Document
advertisement

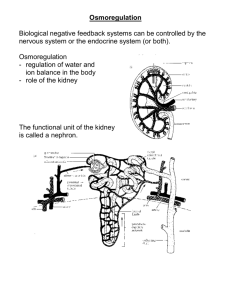
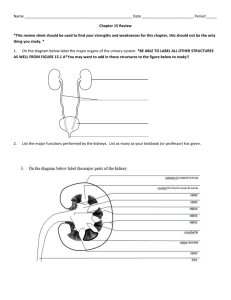
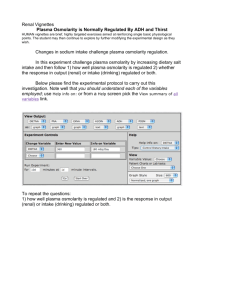
Introduction to Renal Physiology (Excretory System) Basic renal functions Fluid balance Electrolyte balance Elimination of metabolic waste products Components of the system Urinary bladder and associated plumbing Kidneys Basic Anatomy of the Kidney Notice that the only portal into the kidney is the renal artery, the only portals out of it are the renal vein and the ureter. Therefore, everything in the renal artery must wind up in the renal vein or the ureter. Basic anatomy of the nephron Juxtamedullary (20%); Cortical (80%) Renal Circulation About 25% of cardiac output (about 1250 ml;/min) enters renal artery. Nearly all of it gets into the glomerular capillaries. The only blood supply to the renal medulla is the blood in the peritubular capillaries of the juxtamedullary nephrons. That’s only 20% of all nephrons. Therefore, cortex has a rich blood supply, medullary blood supply is much smaller, and moves slowly. Basic Renal Processes Glomerular filtration (about 180 L/day = 45 gallons/day = 125 ml/min) Secretion (into lumen of nephron) Reabsorption (from lumen of nephron) Normal urine production (about 1 L/day – 0.5% of filtrate!) Glomerular filtrate is essentially protein-free plasma. Urine has very different composition. This can’t be true unless various solutes are reabsorbed from and secreted into the lumen of the nephron Glomerular Filtration Forces affecting filtration Hydrostatic pressure in glomerular capillaries (+55 mm Hg) Colloid osmotic pressure of plasma (-30 mm Hg) Hydrostatic pressure in lumen of Bowman’s capsule (-15 mm Hg) Net driving force = +55 – 30 – 15 = 10 mm Hg Why is hydrostatic pressure in glomeruli so high? Glomerular capillaries empty into an arteriole, a resistance vessel Hydrostatic pressure in glomerular capillaries can be varied by varying sympathetic input to afferent arterioles (not much sympathetic innervation to efferent arterioles). Note that filtration can’t occur if glomerular pressure falls to 45 mm Hg. This happens with arterial pressure below about 60 mm Hg. No filtration = no urine = renal shutdown Why doesn’t GFR change with arterial pressure? 1. Juxtaglomerular apparatus: Just outside entrance to Bowman’s capsule, afferent arteriole, efferent arteriole and the macula densa (distal convoluted tubule) all come together; collectively called the juxtaglomerular apparatus. When pressure goes up in afferent arteriole (increased arterial pressure), it presses harder against macula densa. Macula densa then secretes a vasodilator onto the efferent arteriole. This tends to keep glomerular pressure from changing with arterial pressure. 2. Autoregulation: When PO2 goes up or PCO2 goes down, smooth muscle constricts. When arterial pressure goes up, increased flow through afferent arteriole causes local increase in PO2 and decrease in PCO2. Smooth muscle in afferent arteriole constricts, tending to keep pressure in glomerulus constant. Reabsorption from lumen of the nephron Since 180 L/day are filtered and 1 L/day is lost in urine, 179 L/day (99.5%) must be reabsorbed Only mechanism for getting water out of nephron and into interstitial fluid is osmosis. Therefore, if 99.5% of volume is reabsorbed, 99.5% of the solutes must be reabsorbed. There must be lots of active transport of solutes out of the nephron. Some generalities about reabsorption Usually highly active for things that are “useful”. Glucose, for example, is 100% reabsorbed. None enters the urine in healthy people. Usually nonexistent for things that are toxic Since more than 99% of the fluid is reabsorbed, more than 99% of the solutes must be reabsorbed. This can’t happen without active transport Sodium, a cation, is about 40% of the total solutes in plasma, so another 40% has to be anions that maintain electrical neutrality It’s mathematically impossible to reabsorb 99+% of the solutes without reabsorbing at least 99% of the sodium Sodium reabsorption occurs by active transport, driven by a membrane ATPase in the basolateral membranes of the epithelial cells of nephrons Sodium is pumped out of the nephron’s epithelial cells and into the interstitial fluid, is replaced by sodium diffusing out of the lumen and into those cells. It diffuses from the interstitial fluid into the peritubular capillaries. Net effect: sodium leaves the lumen of the nephron, enters renal venules and leaves via renal vein Active transport of other actively reabsorbed solutes (glucose, amino acids, etc.) is linked to and dependent on active transport of sodium Of the sodium that is filtered, about 67% is reabsorbed in the proximal convoluted tubule. Another 25% is reabsorbed in the loop of Henle Therefore, 8% of the filtered sodium gets as far as the distal convoluted tubule. Most of that is reabsorbed. The distal tubule is the only part of the nephron in which sodium reabsorption is controlled (by the hormone, aldosterone). The amount of sodium in the body (and, therefore, the volume of the extracellular fluid) is regulated by varying the amount of sodium reabsorbed in the distal convoluted tubule Renal Reabsorption of Glucose All the filtered glucose - 100% - is reabsorbed in the proximal convoluted tubule. You can’t possibly