Intravenous Drug Administration
advertisement
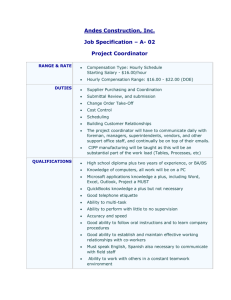
Medication errors & how to minimise them! Kevin Gibbs Clinical Pharmacy Manager Bristol Royal Infirmary Aims To provide an awareness of: Common medication errors How to minimise these The National Patient Safety Agency Resources available to you to aid in safer prescribing Objectives By the end of the session you should be able to: Define a medication error List the ‘Five Rights’ Understand the NHS role in safer prescribing Prescribe safely………… What is an error? What is an error ? Doses omitted Wrong dose Unprescribed drug given Wrong dosage form given Wrong route of administration Wrong rate of administration Yes Yes Yes Yes Yes Yes Wrong time of Yes administration time of day in relation to food etc.... Using unstable/expired drug Wrong administration technique Incorrect reconstitution Extra dose given Yes Yes Yes Error in …. Prescribing Dispensing Administration Counselling/communication Adverse events – What is the problem Adverse-events per admission (%) AE number / year in UK Cost in additional hospital stay (£) Cost of clinical negligence schemes/yr Medication errors = % of incidents 10% 850,000 £2 billion £400 million 25% Incidence Difficult to estimate due to varying definitions - US/UK Prescribing errors 3-20 per 1000 prescriptions Medication errors 1 per patient per day Been estimated that drug errors account for 1/5 of all deaths due to adverse drug events Prescribing errors Process Error Rate Prescribing errors (Primary Care) Computer generated 7.9% Prescribing errors (Primary Care) Hand written 10.2% Prescribing errors (Hospital) 1.5% Serious Errors 0.4% Dean B, Schachter M, Vincent C, Barber N. Quality and Safety in Healthcare 2002; 11:340-344 Shah SNH, Aslam M and Avery AJ. Pharm J. 2002; 267: 860-862 Dispensing and Admin Errors Stage of process Error Rate Serious Errors Dispensing errors (P) 1% 0.18% Dispensing errors Undetected (H) 0.0002 Administration Oral Medicines (H) 3 – 8% Preparation and admin of parenteral medicines 13%- 49% UK references 1 – 12 from Building a safer NHS, Medication Safety 1% The NHS position on error Avoidable failures occur; Untoward events which could be prevented recur, often with devastating results Incidents which result from lapses in standards of care in one hospital do not reliably lead to correction throughout the NHS Circumstances which predispose to failure are not well recognised An Organisation with a Memory Department of Health (2000) http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidan ceArticle/fs/en?CONTENT_ID=4006525&chk=wlMQiJ Patient safety The process by which an organisation makes patient care safer. This should involve: risk assessment; the identification and management of patient-related risks; the reporting and analysis of incidents; and the capacity to learn from and follow-up on incidents and implement solutions to minimise the risk of them recurring. National Patient Safety Agency Collect and analyse information on adverse events Assimilate other safety-related information Learn lessons and ensure that they are fed back into practice Where risks are identified, produce solutions to prevent harm, specify national goals and establish mechanisms to track progress NPSA: Patient safety incident any unintended or unexpected incident which could have or did lead to harm for one or more patients receiving NHS funded healthcare. this is also referred to as an adverse event / incident or clinical error, and includes near misses. NPSA: Seven steps to patient safety Step 1 Step 2 Step 3 Step 4 Step 5 Step 6 Step 7 Build a safety culture Lead and support your staff Integrate your risk management activity Promote reporting Involve and communicate with patients and the public Learn and share safety lessons Implement solutions to prevent harm NHS action on medication errors Reduce to zero the number of patients dying or being paralysed by maladministered spinal injections by the end of 2001 Reduce by 40% the number of serious errors in the use of prescribed medicines by 2005 Building a safer NHS for patients Department of Health (2001) www.doh.gov.uk/buildsafenhs Improving medication safety January 2004 www. doh.gov.uk/buildsafenhs/medicationsafety Improving medication safety 1. 2. 3. 