Dworken Service Overview
advertisement

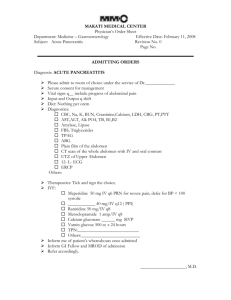
Intro to Dworken (GI) Intern Boot Camp Jacob Sadik, PGY3 What You Will Learn How to survive Dworken How to recognize when a GI patient is sick How to diagnose/manage a few commonlyencountered GI diseases (Biliary disease, transaminitis, comprehensive discussion on GIB, hepatitis and cirrhosis covered in other boot camp lectures) High-Yield Slides Dworken Lksd 55 is your home 2 interns, 1 senior, 2 fellows, 2 attendings (liver, GI) Spend time in the endoscopy lab when you can! Your senior/fellow are always there to help!! The only stupid question is the one you didn’t ask! Dworken Patients Take a GI-focused history Prior GI diagnoses Prior endoscopic studies (EGD, C-scope, CE, ERCP) NSAIDs, anti-platelets, anticoagulation Shadow of a doubt?...make NPO! Know your overnight admissions well!!! Notify primary gastroenterologist re: admission Rectal exams on all bleeding patients (even if done in the ED) No consults for hemoccult positive stools!!! OARRS…. is….everything The OARRS Report Ohio reporting system for narcotics and other controlled substances Get access today! https://www.ohiopmp.gov/Portal/Registration/Defa ult.aspx Case 1 A 56 y/o M with a h/o DMT2, DLD, PUD and EtOH abuse arrives on Lksd 55 from the ED with a 1-week h/o progressively worsening, gnawing epigastric abdominal pain radiating to his back. VS: T 36.1, P 118, R 20, BP 100/80, SpO2 96% RA Orthostatics negative FOCUSED EXAM: HEENT: Sclera anicteric, no palatal jaundice SKIN: No jaundice, +axillary sweat, no truncal ecchymoses ABD: Soft, ND, significant TTP over epigastrium without peritoneal signs, no organomegaly NEURO: AAOx3 PERTINENT LABS: Hgb 15 BUN 10, Cr 0.9, lipase 4600 Acute Pancreatitis Classification Type Edematous, interstitial acute pancreatitis Necrotizing acute pancreatitis Severity Mild-mod (absence/transient organ failure <48 hrs) Severe (persistent organ failure >48 hrs) Acute Pancreatitis Diagnosis Requires 2 or more of the following: 1) Acute, persistent, severe epigastric abdominal pain (often radiating to the back) 2) Elevated serum lipase or amylase ≥3x upper limit of normal 3) CT/MRI/ultrasound evidence of AP (NOTE: imaging is not required for uncomplicated mild AP if #1 and 2 are present) Acute Pancreatitis Initial Evaluation Assess severity. ICU transfer may be indicated if 1 or more of the following are present: P <40 or >150 SBP <80 RR >35 PaO2 <50 mmHg pH <7.1 Anuria Coma Acute Pancreatitis APACHE II SCORING SYSTEM Acute Pancreatitis “Surgical” Abdomen Be concerned about… Rigidity, guarding, rebound tenderness, illappearance Portable KUB STAT Acute care surgery consult STAT ICU transfer If no acute surgical intervention per ACS Your senior/fellow will help you with this Acute Pancreatitis Think About Etiology… Gallstones*** EtOH*** Hypertriglyceridemia (TG >1000s) Trauma (e.g. panc laceration, post-ERCP) Drugs Steroids, azathioprine, Januvia, tetracycline, furosemide, thiazides, flagyl, valproate, HAART, etc.. Infection Other mechanical Autoimmune Toxins (e.g. scorpion sting) Hypercalcemia Idiopathic Acute Pancreatitis Supportive Workup RFP(includes Ca) and CBC LFTs Lipid panel (for TG level) Lactate Blood EtOH level (if indicated) Abdominal ultrasound ABG (if altered, SpO2 <90%, bicarb low, etc) CT abd/pelv with contrast CAUTION in those with AKI Diagnostic or to assess for complications in severe AP EUS/MRCP vs. ERCP (in suspected or overt gallstone pancreatitis) Acute Pancreatitis Management 1) 2) 2) 4) Fluid resuscitation!!! Generally ~>200 cc/hr Decreases morbidity/mortality w/in the 1st 12-24 hrs Monitor for improvement (via VS, BUN, Cr, Hct, UOP) Pain control IV opiates Bowel rest NPO CLD Soft, low-residue, low-fat, soft diet NJ feeding (post-ligament of Treitz) > TPN/PPN Metabolic/electrolyte correction