Georgia 2009: IDP Camp
advertisement
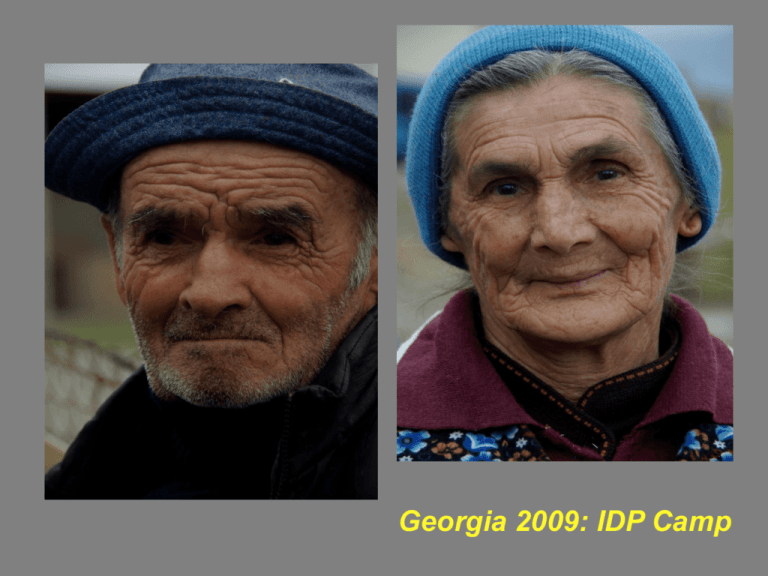
Georgia 2009: IDP Camp Aortic Regurgitation Jen McEntee, MD, MPH Etiology of Acute and Chronic Aortic Regurgitation ETIOLOGIES: Acquired - Bacterial Endocarditis, Ankylosing Spondylitis, Trauma, anorectic drugs (fenfluramine and dexfenfluramine) Congenital/Genetic - Marfan Syndrome, EhlersDanlos, Hurler, VSD, Aortic Dissection, bicuspid valve, Osteogenesis Imperfecta, Giant Cell Arteritis, Reiter’s Syndrome, Degenerative - cystic medial necrosis, myxomatous degeneration, anuloaortic ectasia Pathophysiology of Acute AR Sudden large regurgitant volume --> LV normal size and not dilated --> increase end Diastolic Volume --> decrease forward stroke volume --> tachycardia to maintain CO --> hypotension and Cardiogenic Shock and/or Pulmonary Edema Pathophysiology of Chronic AR Increased regurg vol --> increases left ventricular diastolic volume --> LV enlargement --> LV hypertrophy --> maintains stroke volume and CO Clinical Presentation & Diagnosis: Acute AR: PE: ? Murmur - most likely low-pitched early diastolic murmur and soft systolic murmur , narrow pulse pressure (2/2 to decrease systolic pressure and increase diastolic pressure) Pulmonary Edema, Cardiogenic shock, tachycardia, MI EKG - nonspecific ST and T wave changes CXR - ? Pulmonary edema, ? LV enlargement TTE - diagnostic test of choice Severe Acute AR Echo findings = Vena contracta width > 6 mm, Presence of holodiastolic flow reversal in descending thoracic/proximal abd aorta, Regurg volume >60 ml/beat, regurg fraction > 50% Further Imaging if needed Clinical Presentation of Chronic AR Chronic AR - asymptomatic for decades Sx - related to LVH, angina uncommon PE : Widened Pulse Pressure, Bounding pulses: Head Bobbing (deMusset’s sign), Traube’s sign (pistol shot pulse heard over femoral artery), Quincke’s pulses (cap pulsations in fingertips or lips), Mueller’s sign (uvular sys pulsations), Becker’s sign (visible pulsations of ret arteries and pupils), Rosenbach’s and Gerhard’s sign (pulsations over liver and spleen respectively) High -pitched, decrescendo, blowing Diastolic Murmur, Systolic Murmur, Austin Flint murmur Diagnosis of Chronic AR EKG - LVH with concurrent ST and T wave changes, LAH, Left Axis CXR - cardiomegaly, ? Widened mediastinum ECHO - ECHO - ECHO - ECHO - ECHO - ECHO Cardiac Catheterization - w/ aortic root angiography and LV pressure measurement when TTE inconclusive or discordant with clinical findings and before AVR in pts at risk for CAD. TREATMENT: SURGERY VS MEDICAL MANAGEMENT J McEntee Management for Acute AR Medical Emergency Surgery - AVR If delay in surgery - venodilators and +inotrope Treat underlying etiology - endocarditis Management of Chronic AR Serial Exams: Asymptomatic mild to moderate AR --> after first visit if chronic AR is uncertain repeat TTE and PE in 2-3 months Asymptomatic mild with no LV dilatation and EF >55% --> Yearly PE --> TTE q 2-3 years Asymptomatic Severe AR with EF > 55% but LV EDD > 70 or LV ESD > 50 --> repeat TTE q 6-12 months Symptomatic and EF < 25% or EDD >60 - ??? Surgical Management - AVR Class I - Evidence supports AVR Symptomatic w/ Severe AR Asymptomatic w/ Severe AR and EF <50% Severe AR and undergoing CABG or other valve repair Class II IIa (reasonable)- Asymptomatic Severe AR w/ normal EF but w/ LVD (EDD >75 mm or ESD > 55mm) IIb (may be considered) - moderate AR while undergoing surgery on ascending aorta or CABG, Asymptomatic Severe AR w/ normal EF but w/ LVD (EDD >70 mm or ESD > 50mm) and exercise intolerance. Copyright ©2008 American College of Cardiology Foundation. Restrictions may apply. Medical Therapy: vasodilators Class I (indicated) - Severe AR with Symptoms or EF < 50% but surgery not recommended Class IIa (reasonable) - short-term tx to improve cardiac function prior to AVR in pts with severe AR with Symptoms and EF < 50% Class IIb (may be considered) - long-term tx asymptomatic severe AR with normal EF but LVD Post-op Monitoring and Prognosis Post-op Monitoring TTE prior to pt DC and decreased LVD--> follow clinically 6-12 months Persistent LVD --> treat with beta blockers and ACE-I --> re-evaluation with TTE and clinically in 6-12 months Prognosis Good predictor is decrease in LV EDD (80% reduction in 10-14 days post-op) Our Pt AORTIC VALVE REPLACEMENT WITH BIOPROSTHETIC VALVE AORTA GRAFT Post op complications with dev of atrial flutter --> cardioverted to SR Repeat TTE --> POINTS TO PONDER Indications for surgery - Symptoms, EF <50, LV EDD > 75 mm, LV ESD > 55, BB contraindicated in acute and severe AR (even though treatment in Aortic Dissection) Pt’s can always surprise you - the H and P is the most important art of medicine. References G. Hicks Jr. and H.T. Massey. Update on indications for surgery in aortic insufficiency. Current Opinion Cardiology 2002, 17:172-178. M. Enriquez-Sarano and A.J Tajik. Aortic Regurgitation. The New England Journal of Medicine. October 7, 2004, 351:15; 1539-1546. F. Kerendi, R. Guyton, J.D. Vega, P.D. Kilgo, and E.P. Chen. Early Results of Valve-Sparing Aortic Root Replacement in High-Risk Clinical Scenarios. Ann Thorac Surg 2010; 89; 471-478. Bonow et al. ACC/AHA VHD Guidelines: 2008 Focused Update Incorporated. JACC Vol. 52, No 13, 2008. September 23, 2008: e 1-e142. UTD: Auscultation of Heart Murmurs,