Placebo
advertisement
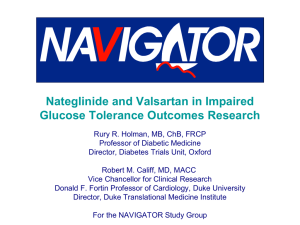
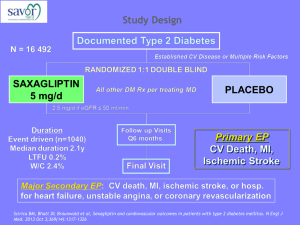
Nateglinide and Valsartan in Impaired Glucose Tolerance Outcomes Research` Rury R. Holman, MB, ChB, FRCP Professor of Diabetic Medicine Director, Diabetes Trials Unit, Oxford Robert M. Califf, MD, MACC Vice Chancellor for Clinical Research Donald F. Fortin Professor of Cardiology, Duke University Director, Duke Translational Medicine Institute For the NAVIGATOR Study Group NAVIGATOR Trial Organization Data Monitoring Committee Executive Committee Trial Oversight Publications Endpoint Committees Steering Committee Trial Operations 43 Members Novartis Research Sites 806 centers in 40 countries Sponsored by Novartis Pharmaceuticals Primary Objective To evaluate whether valsartan or nateglinide, in addition to lifestyle modification, can reduce the risk of diabetes and cardiovascular events in persons with impaired glucose tolerance (IGT) and either cardiovascular disease or risk factors for cardiovascular disease NAVIGATOR 2 × 2 Factorial Design Valsartan Comparison Nateglinide/Placebo (n=2329) Valsartan/Placebo (n=2315) Placebo/Placebo (n=2346) Nateglinide Comparison Valsartan/Nateglinide (n=2316) • All subjects participated in a lifestyle modification program • Nateglinide 60 mg three times a day before meals • Valsartan 160 mg once a day NAVIGATOR Global Enrollment Europe 4909 North America 2146 9306 patients 806 centers 40 countries Asia-Pacific 692 Africa 153 Central & South America 1406 Major Inclusion Criteria IGT* plus FPG ≥95 mg/dL (≥5.3 mmol/L) and either CVD and age 50 yr or 1 risk factor for CVD and age 55 yr *Impaired glucose tolerance according to ADA definition: Nathan DM et al, Diabetes Care, 2007 Coprimary Endpoints • Incidence of diabetes FPG ≥126 mg/dL (≥7.0 mmol/L) and/or 2 hr PG ≥200 mg/dL (≥11.1 mmol/L), confirmed on OGTT within 12 weeks • Extended cardiovascular outcome CV death, nonfatal MI, nonfatal stroke, hospitalization for heart failure, arterial revascularization, or unstable angina • Core cardiovascular outcome CV death, nonfatal MI, nonfatal stroke, or hospitalization for heart failure Nateglinide Data NAVIGATOR Pilot Study Postprandial glucose lowering with nateglinide in IGT Meal Saloranta C et al. Diabetes Care 2002;25:2141-2146 Baseline Patient Characteristics Nateglinide n=4645 Placebo n=4661 Age, years 63.7 ± 6.8 63.8 ± 6.9 Female sex, n (%) 2368 (51.0) 2343 (50.3) White 3854 (83.0) 3880 (83.2) Black 120 (2.6) 116 (2.5) Asian 310 (6.7) 303 (6.5) Other 361 (7.8) 362 (7.8) Weight, kg 83.6 ± 17.2 83.6 ± 17.2 BMI, kg/m2 30.5 ± 5.4 30.5 ± 5.4 Waist circumference, cm 101 ± 14 101 ± 14 Men 104 ± 12 104 ± 13 Women 98 ± 14 98 ± 14 Systolic 139.8 ± 17.5 139.5 ± 17.4 Diastolic 82.6 ± 10.3 82.5 ± 10.2 1140 (24.5) 1126 (24.2) Race, n (%) Mean sitting BP, mm HG History of CVD, n (%) Holman RR et al, N Engl J Med, 2010 Baseline Patient Characteristics (continued) Nateglinide n=4645 Placebo n=4661 Fasting plasma glucose (mmol/L) 6.1 ± 0.45 6.1 ± 0.46 2-hour plasma glucose (mmol/L) 9.2 ± 0.93 9.2 ± 0 .94 Glycated hemoglobin (%) 5.8 ± 0.45 5.8 ± 0.48 Metabolic syndrome, n (%) 3896 (83.9) 3898 (83.6) Total cholesterol, mg/dL 210 ± 41 210 ± 43 HDL, mg/dL 50 ± 13 50 ± 13 LDL, mg/dL 126 ± 36 127 ± 38 151 (109, 208) 150 (107, 209) 0.9 ± 0.2 0.9 ± 0.2 80.3 ± 18.6 81.1 ± 19.0 7.1 (4.5, 14.1) 7.1 (4.5, 14.8) Glycemic indices Lipids Triglycerides, mg/dL Creatinine, mg/dL Estimated GFR mL/min/1.73m2 Urinary albumin:creatinine (mg/g) Holman RR et al, N Engl J Med, 2010 Adherence to Protocol • Taking study drug at 5 years – Nateglinide 70% – Placebo 71% • 13% withdrew consent or lost to follow-up, mostly during extension of trial • Vital status available for 96% of the possible follow-up time • Median follow-up – 6.5 years for vital status – 5.0 years for incident diabetes Holman RR et al, N Engl J Med, 2010 Concomitant Medications Nateglinide n=4645 n (%) Placebo n=4661 n (%) Baseline 330 (7.1) 346 (7.4) Last study visit 729 (15.7) 745 (16.0) Baseline 12 (0.3) 18 (0.4) Last study visit 249 (5.4) 229 (4.9) Baseline 1872 (40.3) 1794 (38.5) Last study visit 1913 (41.2) 1927 (41.3) Baseline 1519 (32.7) 1493 (32.0) Last study visit 1674 (36.0) 1720 (36.9) Baseline 1461 (31.5) 1499 (32.2) Last study visit 1664 (35.8) 1755 (37.7) P Value ACE inhibitor 0.64 Angiotensin-receptor blocker 0.32 Beta blocker 0.82 Calcium channel blocker 0.39 Diuretic Holman RR et al, N Engl J Med, 2010 0.07 Concomitant Medications (continued) Nateglinide n=4645 Placebo n=4661 n (%) n (%) Baseline 1797 (38.7) 1780 (38.2) Last study visit 2301 (49.5) 2358 (50.6) Baseline 1712 (36.9) 1713 (36.8) Last study visit 2119 (45.6) 2114 (45.4) 2 (<0.1) 5 (0.1) 651 (14.0) 670 (14.4) P Value Lipid-lowering drug 0.25 Aspirin/other antiplatelet drug 0.91 Antidiabetic drug Baseline Last study visit—all subjects* *For those with diabetes: 33.3% nateglinide, 37.7% placebo Holman RR et al, N Engl J Med, 2010 0.61 Nateglinide Decreased FPG; Increased 2 Hr PG Holman RR et al, N Engl J Med, 2010 Weight and Waist Circumference Increase with Nateglinide Holman RR et al, N Engl J Med, 2010 Incidence of Diabetes Placebo Nateglinide *Not significant after adjustment for multiple testing Holman RR et al, N Engl J Med, 2010 1580 events (33.9%) 1674 events (36.0%) Extended and Core CV Outcomes Holman RR et al, N Engl J Med, 2010 Placebo Nateglinide 707 events (15.2%) 658 events (14.2%) Placebo Nateglinide 387 events (8.3%) 365 events (7.9%) Adverse Events: Hypoglycemia* Overall, n (%) Mild (maximum severity) Moderate (maximum severity) Severe (maximum severity) Discontinuation for adverse events, n (%) Nateglinide n=4645 Placebo n=4661 P Value 911 (19.6) 676 527 (11.3) 411 <0.001 214 21 104 12 520 (11.2) 485 (10.4) 0.23 *Includes MedDRA preferred terms: hypoglycemia and hypoglycemic seizure Adverse events otherwise did not differ between treatment groups Holman RR et al, N Engl J Med, 2010 Nateglinide Conclusions In people with IGT and CV disease or risk factors, nateglinide in addition to lifestyle modification – Did not reduce the incidence of diabetes (median follow-up 5 yrs) – Did not reduce the co-primary CV outcomes