Acute Pancreatitis AP Sequelae Non-discrete peri-pancreatic fluid collections Walled off fluid collections (or “pseudocysts”) Necrotizing pancreatitis (+/- secondary infection) Pancreatic ascites Hemorrhagic pancreatitis Abdominal compartment syndrome Pseudoaneurysms Acute Pancreatitis Non-Discrete Fluid Collections Acute Pancreatitis Walled-Off Fluid Collections Acute Pancreatitis Pancreatic Necrosis Acute Pancreatitis Management of Infected Necrosis Empiric antibiotics with good pancreatic penetration (e.g. carbapenems*, quinolones, flagyl) Cover GNRs and anaerobes Trend towards conservative management with ABx and observation for several weeks vs. immediate surgical resection Limited role for CT-guided FNA Open/endoscopic partial/total necrosectomy may eventually be required Acute Pancreatitis Hemorrhagic Pancreatitis Cullen’s Sign Grey Turner’s Sign Acute Pancreatitis Pancreatitis Take Home Points Once Dx is known, assess severity first Does your patient need ICU level care? FLUIDS! Close monitoring (VS, UOP, BUN, lactate, etc.) Etiology will help guide management Be mindful of complications Case 2 A generous NF resident gives you an overnight patient. Pt is a 56 y/o M who presents to the ED with a 1-week h/o progressively worsening left quadrant/flank pain and fever. Endorses associated anorexia, nausea and fatigue. Had a colonoscopy ~1 week ago, revealing scattered, non-bleeding diverticuli. VS: T 38.2, P 100, R 22, BP 128/86, SpO2 100% on RA FOCUSED EXAM: GEN: Well-nourished CM in mod distress d/t pain SKIN: No jaundice ABD: Soft, ND, mild TTP over LLQ without peritoneal signs, no organomegaly NEURO: AAOx3 PERTINENT LABS: WBC 13K with left shift, CRP 10 What is your DDx? Pyelonephritis Acute uncomplicated/complicated diverticulitis Nephrolithiasis Iatrogenic microperforation Acute pancreatitis Infectious colitis Crohns disease CRC Acute appendicitis What do you order next? A CT scan! What is the Dx? Acute Diverticulitis Presentation Mean age ~60s LLQ abd pain Fever Leukocytosis N/V/constipation Recurrence is ~20-40% after initial attack and 20% may have chronic abd pain Acute Diverticulitis Classification 1) Uncomplicated 2) Complicated Perforation Abscess Fistulas Obstruction Peritonitis Acute Diverticulitis Management Bowel rest Antibiotics covering GNRs and anerobes Amp/sulbactam, pip/tazo May be transitioned to PO Augmentin prior to discharge Pain control with IV opiates +/- Surgery consult Indicated for acute complications Surgery decided on case-by-case basis <40 y/o, R-sided disease, immunocompromised Acute Diverticulitis Management Colonoscopy due at least 6-8 weeks out from onset to exclude CRC NOT during acute flare given risk of iatrogenic perforation Acute Diverticulitis Your patient asks, “I read that seeds, nuts and popcorn are bad for my diverticulitis. What do you think? Case 3 You get called from the DACR at 6:50 because a 68 y/o F with a h/o osteoarthritis and SLE (on chronic hydroxychloroquine and prednisone) is in the ED complaining of a 2-day h/o frequent black, tarry stools and lightheadedness. She has been taking Ibuprofen for the past 7 days because of knee pain. VS: T 37, P 120, R 24, BP 104/80, SpO2 99% on RA Orthostatics negative FOCUSED EXAM: GEN: Lethargic, in NAD HEENT: Conjunctival pallor, dry mucous membranes ABD: Soft, ND, epigastric TTP without rebound/rigidity/guarding NEURO: AAOx3 LABS: Hgb 6.4 (baseline 12) BUN 18, Cr 1.34, bicarb 18, K 3.2 Lactate 1.8 GIB What else do you want to know? Use of NSAIDs, anti-platelets, anticoagulants Abdominal pain? Relation to food? Stool color, character, quantity Previous GIB Previous EGD/colonoscopy/CE? EtOH abuse H/o cirrhosis or visualized varices Primary thrombophilia Recent pepto or iron ingestion darkens stools GIB Initial Management NPO CBCs q6h and active T&S with blood consent RFP, LFTs, coags 2 18-gauge (large-bore) PIVs Bolus NS/LR for orthostatic hypotension Stop all NSAIDs, anti-platelets and anticoagulants Hold pharmacologic DVT prophylaxis +/- NG lavage Oxygen as needed Abdominal pain? KUB prior to endoscopy Transfer to ICU? (discuss with your senior) GIB Transfusion Goals Transfuse pRBCs for Hgb <7 (consider <8 in patients with cardiac disease) Transfuse platelets for… Active bleeding with PLT <50K Pre-procedural PLT <50K with/without bleeding Any PLT <10K Transfuse FFP for INR >1.5 in the setting of active bleeding or pre-procedural in some cases GIB Prep Basics EGD NPO +/- erythromycin 3 mg/kg IV q8h (off-label) to clear stomach contents for better visualization – ask GI Flexible sigmoidoscopy or ileoscopy Tap water enemas 30 minutes apart x 3 or until clear Colonoscopy Golytely “split-prep” (2L in the evening, 2L in the early morning; i.e. 7PM, 3AM) Movi-Prep (Gatorade) NG tube if refusing PO GIB Concerning GIB Active bloody bowel movements Hemodynamic instability Drop in Hgb >/= 2 gm/dL or poorly incrementing Hgb after transfusion (1 unit pRBCs should bump Hgb by 1-1.5 g/dL) Change in mental status or symptomatic anemia REMEMBER! Blood is a laxative. Hemodynamically-significant GI blood loss will present itself. Case 4 Your covering the Dworken team pager on NF when you are paged by nursing about a 36 y/o F with a h/o ulcerative colitis who is having multiple, small-volume bloody bowel movements. She has been taking Keflex for the past week for a soft tissue infection. What do you do?!? Examine the patient VSS? Pain? Mentation? Abd exam? DRE? “Show me the stool!” CBC STAT Orthostatics Send C.diff PCR! IBD IBD 2nd-3rd decade of life Crohns disease has bimodal distribution (7th-8th decade) Disease predilection for developed countries and the northern hemisphere Look for extraintestinal manifestations Episcleritis, uveitis, iritis Ankylosing spondylitis Pyoderma gangrenosum Eythema nodosum IBD Genetic Predisposition IBD Immune System Dysregulation Environmental Triggers IBD Crohns Disease Risk factors: smoking, “western” diet Protective factors: high-fiber diet Transmural bowel wall inflammation Entire GI tract (TI most commonly involved) “Skip” cobblestone lesions Rectal sparing Abdominal pain, diarrhea, fatigue, weight loss, kidney stones IBD Diagnosis of CD Colonoscopy with intubation of the terminal ileum and biopsy acquisition is the gold standard MRE is preferred for initial Dx of small bowel CD Consider CE in difficult-to-diagnose cases MRI or EUS to evaluate perianal CD IBD Tx Strategies in CD “Step-Up” Slow-release 5ASA for ileitis Sulfasalazine for colitis Antibiotics if not improving Biologic agent Immunomodulator “Top-Down” Biologic agent Immunomodulator Slow-release 5ASA for ileitis Sulfasalazine for colitis IBD Ulcerative Colitis Bloody diarrhea, tenesmus, fecal urgency, fatigue weight loss and sometimes fever DDx: infectious, ischemic, CD, radiation-induced High CRC risk Predisposition to C.diff colitis Erythematous, engorged mucosa Rectal involvement with continuous progression Crypt abscesses IBD Dx of UC Consider flex sig if inpatient for severe active flare due to risk of iatrogenic complications with colonoscopy Colonoscopy if flare not severe IBD Acute IBD Flares Severe flares Fever (>/= 37.5C) Tachycardia Anemia (Hgb <7 g/dL) Elevated inflammatory markers (ESR, CRP) Corticosteroids NPO Fluid resuscitation Electrolyte correction Consider 5-ASA compound (for those who are not on maintenance therapy) IBD Back to our Patient… Initiate supportive care CRP, ESR, CBC, RFP, LFTs C.diff PCR, stool studies first If C.diff PCR negative, would start steroids High-dose 5-ASA compound (e.g. sulfasalazine) Now you know a little bit about…. The Dworken team How to recognize a sick patient Prep Basics Acute pancreatitis Diverticular Disease GI bleeding (briefly) IBD (briefly)