4. Medication safety – a worldwide health priority. Medication errors: definition, incidence, causes. The medication process, prescribing, dispensing, administration. Reducing risks for specific patients groups. Patients with allergies Seriously ill patients Children Improving medication safety 5. Reducing the risks for specific medicines 6. Anaesthetic practice Anticoagulants Cytotoxic drugs Intravenous infusions Methotrexate Opiate analgesics Potassium chloride Organisational and environmental strategies Information management and technology Improved labelling and packaging Interfaces between healthcare settings Education and training for medication safety Managing medication safety in secondary care NHS Trusts should have dedicated machinery for organisation wide management of patient safety. The CNST has developed new standards for medicines. This requires trusts to have medicines management policies, together with annual reports, improvement programmes with defined objectives and progress. Prescribing responsibilities Drug Dose Route Rate of administration Duration of treatment Checking patient allergies & sensitivities Providing a prescription that is: Legible Legal Signed Giving all information to allow safe administration Internationally Research says: USA 44-98,000 deaths “To Err is Human” Australia 250,000 adverse events 50,000 permanent disability 10,000 deaths “Iatrogenic Injury in Australia” Denmark confirmed 9% of admissions Commonest causes of medication errors Lack of knowledge of the drug – 36% Lack of knowledge about the patient “rule” violations – 10% “Slip” or memory loss – 9% JAMA 1995;274:35-43 Common error types Wrong patient Contra-indicated medicine Allergy, medical condition, drug-drug interaction Wrong drug / ingredient Wrong dose / frequency Wrong formulation Wrong route of administration Wrong quantity Poor handwriting on Rx Incorrect IV administration calculations or pump rates Poor record keeping/checking double doses wrong patient Paediatric doses Poor administration technique Complicated prescriptions Calculations Verbal orders Lack of knowledge about drugs Mistakes in identifying drugs names packaging misreading Examples Rx: Insulin 7 stat read as 70 units, given Erythromycin 500mg IV Highly irritant – should in 50ml ISMN 10mg be 250-500 ml ISTIN 10mg given Vancomycin IV 1g Isosorbide mononitrate given instead of amlodipine given as bolus rather than infusion cardiac arrest Ceftazidime 2g tds IV written badly Methotrexate 20mg daily (Dx: RA) Digoxin 125mg IV Should be weekly loading dose 10mg od Neutropenia Should be micrograms Discharged on warfarin Cefotaxime given given - cardiac arrest Not referred for dose adjustment to clinic 14days of 10mg od INR 12.3 Weight-related dose for tinzaparin – 80kg body weight estimated CABG patient, standard therapy Galantamine re-started after a gap 8ml qds Patient was 51kg Thyroxine missed on admission, discovered day 10 Should have been 12mg (2ml) bd PRHO confused over liquid strength Anaesthetist adjusted rate of fentanyl syringe pump in Theatre Rx: Co-amoxiclav Penicillin-alllergic Rx: morphine 0.4ml 30% sodium chloride used instead of 0.9% to dilute an epidural New pump. Increased rate x 1000 Respiratory arrest Did not realise this is a penicillin – anaphylaxis 4ml given Severe pain Rx: Ranitidine 50mg In Theatre: Sodium chloride flush for a central line switched with fentanyl IV line flushed with sodium chloride 0.9% Given via epidural line rather than central line Respiratory arrest. Syringes made up in advance and not labelled Was in fact Potassium 15% - death. Ampoules look similar in design. Case study 1 – "Cambridge" Rx Methotrexate 17.5mg once a week New Rx 10mg once a day 10mg daily dispensed by locum pharmacist Rx error noticed by 2nd GP, but the computer record was not altered +5/7 patient admitted to ENT ward Drug chart written for 100mg daily +1/7 Nurse d/w patient – back to 10mg od +1/7 Pharmacist queries and asks nurse to ask Dr to check dose GP records confirm 10mg od +2/7 blood tests re-checked } Haem +5/7 patient dies Case study 2 – “Nottingham” Rx Intrathecal methotrexate under GA in theatre by Oncology Reg & intravenous vincristine on ward by specialist nurse "Outlied" on non-specialist ward Both drugs delivered to theatre from ward Given food pre-op – op postponed Orignal SpR off-duty now Cover SpR unable to leave ward, anaesthetist to admin intrathecal drug Aneasthetist had given I/Thecal drugs before but had never given chemotherapy Methotrexate given intravenously Vincristine given intrathecally Patient died How to handle errors Is there an acceptable rate ? Should errors be graded or scored for severity ? Blame vs. No blame Analyse why the errors have occurred and try to prevent reoccurrence When things go wrong The "patient-centered“ approach Identify an individual to blame Focus on events surrounding the adverse event Focus on the human acts or omissions immediately preceding the event Blame, name & shame Myths Perfection myth If people try hard enough they will