reabsorb 100% of anything without active transport: at some point it must move uphill in concentration. There are glucose carrier proteins involved in the active reabsorption of glucose. They have a finite capacity – once all glucose binding sites are occupied, they can’t bind more Therefore, there is a maximum rate at which glucose can be reabsorbed. It’s called the transport maximum (Tm). Tm for glucose is around 400 mg/minute Since Tm for glucose = 400 mg/minute, we can ask, “How much glucose enters the lumen of the nephron per minute?” It must be less than 400 mg, otherwise not all the glucose could be reabsorbed The amount of any substance entering the lumen of the nephron per minute is the tubular load. It’s the concentration of that substance in plasma x the volume of plasma entering the lumen of the nephron per minute (the GFR) Plasma glucose concentration is around 1 mg/ml = 100 mg/100 ml = 100 mg% = 100 mg/dl = about 3 mM GFR is around 125 ml/minute Tubular load for glucose is, therefore, 125 ml/min x 100 mg/dl = 125 mg/minute. Since Tm for glucose = 400 mg/minute, the tubular load is totally reabsorbed What happens if plasma glucose levels rise? Consuming a meal with lots of sugar in it causes a transient increase in plasma glucose levels (typically to not more than 200 mg/dl after a nice big piece of heavily frosted birthday cake). This increases the tubular load for glucose to 125 ml/minute x 200 mg/dl = 250 mg/min. This is less than Tm, so all the glucose is reabsorbed in the proximal tubule Plasma glucose levels that go as high as 300 mg/dl (tubular load = 375 mg/minute) are still totally reabsorbed. But if plasma glucose levels get much higher, Tm for glucose is exceeded and some glucose enters the urine. For example, if plasma glucose concentration rises to 500 mg/dl, tubular load for glucose becomes 625 mg/minute and 225 mg of glucose enters the urine per minute. That 325 grams (= 11 ounces; about ¾ pound!) per day. What happens in diabetes? There are two disorders called diabetes. One, the most common endocrine disorder, is diabetes mellitus (diabetes = having a large volume of urine; mellitus = honey-like; same root word as mellifluous) Diabetes mellitus patients have elevated plasma glucose levels. When those levels exceed 300 mg/dl, not all glucose is reabsorbed. The glucose that enters the urine increases urine volume osmotically. It’s been known for centuries that the urine produced by most people who produce large volumes of urine is sweet (attracts dog, flies, physicians) Diabetes Insipidus Diabetes insipidus (diabetes = having a large volume of urine; insipidus = without flavor) is also an endocrine disorder. I’ll come back to it later Sodium Reabsorption and Water Reabsorption Active reabsorption of sodium causes passive reabsorption of an equal amount of anions, mostly chloride. The reabsorption of sodium and chloride create the osmotic gradients that cause nearly all of the reabsorption of water (about 180 liters/day) in the nephrons Passive Reabsorption Some substances are reabsorbed passively, but wind up much more concentrated in urine than in plasma. Huh? Water is reabsorbed osmotically, and diffuses across membranes faster than any other water-soluble substance. Water reabsorption creates concentration gradients (concentration in tubular fluid > than that in plasma) for everything that isn’t actively reabsorbed. Substances that can cross the membranes of the nephron diffuse out, down their concentration gradients. They can’t diffuse out as fast as water, so their concentrations in the tubular fluid increase. Urea diffuses at about half the rate that water does. Its concentration in urine is about 50x its concentration in plasma Tubular Secretion A number of things are actively transported into the lumen of the nephron (secreted) Some important members of this group are H+, K+, and many organic anions The organic anions include detoxified foreign compounds, including pharmaceuticals Plasma Clearance It’s usually easy to measure the rate at which something is excreted: measure its concentration in urine and the rate of urine production. The product = rate of excretion It’s useful to ask how much plasma contains the amount of some substance that appears in the urine per minute. That volume of plasma is called the plasma clearance of that substance. Plasma clearance = (Urine Conc’n x Urine Flow rate)/Plasma Conc’n The more efficiently the kidneys remove a substance from plasma, the higher the plasma clearance for that substance Inulin Clearance and GFR Inulin (NOT insulin) is a polysaccharide in artichokes, onions and garlic. It is freely filtered in the glomerulus, so it enters the lumen of the nephron at the same concentration it has in plasma Inulin is neither reabsorbed (passively or actively), nor secreted into the lumen of nephrons. Therefore, the amount of inulin in the urine is the amount that entered the lumen of the nephron The amount of inulin that entered the nephron per minute is the plasma inulin concentration x the volume of plasma filtered per min Hey! Wait a minute! Isn’t the volume of plasma filtered per minute the GFR? Indeed, it is. So inulin clearance = GRF. That’s how GFR was first measured. There’s usually no inulin in plasma, but other ways of measuring GFR have been worked out. The most