on one end of the breast plate and on the other end. This supports the shoulder blades. The shoulder blades provide points of contact and attachment for many muscles and the bone of each upper arm. Arm bone and hand bone – The arm is basically broke up into three mains parts which are the upper arm, the lower arm and the hand. The upper arm is a long bone. Each hand has twenty seven bones, eight carpal bones that make up the wrist, five metacarpal bones that extend the length of your palm, and fourteen phalanges that form four fingers with three bones each along with a single two-boned thumb. The pelvic girdle – The pelvic girdle supports a person when they sit down as that is where all their weight immediately goes. The hip bones protect lower organs such as the bladder and for women the opening in the centre of the girdle must be big enough for child birth. Bones of the thigh, leg and foot – The bone which connects the pelvic girdle to the lower leg in the thigh is a bone called the femur. This is the longest and the strongest bone in the body. The femur connects through the knee joint to the shin bone. Slightly smaller than the tibia is the other bone in the leg which is called the fibula. This is responsible for muscular connections, while tibia makes sure your foot and your knee don’t get any farther apart from each other. Each foot has twenty six bones, seven tarsal bones that make up the ankle, five metatarsal bones that make up the body of your foot, and fourteen phalanges that form four toes with three bones each with a big toe which has two bones. The terms osteogenesis and ossification are often used to indicate the process of bone formation. Parts of the skeleton form in the first few weeks of conception. Bone development continues throughout adulthood, bone development continues for repair of fractures and for remodelling to meet lifestyles. Bones grow in length at the epiphyseal plate by a process that is similar to endochondral ossification. The cartilage in the region of the epiphyseal plate next to the epiphysis continues to grow by mitosis. Osteoblasts move and ossify the matrix to form bone. This process continues throughout childhood and the adolescence years until the cartilage growth slows and finally stops. Even though bones stop growing in length in early adulthood, they can continue to increase in thickness or diameter throughout life in response to stress from increased muscle activity or to weight. 2. Although bone is a very strong material it can break in a number of ways with enough force pushing, pulling or twisting. Some breaks include: Open fracture- Unlike closed fractures in which all portions of the broken bone remain within the skin, open fractures result in a piece of bone sticking out the skin. Complete fracture- This is when the breaks nearly into two pieces. Single fracture- This is when a bone is only damaged in one area. Spiral fracture- This occurs when the bone has been twisted past its maximum point. Almost immediately after the break, the body begins to try and put itself back together again. When a bone breaks, the fissure also severs the blood vessels running down the length of the bone. Blood leaks out of these veins and quickly forms a clot called a fracture hematoma. This helps to stabilize the bone and keep both pieces lined up for mending. The clot also cuts off the flow of blood to the jagged bone edges. Without fresh blood, these bone cells quickly die. Swelling and inflammation follow due to the work of cells removing dead and damaged tissue. Tiny blood vessels grow into the fracture hematoma to help the healing process. After a few days the fracture hematoma develops tougher tissue, transforming it into a soft callus. Cells called fibroblasts begin producing fibers of collagen, the major protein in bone and connective tissue. Chondroblasts then begin to produce a type of cartilage called fibrocartilage. This transforms the callus into a tougher fibrocartilaginous callus, which bridges the gap between the two pieces of bone. This callus generally lasts for about three weeks. Next, osteoblasts move in and produce bone cells, transforming the callus into a bone callus. This hard shell lasts three to four months, and it provides necessary protection and stability for the bone to enter the final stage of healing. At this point, the body establishes the position of the bone within the flesh, begins reabsorbing bits of dead bone, and creates a hard callus to bridge the gap between the two pieces of bone. However, this bulge of tissue needs a lot of work before the bone can take any strain. Osteoporosis is a common homeostatic disorder of the skeleton it affects the bones which makes the bone more fragile and prone to break after a minor bump or fall. These broken bones are often referred to as fragility fractures. Although fractures can occur in different parts of the body, the wrist, hip and spine are most commonly affected. Bones stop growing in length between the ages of 16 and 18, but bone density continues to increase slowly until a person is in their mid 20s. At this point the balance between bone demolition and bone construction stays stable. After the age of 35, bone loss increases very gradually as part of the natural ageing process. This bone loss becomes more rapid in women for several years following the menopause and can lead to osteoporosis and an increased risk of broken bones, especially in later life. Consequences - Having osteoporosis does not automatically mean that your bones will break, it just means that you have a bigger risk of fracture. Thin, fragile bones in themselves are not painful but the broken bones that can result, can cause pain and other problems. Osteoporosis does not generally slow or stop the healing process. Bones that break because of osteoporosis will still heal in the same way as they do in people who do not have osteoporosis, which is usually about six to eight weeks. Prevention - The older we get, the greater our risk of breaking a bone. Osteoporosis becomes more common as the density of bone decreases and bones