not make any errors Punishment myth If we punish people when they make a errors, ther will make fewer of them Or/ “Active learning” = Understanding causes of failure Human error may precipitate a serious error but Deeper, systematic, factors are usually present Addressing these would have prevented the error Humans are fallible Errors are inevitable Change work conditions to make humans less error-provoking Why did the defences fail? What factors contributed to the failure? CPD How can we help you? Clinical pharmacists How can we help you? Medicines Information Department How can we help you? Formularies and Prescribing guidelines MEDICAL DIRECTORATE ANTIBIOTIC GUIDELINES 1) 3) 4) 5) Don’t use IV antibiotics without good cause 2) Don’t use multiple antibiotics without good indications Don’t give IV therapy for more than 2 days without review (nurses/pharmacists will request new prescription) (IV to Oral policy) Don’t prescribe antibiotics for acute asthma without strong evidence of bacterial infection (usually viral) Review antibiotics when results e.g., urine, blood, sputum cultures etc are available. Use oral antibiotics for 5-7 days unless otherwise stated. Doses assume adult with normal renal function INFECTION COMMENTS DRUG DOSE DURATION OF TX Intravenous Benzylpenicillin should be switched to oral Amoxicillin where appropriate. Infective Exacerbation of COPD Community Acquired Pneumonia Risk Factors in CAP (CURB-65) C = confusion MTS 8 or less U = Urea >/= 7mmol/l R = Resp. Rate >/= 30/min B = BP Systolic < 90 mmHg +/- Diastolic </= 60 mmHg 65 = age >/= 65 yrs Amoxicillin Moxifloxacin Amoxicillin 500mg po 8 hourly 400mg po once daily 500mg po 8 hourly Mild – if atypical suspected or penicillin allergic Severe Moxifloxacin 400mg po once daily Benzylpenicillin PLUS Ciprofloxacin Severe – penicillin allergic Levofloxacin 2.4grams (4mu) iv 6 hourly 750mg po 12 hourly 500mg iv 12 hourly If penicillin allergic Mild 5 days 7-10 days 7-10 days Switching to oral Moxifloxacin 400mg po once daily Legionella Pneumonia Ciprofloxacin PLUS Rifampicin 750mg po 12 hourly 300mg-600mg iv/po 12 hourly 2-3 weeks Suspected Staphylococcal Pneumonia Flucloxacillin PLUS Gentamicin 2 weeks 5 days then review Amoxicillin 2grams iv 6 hourly 4mg/kg/day iv single daily dose (check trough level) 2.4grams iv 6 hourly 500mg iv 8 hourly or 1gram pr 8-12 hourly 500mg po 8 hourly Moxifloxacin 400mg po once daily Benzylpenicillin PLUS Ciprofloxacin (Consider Vancomycin instead of Benpen. – if MRSA colonised) 2.4grams (4MU) iv 6 hourly 750mg po 12 hourly (1gram iv 12 hourly and check levels) Ceftriaxone 4grams iv once daily Benzylpenicillin PLUS Metronidazole Aspiration Pneumonia Mild Nosocomial Chest Infection If penicillin allergic Severe Nosocomial Chest Infection Meningitis All Cases Initial treatment THEN discuss further management with microbiologists Cellulitis If penicillin allergic Cellulitis in Diabetics If Over 55yrs ADD Ampicillin Benzylpenicillin PLUS Flucloxacillin Clindamycin Co-amoxiclav 2grams iv 4 hourly 2.4grams (4MU) iv 6 hourly 1gram iv 6 hourly 600mg iv 6 hourly or 450mg po 6 hourly 625mg po 8 hourly Depends on individual case. OR Ciprofloxacin PLUS Clindamycin Trimethoprim Ampicillin PLUS Ciprofloxacin Urinary Tract Infection Urinary Catheter Infections and Pyelonephritis Sepsis of unknown source PLUS Stat dose Gentamicin Mild Severe (Life Threatening) Benzylpenicillin PLUS Ciprofloxacin Ceftriaxone PLUS Gentamicin 750mg po 12 hourly 450mg po 6 hourly 200mg po 12 hourly 1gram iv 6 hourly 750mg po 12 hourly 4mg/kg iv single dose 2.4grams (4MU) iv 6 hourly 750mg po 12 hourly 4grams iv once daily 4mg/kg/day iv single daily dose (check trough) 3 days How can we help you? Resources BNF Medicines for Children Safe prescribing: A summary Clear and unambiguous Care with units Legal Is it weight/BSArelated dosing. Is weight accurate? Approved name No abbreviations Care with IVs Clear decimal points 0.5ml not .5ml Rewrite charts ***** In English If abbreviate use ‘standard’ ones od / bd / tds / qds regularly NOT 250mg3 Take time, eg to read labels Care if: Impaired renal function (NB: GFR) Hepatic dysfunction Children The elderly Drug unknown to you Very new drug The “5 Rights” • the right patient • the right drug • the right time • the right dose • the right route If in doubt …….. Please ask Further reading/references Naylor, R. Medication Errors. Radcliffe Press. ISBN 1857759567 Department of Health. (2004). Building a safer NHS. Improving patient safety. National Patient Safety Agency (NPSA) (UK) Website: http://www.npsa.nhs.uk/ Institute for Safe Medication Practices (ISMP) (American) Website: http://www.ismp.org/