common is to measure creatinine clearance. Creatinine is a normal plasma constituent, is freely filtered, very weakly reabsorbed and not secreted. Its plasma clearance is a pretty good approximation of GFR. P-Aminohippuric acid (= PAH) is a compound that’s freely filtered, not reabsorbed, but actively secreted into the lumen of the nephron so vigorously that nearly all is removed from plasma. Therefore, PAH clearance = renal plasma flow. Since plasma is about 50% of the volume of blood, knowing renal plasma flow means we also know renal blood flow The numbers that I have been casually tossing around (GFR = 125 ml/min; renal blood flow = 1200 ml/min; etc.) are all traced to measuring inulin and PAH clearances. Note that the kidneys receive about 20% of cardiac output Long Term Regulation of Arterial Pressure Renal Function Curve Regulation of Urine Volume You might recall that I said juxtamedullary nephrons have a special function. Now I’ll tell you what it is. In these nephrons, peritubular capillaries are long, straight vessels that follow the loops of Henle into the full depth of the renal medulla. They’re called vasa recta (= straight vessels). Some important properties of the loop of Henle are: 1. Descending (thin) limb is highly permeable to water, doesn’t pump sodium much. 2. Ascending (thick) limb has vigorous sodium pump, very low water permeability. Let’s do a little thought experiment. Pretend that all the fluids in this system (tubular fluid, interstitial fluid, and plasma) are equilibrated, none is moving, sodium pumps aren’t running Therefore, osmolarity everywhere is the same, about 310 mOsm Let’s start the fluid flowing in the lumen of the nephron and turn on the sodium pump in the ascending limb of the loops of Henle. The result? The interstitial fluid osmolarity around the loops of Henle will go up. Result of that? Osmolarity in tubular fluid in descending limbs will go up. Result of that? Sodium concentration in next bit of fluid entering ascending limb will be higher than it was. Result of that? Sodium pump in ascending limb will reabsorb sodium faster. Therefore, osmolarity of interstitial fluid will increase even more, further increasing osmolarity in tubular fluid in descending limb, further increasing rate of sodium reabsorption in ascending limb. This is a positive feedback loop. If it continues indefinitely, all the sodium on the planet will eventually be in the interstitial fluid in someone’s kidneys. Why doesn’t that happen? Because blood is flowing in the vasa recta, and sodium (high interstitial fluid level) diffuses into it. At some point, the rate at which sodium is lost by diffusion and the rate at which it’s reabsorbed from the lumen become equal. At that point, the system is stable. The diffusion of sodium into the vasa recta, the pumping of sodium from the lumen of the ascending limb of the loop of Henle, and diffusion between the medullary and cortical interstitial spaces results in a stable osmotic gradient in the renal medulla. Near the cortex, where the high blood flow prevents it from changing, all the fluids are about 310 mOsm Deep in the medulla, the osmolarity is around 1200 mOsm A stable gradient exists between those two extremes. So, as we go deeper and deeper into the medulla, the osmolarity progressively increases from 310 to 1200 mOsm So what? Be patient, I’ll get to that. Countercurrent Multiplication The stable osmotic gradient in the renal medulla is only possible because all of the following are true: 1. Descending limb of loop of Henle is highly permeable to salt and water 2. Ascending limb of loop of Henle has highly active sodium pump 3. The two limbs of the loop of Henle are close to each other 4. Fluid flows in opposite directions in the two limbs 5. Blood flow in the vasa recta is sluggish Interacting fluids flowing in opposite directions in parallel pipes is called countercurrent flow. The mechanism by which an osmotic gradient is created in the renal medulla is called the countercurrent mechanism So what? Every collecting duct passes through the osmotic gradient created by only 20% of the nephrons. If collecting ducts are very permeable to water, they’ll lose about 75% of their volume and will become 1200 mOsm instead of 310 mOsm. If collecting ducts are impermeable to water, the fluid leaving them (urine) will have the same volume and osmolarity as the fluid that entered them (about 310 mOsm). Therefore, if there was a way to control collecting duct permeability to water, we could control volume of fluid lost in urine (and, as an incidental effect, the urine osmolarity) Good news! There is a way to do it. Antidiuretic Hormone Remember the hypothalamus? It has osmoreceptors that monitor the osmolarity of plasma. When plasma osmolarity is above normal (during dehydration), the osmoreceptors secrete a hormone, antidiuretic hormone (= ADH). Antidiuresis = reduced urine production. ADH increases collecting duct water permeability, thus, more water reabsorption. Result is lower volume of more concentrated (darker) urine. Low ADH levels let collecting ducts remain pretty impermeable to water. Hence, larger volumes of urine, which is more dilute. This is the most important mechanism for regulating extracellular fluid volume, which is how we regulate arterial pressure over the long term.