APPROACH TO WIDE QRS COMPLEX TACHYCARDIA
advertisement

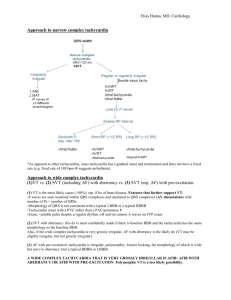
WIDE COMPLEX TACHYCARDIA Dr.Pradeep Sreekumar Definitions Wide QRS complex tachycardia is a rhythm with a rate of ≥100 b/m and QRS duration of ≥ 120 ms VT – Three or more consequtive ventricular beats with rate of 100/minute or more SVT- Tachycardia requiring participation of structures above bundle of His. LBBB morphology-QRS complex duration ≥ 120 ms with a predominantly negative terminal deflection in lead V1 RBBB morphology-QRS complex duration ≥ 120 ms with a predominantly positive terminal deflection in V1 Why QRS is wide? A widened QRS (≥120 msec) occurs when ventricular activation is abnormally slow Arrhythmia originates outside of the normal conduction system (ventricular tachycardia) Abnormalities within the His-Purkinje system (supraventricular tachycardia with aberrancy). Pre-excited tachycardias: supraventricular tachycardias with antegrade conduction over an accessory pathway into the ventricular myocardium. SVT (20%) VT (80%) Stewart RB. Ann Intern Med 1986 Causes of wide QRS complex tachycardia Supraventricular tachycardia - with prexsisting BBB - with BBB due to heart rate (aberrant conduction) - antidromic tachycardia in WPW syndrome Ventricular tachycardia Other causes.. Hyperkalemia Acidosis Antiarrhythmics-IA,IC Ventricular pacing Functional Bundle Branch Block Functional aberration results from sudden change in cycle length when parts of the His-Purkinje system are partially or wholly inexcitable Functional RBBB more common. Linking phenomenon Mechanism for perpetuation of functional anterograde bundle branch block due to repetitive transseptal retrograde concealed penetration by impulses propagating along the contralateral bundle. Linking: a dynamic electrophysiologic phenomenon in macroreentry circuits,Michael h. lehmann et al, Circulation. 1985;71:254-265 LINKING PHENOMENON AVRT Orthodromic AVRT – Antegrade conduction :AVnode Retrograde conduction : Accessory pathway. Wide QRS is produced only if aberrant conduction (rate related or preexisting BBB) Antidromic AVRT – antegrade conduction over the accessory pathway and retrograde conduction over the AV node . AVRT Mahaim fibre mediated tachycardia Antegrade conduction : Mahaim pathway Retrograde LBBB Left conduction:AV node morphology axis deviation Pre-excitation during sinus rhythm is uncommon Bundle Branch Reentrant VT RBBB morphology wide QRS tachycardia VT Structurally normal heart LVOT VT Fasicular VT Abnormal heart LV myocardial VT Bundle Branch Reentrant VT SVT SVT with pre existing RBBB SVT with functional RBBB LBBB morphology wide QRS tachycardia VT Structurally normal heart RVOT VT Abnormal heart Right ventricular myocardial VT ARVD SVT Mahaim fibre mediated tachycardia SVT with LBBB Unique clinical challenge Diagnosing the arrhythmia is difficult — Diagnostic algorithms are complex and imperfect. Urgent therapy is often required — Patients may be unstable at the onset of the arrhythmia or deteriorate rapidly at any time. Risks associated with giving therapy for an SVT to a patient who actually has VT SVT vs VT Clinical history Age - ≥ 35 ys → VT (positive predictive value of 85%) Underlying heart disease Previous MI → 90% VT Pacemakers or ICD Increased risk of ventricular tachyarrhythmia Medication Drug-induced tachycardia → Torsade de pointes Diuretics Digoxin-induced arrhythmia → [digoxin] ≥2ng/l or normal if hypokalemia Duration of the tachycardia — SVT is more likely if the tachycardia has recurred over a period of more than three years SVT vs VT AV dissociation -cannon A waves -variable intensity of S1 Termination of WCT in response to maneuvers like Valsalva, carotid sinus pressure, or adenosine favor SVT Maneuvers The response of the arrhythmia to maneuvers may provide insight to the mechanism of the WCT Carotid sinus pressure — Enhances vagal tone , depresses sinus and AV nodal activity Carotid sinus pressure Sinus tachycardia will gradually slow with carotid sinus pressure and then accelerate upon release. Atrial tachycardia or atrial flutter-the ventricular response will transiently