File
advertisement

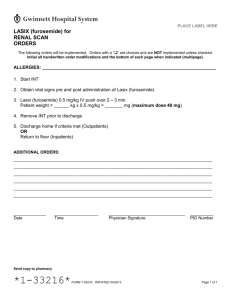
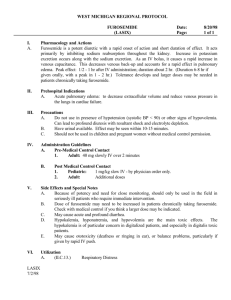
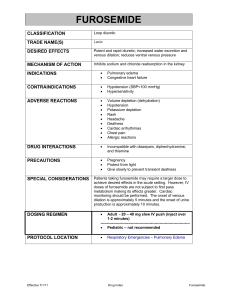
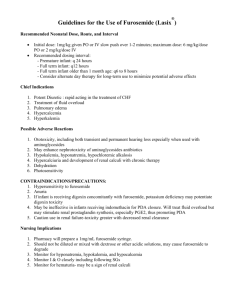
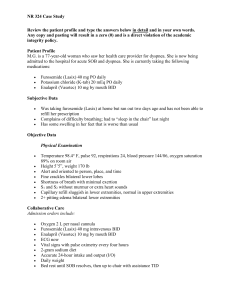
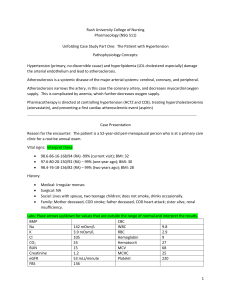
CHF 2 1 A 65-year-old man presents to the clinic with peripheral edema and dyspnea on exertion that have progressively worsened. His medical history is significant for coronary artery disease and hypertension . Other pertinent diagnostic and laboratory findings include: left ventricular ejection fraction (LVEF) 35% ,systolic blood pressure (SBP) 130/85 mm Hg,heart rate (HR) 78 beats/minute, serum creatinine (SCr) 0.9 mg/dL, and serum potassium 4.2 mEq/L. Acute cardiac ischemia is ruled out; however, a diagnosis of stable symptomatic heart failure (HF) with reduced ejection fraction (EF) is made. The patient’s weight is presently 6 kg above baseline. Current medications include aspirin (ASA) 325 mg/day and amlodipine 5 mg/day. 1 Which is the best recommendation for thispatient? A. Admit patient to the hospital and initiate furosemide 80 mg intravenously two times/day. B. Initiate therapy with enalapril 5 mg orally two times/day and carvedilol 3.125 mg orally two times/day. C. Initiate furosemide 20–40 mg orally two times/day and enalapril 2.5–5 mg orally two times/day. D. Initiate hydrochlorothiazide (HCTZ) 25 mg/day. 2 Routine treatment with evidence-based therapies remains the cornerstone of pharmacotherapy for patients with HF. Which is the best recommendation for treating stage C systolic HF? A. Angiotensin-converting enzyme (ACE) inhibitors and diuretics. B. ACE inhibitors, β-Blockers, and diuretics if needed for fluid retention. C. β-Blockers and digoxin. D. ACE inhibitors, digoxin, and inotropes. H.F. is a 70-year-old patient with chronic stage C HF who had stable symptoms until about 3 months ago. At that time, the patient was hospitalized for acute decompensated heart failure . During the hospitalization, he received intravenous diuretics for hypervolemia; ultimately, he was discharged on the following medical regimen: lisinopril 20mg/day, digoxin 0.125 mg/day, and furosemide 80 mg two times/day. One month after discharge, metoprolol controlled release/ extended release (CR/XL) 12.5 mg/day was initi- ated; 2 weeks later, this was increased to 25 mg/ day. His medication regimen has been stable for the past 1½ months. Today, the patient presents to the clinic with lightheadedness. The patient’s BP while sitting is 115/70 mm Hg, HR while sitting is 68 beats/minute, BP while standing is 90/68 mm Hg, and HR while standing is 82 beats/minute; orthostatic hypotension is confirmed. Other pertinent diagnostic and laboratory findings include sodium (Na) 140 mEq/L, potassium (K) 4.2 mEq/L, blood urea nitrogen (BUN) 63 mg/dL, and SCr 1.2 mg/ dL. Physical examination reveals the following: cardiac, regular rate and rhythm; neck, no elevated jugular venous distension; lungs, clear to auscultation; and extremities, no evidence of edema. Which is the best recommendation for this patient? A. Decrease dose of metoprolol XL. B. Decrease dose of furosemide. C. Decrease dose of lisinopril. D. Discontinue metoprolol XL and initiate carvedilol 3.125 two tim es/day