Palliative Care
advertisement
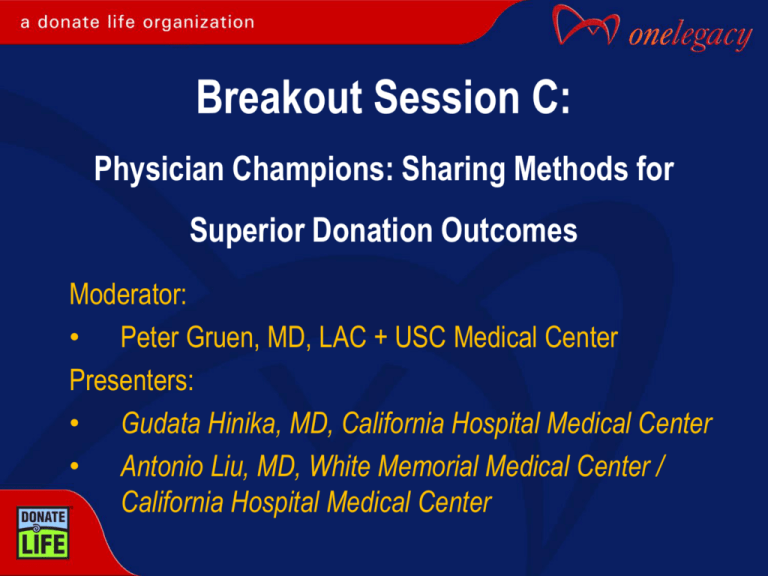
Breakout Session C:
Physician Champions: Sharing Methods for
Superior Donation Outcomes
Moderator:
• Peter Gruen, MD, LAC + USC Medical Center
Presenters:
• Gudata Hinika, MD, California Hospital Medical Center
• Antonio Liu, MD, White Memorial Medical Center /
California Hospital Medical Center
Questions to Run On
What “best practices” presented today would improve
the brain death declaration and the organ donation
processes in your hospitals?
What “best practices” presented today will you share
with your physician colleagues?
Antonio Liu, MD
Neurologist
Objectives
By the end of this presentation, the attendee will be
able to:
• Identify “best practice” standards for brain death
determination.
• Identify effective family-centered care for families facing a
brain death diagnosis
• Understand cultural sensitivity surrounding brain death
diagnosis
What is Brain Death?
Neurologic determination of death
Irreversible loss of function of the brain and brainstem
Spinal cord reflex does not count
Confounding Practices
There is a need for standardization:
• Wide variance in brain death determination practices
• In large hospital, neurologists diagnosis 25 – 30 times /year
• In small hospitals, physicians diagnosis 0 – 3 times / year
• Hospital Brain Death Policies may not proceduralize the
clinical exam or documentation requirements
• Physicians may not be confident to declare patients without
detailed standards of practice
The public expects physicians to get “dead” right
Brain Death Legislation
National: Uniform Determination of Death Act
Approved in 1981
In cooperation with AMA, ABA,
President’s Commission on Medical Ethics
Adopted by most states
State: California Health and Safety Code, Section 7184
An individual who has sustained either 1) irreversible cessation of
circulation and respiration, or 2) irreversible cessation of all functions
of the entire brain, including brainstem, is dead. A determination of
death must be made in accordance with accepted medical standards.
American Academy of Neurology (AAN)
Guidelines 2010
Prerequisites
• Acute CNS catastrophe
• Exclusion of confounding factors
• No intoxication or poisoning
• Core Temp > 36C
Three cardinal findings
• Coma
• Lack of brainstem reflexes
• Apnea . . . . . . . not just another clinical test
American Academy of Neurology (AAN)
Guidelines 2010
Ancillary Testing
Angiography
EEG
Transcranial doppler
Technetium 99 brain scan “hollow skull”
Somatosensory evoked potentials
New AAN: Ancillary testing may take the place of apnea testing
if it is inconclusive or it has to be aborted.