Holman RR et al, N Engl J Med, 2010 Valsartan Data Baseline Patient Characteristics Characteristic Valsartan n=4631 Placebo n=4675 Age, years 63.7 ± 6.8 63.8 ± 6.8 Female sex, n (%) 2317 (50.0) 2278 (51.3) White 3849 (83.1) 3885 (83.1) Black 113 (2.4) 123 (2.6) Asian 298 (6.4) 315 (6.7) Other 371 (8.0) 352 (7.5) Weight, kg 83.5 ± 17.4 83.8 ± 17.1 BMI, kg/m2 30.4 ± 5.5 30.6 ± 5.3 Waist circumference, cm 101 ± 14 101 ± 14 Men 104 ± 13 104 ± 12 Women 98 ± 14 98 ± 14 Systolic 139.4 ± 17.8 139.9 ± 17.1 Diastolic 82.5 ± 10.4 82.6 ± 10.1 1148 (24.8) 1118 (23.9) Race, n (%) Mean sitting BP, mm Hg Any CVD, n (%) McMurray JJ et al, N Engl J Med, 2010 Baseline Patient Characteristics (continued) Characteristic Valsartan n=4631 Placebo n=4675 Fasting plasma glucose (mmol/L) 6.1 ± 0.5 6.1 ± 0.5 2 hr plasma glucose (mmol/L) 9.2 ± 0.9 9.2 ± 0.9 Glycated hemoglobin (%) 5.8 ± 0.5 5.8 ± 0.5 3825 (82.6) 3969 (85.0) Total cholesterol, mg/dL 209 ± 42 209 ± 42 HDL, mg/dL 50 ± 14 50 ± 13 LDL, mg/dL 127 ± 38 127 ± 37 Triglycerides, mg/dL 177 ± 104 117 ± 104 0.9 ± 0.2 0.9 ± 0.2 80.9 ± 18.5 80.4 ± 19.0 0.8 0.8 Glycemic indices Metabolic syndrome, n (%) Lipids Creatinine, mg/dL Estimated GFR mL/min/1.73m2 Urinary albumin:creatinine (mg/g) McMurray JJ et al, N Engl J Med, 2010 Adherence to Protocol • Taking study drug at 5 years – Valsartan 67% – Placebo 66% • 13% withdrew consent or lost to follow-up, mostly during extension of trial • Vital status available for 96% of the possible follow-up time • Median follow-up – 6.5 years for vital status – 5.0 years for incident diabetes Concomitant Medications Medication Valsartan n=4631 n (%) Placebo n=4675 n (%) Baseline 351 (7.6) 325 (7.0) Last study visit 688 (14.9) 786 (16.8) Baseline 10 (0.2) 20 (0.4) Last study visit 212 (4.6) 266 (5.7) Baseline 1863 (40.2) 1803 (38.6) Last study visit 1840 (39.7) 2000 (42.8) Baseline 1483 (32.0) 1529 (32.7) Last study visit 1537 (33.2) 1857 (39.7) Baseline 1451 (31.3) 1509 (32.3) Last study visit 1578 (34.1) 1841 (39.4) P Value ACE inhibitor 0.005 Angiotensin-receptor blocker 0.02 Beta blocker <0.001 Calcium channel blocker <0.001 Diuretic, n (%) McMurray JJ et al, N Engl J Med, 2010 <0.001 Concomitant Medications (continued) Medication Valsartan n=4631 n (%) Placebo n=4675 n (%) Baseline 1782 (38.5) 1795 (38.4) Last study visit 2298 (49.6) 2361 (50.5) Baseline 1729 (37.3) 1696 (36.3) Last study visit 2103 (45.4) 2130 (45.6) 1 (<0.1) 6 (0.1) 588 (12.7) 733 (15.7) P Value Lipid-lowering drug, n (%) 0.27 Aspirin/other antiplatelet drug, n (%) 0.64 Antidiabetic drug, n (%) Baseline Last study visit—all subjects* *For those with diabetes: 33.4% valsartan, 37.2% placebo McMurray JJ et al, N Engl J Med, 2010 <0.001 Valsartan Significantly Reduced Mean Sitting BP McMurray JJ et al, N Engl J Med, 2010 Valsartan Reduced Fasting and 2 Hr Glucose McMurray JJ et al, N Engl J Med, 2010 Incidence of Diabetes Placebo Valsartan McMurray JJ et al, N Engl J Med, 2010 1722 events (36.8%) 1532 events (33.1%) Extended and Core CV Outcomes Placebo 693 events (14.8%) Valsartan 672 events (14.5%) Placebo