become generally less strong and more fragile. Falling is also much more common because of poor balance and co-ordination leading to a higher risk of breaking a hip. Lifestyle changes and keeping active can help to prevent falling. Drug treatments, to strengthen bones, are available for those at highest risk of fracture. Fixed joint http://www.zimmer.com/web/enUS/images/ products/joints/knees/lps_flex_fixed_knee2.jpg A fixed joint is a joint between two bones that do not move. A good example of this is in the skull - the skull plates do not move together or against each other, but they are connected or fused. Fixed joints are also called fused joints for this reason. Cartilaginous joint - A Cartilaginous joint is a joint in the skeletal system which is connected tightly by cartilage, an example of this would be the spinal column. There are two other types of joint also, a fibrous joint that does not allow any movement what so ever such as the cranium (scull) and they synovial joint which is the most common joint in the skeletal system. http://www.healthydirect.com/medias/sys_master/8450599988759728.gif Freely moveable joint - There are four types of freely movable joints which are grouped according to the shapes of the surfaces of the adjacent bones. Ball and socket joints permit circular movement. Circular movement is the largest range of moment. The joints of the shoulder blade are an example of a ball and socket joint. The hinge joint permits back and fourth movement like the opening and closing of a door. The joints where the femur,patella, fibula, and tibia connect are example of a hinge joint. Pivot joints allow one bone to rotate around another. The joints where the humerus, radius, and ulna meet are an example of a pivot joint. Saddle joints allow one bone to slide in two directions. The thumb is an example of a saddle joint. http://www.marymount.k12.ny.us/marynet/stwbwk05/05bio/caskeletal/html / Pivot joints – Also known as rotary joints. These joints allow for rotation around an axis. There is a pivot joint near the top of your spine that allows your head to move from side to side. Hinge joints – This type of joint can open and close like a door. Your elbow is a hinge joint. Your biceps and triceps muscles are basically two people standing on opposite sides of a wall (the humerus, or upper-arm bone), each with one hand reaching over to its respective side of a door (the bones of the lower arm). The biceps "shuts" the door, by contracting and lessening the degree of the joint angle, and the triceps, when it pulls on its respective side of the door, "opens" the door, as the hinge then widens. Gliding Joints - This type of joint features two bone plates that glide against one another. The joints in your ankles and wrists are gliding joints. (Holding your forearm steady while your hand points upward and then waving side-to-side with your hand is an example of this joint's functioning.) Ball and socket joints - This is the most maneuverable type of joint. Your shoulder and your hip are both ball-and-socket joints. These joints feature a connection between one bone-end equipped with a protrusion that fits into the receptive space at the end of the other bone in the joint. These joints allow for forward motion, backward motion and circular rotation. Saddle Joints - These joints allow for two different types of movement. For instance, a saddle joint allows your thumb to move toward and away from your forefinger (as when you spread all five digits out, then bring them all together side-by-side) as well as cross over the palm of your hand toward your little finger. Conyloid joints - These joints are similar to ball-and-socket joints, just without the socket. Football is an exercise which involves a ball and socket joint and a hinge joint. http://www.hopkinsortho.org/pfps_1.gif The knee is a hinge joint held together by four ligaments. A ligament is a structure in the knee that holds the bones together and helps to control joint movement or motion. There is a ligament on each side of the knee (the collateral ligaments) and two ligaments deep inside the knee. The two ligaments inside the knee "cross" each other are called the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). Both ligaments attach on one side to the end of the thigh bone (femur) and on the other to the top of the shin bone (tibia). During activity, the ACL controls how far forward the tibia can "slide" relative to the femur: it essentially acts to prevent too much forward movement this could cause an injury during football if it went too far forward. While some degree of motion or sliding is normal and is required for knee function, too much motion may damage other structures in the knee which can lead to long term problems in some patients. For football players it is essential to try and avoid these kinds of movements as they could end up in strains, fractures and brakes. Factors which affect these are things such as: Age- Depending on a person’s age depends on how likely they are to become injured during a game of football. The older someone is the more fragile they become and more susceptible to injury. Physical fitness – If someone is not used to exercising they could do themselves a lot of damage as they are using muscles which haven’t been worked in a long period of time. If someone is physically unfit they could seriously damage themselves. Environment- Depending on where someone is could affect the out come. If someone was in the park having a friendly game of football they are less likely to get injured then they are on a football pitch. Weather can also affect things as if it is raining you are more likely to slip over. The muscles involved when playing football are: Gluteus maximus, minimus Quadriceps (Rectus Femoris, Vastus Lateralis, Vestus medialis) Hamstrings (Biceps Femoris, semimembranosus, semitendinosus) Soleus Gastrocnemius Tibialis Anterior Peroneus Longus Bibliography http://www.physioroom.com/products/knee_braces.php http://kidshealth.org/kid/htbw/muscles.html http://en.wikipedia.org/wiki/Ball_and_socket_joint