Improved Brain Death Policies
Alleviate variance in brain death determination practices
Implement a Standard Brain Death Note
Update policies to reflect new AAN guidelines
Proceduralize comprehensive clinical exam
Integrate AAN Checklist to Standardize
Brain Death Diagnosis and Documentation
Prerequisites (all must be checked):
Coma, irreversible and cause known
Neuroimaging explains coma
CNS depressant drug effect absent
No evidence of residual paralytics
Absence of severe acid-base, electrolyte, edocrine abnormality
Normothermia or mild hypothermia (core temp > 36 C)
Systolic blood pressure > 100 mm Hg
No spontaneous respirations
Integrate AAN Checklist to Standardize
Brain Death Diagnosis and Documentation
Examination (all must be checked):
Pupils nonreactive to bright light
Corneal reflex absent
Oculocephalic reflex absent (tested only if C-spine integrity ensured)
Oculovestibular reflex absent
No facial movement to noxious stimuli at supraorbital nerve,
temporomandibular joint
Gag reflex absent
Cough reflex absent to tracheal suctioning
Absence of motor response to noxious stimuli in all four limbs (spinally
mediated relexes are permissible)
Integrate AAN Checklist to Standardize
Brain Death Diagnosis and Documentation
Apnea testing (all must be checked):
Patient is hemodynamically stable.
Ventilator adjusted to provide normocarbia (PaCO2 35 – 45 mm HG).
Patient preoxygenated with a PEEP of 5 cm of water.
Provide oxygen via a suction catheter to the level of the carina at 6 L/min or
attach T-piece with CPAP at 10cm H2O.
Disconnect ventilator.
Spontaneous respirations absent.
Arterial blood gas drawn at 8-10 minutes, patient reconnected to ventilator.
PCO2 > 60 mm Hg, or 20 mm Hg from normal baseline value.
OR:
Apnea test aborted.
Integrate AAN Checklist to Standardize
Brain Death Diagnosis and Documentation
Ancillary testing (only one needs to be performed) (to be ordered only if clinical examination
cannot be fully performed due to patient factors, or if apneas testing inconclusive or aborted):
Cerebral angiogram
HMPAO SPECT
EEG
TCD
Normothermia or mild hypothermia (core temp > 36 C)
Systolic blood pressure > 100 mm Hg
No spontaneous respirations
Time of death (DD/MM/YY): _______ / ________ / ________
Name of physician and signature: _______________________
Sensitive family-centered care
Who informs the family about grave prognosis?
Who informs the family about the impending brain death
examination? And the exam results?
Who informs the family about the opportunity for organ
and tissue donation?
When, and how, does the physician / hospital sensitively
introduce OneLegacy to the family?
Sensitive family-centered care
Preparing a family to meet with OneLegacy:
“I am very sorry for your loss. We will give you some time
alone to be together as a family, and if you have any
questions, we will contact {nurse, social worker, chaplain} for you.
Later, we will introduce someone specialized in End-of-Life
decisions to support you and your family
through the next steps.”
Sensitive family-centered care
• Timing is almost EVERYTHING!
• Family may need time between brain death discussion
with physician and donation discussion with OneLegacy.
• Family acceptance of brain death diagnosis is necessary
before introducing the discussion of organ donation.
Sensitive family-centered care
All donation discussions with family should be planned
events.
Who? Where? When? clearly customized for each family
during hospital and OneLegacy care plan “huddle”.
Avoid the perception of conflict of interest.
Cultural Diversity & Brain Death
Cultural differences may influence acceptance of brain death:
Western vs. Eastern philosophies of mind / body /spirit
connection
Coma vs. Brain Death: waiting for a miracle
Socially or economically disenfranchised may not trust diagnosis
Responding to cultural differences:
Show and Tell - “seeing is believing”
Multiple family conferences to clarify
Balance sensitivity with definitiveness
Summary
Updated AAN Guidelines can be incorporated into
hospital policies to standardize brain death determination
practices.