Valsartan McMurray JJ et al, N Engl J Med, 2010 377 events (8.1%) 375 events (8.1%) Exploratory Outcomes: CV & Total Mortality McMurray JJ et al, N Engl J Med, 2010 Placebo Valsartan 327 events (7.0%) 295 events (6.4%) Placebo Valsartan 116 events (2.5%) 128 events (2.8%) Adverse Events of Interest Valsartan n=4631 n (%) Placebo n=4675 n (%) P Value Hypotension-related* 1964 (42.4) 1680 (35.9) <0.001 Hypertension 693 (15.0) 950 (20.3) <0.001 Renal dysfunction 136 (2.9) 146 (3.1) 0.55 Hyperkalemia 35 (0.8) 35 (0.7) 0.99 Hypokalemia 45 (1.0) 84 (1.8) <0.001 Hypoglycemia 731 (15.8) 707 (15.1) 0.39 Hyperglycemia 45 (1.0) 44 (0.9) 0.93 Angioedema 89 (1.9) 123 (2.6) 0.02 *MedDRA preferred terms include: hypotension, dizziness (including dizziness exertional, dizziness postural), syncope, presyncope and shock (not otherwise specified) McMurray JJ et al, N Engl J Med, 2010 Valsartan Conclusions In people with IGT and CV disease or risk factors, valsartan in addition to lifestyle modification leads to: – 14% relative (3.8% absolute) reduction in the incidence of diabetes (median follow-up 5 yrs) – Did not reduce the co-primary CV outcomes McMurray JJ et al, N Engl J Med, 2010 Thoughts After NAVIGATOR • We are in the midst of a global epidemic of obesity, diabetes, and associated cardiovascular disease. • Many people with impaired glucose tolerance will develop diabetes in a short period of time, even with standard medical care. • Lifestyle intervention remains the cornerstone of diabetes prevention and therapy for impaired glucose tolerance. • We must continue to seek better pharmacological treatments while emphasizing exercise and weight control to prevent diabetes and its morbid and mortal consequences. • NAVIGATOR demonstrates once again that the risks and benefits of therapies cannot be predicted accurately based on biology and intermediate measures, so they must be empirically demonstrated with proper RCTs Slides Available from www.dtu.ox.ac.uk www.dcri.org Disclosures Robert M. Califf, MD reports receiving research grant support from Novartis Pharmaceuticals, Johnson & Johnson/Scios, Lilly, Merck, and Schering Plough, and consulting fees from Annenberg, Aterovax, Bayer/Ortho McNeil, BMS, Boehringer Ingelheim, GSK, WebMd/theheart.org, Johnson and Johnson/Scios, Kowa Research Institute, McKinsey & Company, Medtronic, Merck, Novartis Pharmaceuticals, Sanofi Aventis, and Schering Plough, and an equity position with NITROX, LLC. All personal income from industry relations is donated to non-profit entities. Dr. Califf's industry relations are kept up to date quarterly at www.dcri.org/coi.jsp. Disclosures Rury R. Holman MD, reports receiving grant support from Asahi Kasei Pharma, Bayer Healthcare, Bayer Schering Pharma, Bristol-Myers Squibb, GlaxoSmithKline, Merck, Merck Serono, Novartis, Novo Nordisk, Pfizer, and Sanofi-Aventis, consulting fees from Amylin, Eli Lilly, GlaxoSmithKline, Merck, and Novartis, and lecture fees from Astella, Bayer, GlaxoSmithKline, King Pharmaceuticals, Eli Lilly, Merck, Merck Serono, Novo Nordisk, Takeda and Sanofi-Aventis.