Sensitive family-centered care requires coordinated
efforts of the right experts to support the family at the
right time.
Physicians should be prepared to aid families from varied
cultural backgrounds to best understand and accept the
brain death diagnosis.
Thank You
Contact:
Antonio Liu, MD
(323) 987-1362
American Academy of Neurology (AAN)
www.aan.com
Physician Champions:
Sharing Best Practices
Dr. Gudata Hinika
Chief of Trauma
California Hospital Medical Center
Objectives
By the end of this presentation, the attendee
will be able to:
1) Identify procedures and protocols for improving
patient resuscitation in the ED.
2) Understand the value of a having an active multidisciplinary Donation Council with physician
leadership.
3) Identify specific strategies for improving hospital
and OneLegacy partnerhip from referral to
recovery.
California Hospital Demographics
• Trauma Level II facility
• 316-bed acute care hospital
• Located in downtown Los Angeles
• Serving primarily lower income and transient
population
CHMC Organ Donation Data
2008
2009
2010
CMS Goal
Organ Donors
4
10
16
Eligible Deaths
14
15
20
Total Organs Transplanted
13
27
57
OTPD
3.25
2.70
3.80
3.75
Conversion Rate
29%
67%
75%
75%
Timely Referrals
96%
96%
92%
100%
Effective Request
89%
64%
73%
100%
ED Protocol
• ED Level I, II, and Consultation Activation
• Level I:
All key team members must respond, i.e.; (Blood Bank,
Trauma Surgeon, Anesthesiologist, ED physicians, RNs, RTs, & Radiology)
•
Sign-in sheet upon staff arrival
• Resuscitation measures
• GOAL: Patient receives multi-disciplinary
resuscitation
ED Protocol
Once resuscitation is achieved:
• Allows for immediate ED to OR time
• ICU maintains 1 available bed for Trauma
Donation Council
•
•
•
•
•
•
•
CHMC established Donation Council 8/2010
GOAL: Process Improvement
High Level Chair with physician influence
Active OneLegacy Coordinator
Multi-disciplinary – meets quarterly
Review all referrals/cases/timeliness
Chair holds Lead persons accountable for PI
OneLegacy Partnership
Education is key
•
•
•
•
Nursing Competencies/Annuals
Department meetings
Grand Rounds
Hospital knowledgeable on policies & process
Early Referral for Imminent & Cardiac Death
• Avoids missed/late referrals for organ and tissue
• CMS mandate = Goal is 100% timeliness
RN Champions
• What is a Nurse Champion?
A registered nurse (preferably not a charge nurse) formally recognized as
an advisor on the donation process. Nurses, physicians, RT’s,
OneLegacy coordinators, and hospital Administration consult
the Nurse Champion, regarding referrals, general donation
policy, protocol or practice.
• When does a facility need one?
Anytime. Nurse Champions foster leadership and peer-to-peer
interaction/education throughout the referral process. And
the charge nurses and manager can rely on the Nurse
Champions to help less experienced staff navigate the referral
process effectively.
RN Champions
• CHMC has 4 Nurse Champions!!
• 3 day shift & 1 night shift
• Multiple referrals in units at one time with several OL
coordinators onsite, same physicians, etc.
• Champions help with overall organization and
communication in real-time for staff,
OneLegacy and families.
OneLegacy Partnership
C O M M U N I C A T E!
C O M M U N I C A T E!
C O M M U N I C A T E!
• Multiple huddles (all teams w/OneLegacy involvement)
• Involve your RN Champions early for assistance
• Have OL Coordinator e-mail updates to all Donor Council
members to keep updated on referrals/donors
THANK YOU!
Contact information:
Dr. Gudata Hinika
California Hospital Medical Center
Gudata.Hinika@chw.edu
(323) 545-9288
QUESTIONS
for
Dr. Liu & Dr. Hinika?
Questions to Run On
What “best practices” presented today would improve
the brain death declaration and the organ donation
processes in your hospitals?
What “best practices” presented today will you share
with your physician colleagues?