slow. The arrhythmia is unaffected. Paroxysmal SVT frequently terminates with carotid sinus pressure. VT Unaffected by vagal maneuvers such as carotid sinus pressure or valsalva May slow or block retrograde conduction. Exposes AV dissociation Rarely, VT terminates in response to carotid sinus pressure. Laboratory tests The plasma potassium and magnesium concentrations (hypokalemia and hypomagnesemia predispose to the development of ventricular tachyarrhythmias. ) Digoxin, quinidine, or procainamide levels-to rule out drug toxicity Chest x-ray Evidence suggestive of structural heart disease Evidence of previous cardiothoracic surgery Presence of a pacemaker or ICD. Rate Limited use in distinguishing VT from SVT. When the rate is approximately 150 beats per minute, atrial flutter with aberrant conduction should be considered. Ventricular rate > 200-suspect preexcitation tachycardia Regularity Marked irregularity of RR interval occurs in atrial fibrillation (AF) with aberrant conduction and polymorphic VT Axis A right superior axis (axis from -90 to ±180º)“northwest" axis, strongly suggests VT . (sensitivity 20%,specificity 96%) Exception -antidromic AVRT in Wolff-ParkinsonWhite (WPW) syndrome . Compared to the axis during sinus rhythm, an axis shift during the WCT of more than 40º suggests VT . In a patient with a RBBB-like WCT, a QRS axis to the left of -30º suggests VT. In a patient with an LBBB-like WCT, a QRS axis to the right of +90º suggests VT . QRS duration In general, wider QRS favors VT. In a RBBB-like WCT, a QRS duration >140 msec suggests VT In a LBBB-like WCT, a QRS duration >160 msec suggests VT In an analysis of several studies, a QRS duration >160 msec was a strong predictor of VT (likelihood ratio >20:1) . A QRS duration <140 msec does not exclude VT ( VT originating from the septum or within the HisPurkinje system may be associated with a relatively narrow QRS complex.) Concordance Concordance is present when the QRS complexes in all six precordial leads (V1 through V6) are monophasic with the same polarity. Either -entirely positive with tall, monophasic R waves, or entirely negative with deep monophasic QS complexes. If any of the six leads has a biphasic QRS (qR or RS complexes), concordance is not present. Negative concordance is strongly suggestive of VT exception:SVT with LBBB aberrancy may demonstrate negative concordance Positive concordance -also indicates VT exception: antidromic AVRT with a left posterior accessory pathway Presence of concordance strongly suggests VT (90 percent specificity) Absence is not helpful diagnostically (approximately 20 percent sensitivity) Higher specificity for Positive concordance compared to negative concordance(specificity 95% vs 90 %) Negative concordance Positive concordance AV dissociation AV dissociation is characterized by atrial activity that is independent of ventricular activity Atrial rate slower than the ventricular rate diagnostic of VT. Atrial rate that is faster than the ventricular rate SVTs. Absence of AV dissociation in VT AV dissociation may be present but not obvious on the ECG. The ventricular impulses conduct backwards through the AV node and capture the atrium ( retrograde conduction), preventing AV dissociation. Dissociated P waves PP and RR intervals are different PR intervals are variable There is no association between P and QRS complexes The presence of a P wave with some , but not all, QRS complexes Fusion beats Fusion beat-produced by fusion of two ventricular activation wavefronts characterised by QRST morphology intermediate between normal and fully abnormal beat. Fusion beats during a WCT are diagnostic of AV dissociation and therefore of VT. Low sensitivity(5-20%) Capture beats Capture beats, or Dressler beats, are QRS complexes during a WCT that are identical to the sinus QRS complex . Implies that the normal conduction system has momentarily "captured" control of ventricular activation from the VT focus. Fusion beats and capture beats are more commonly seen when the tachycardia rate is slower If old ecg available… Ideal QRS configuration between baseline and WQRST-suggest SVT(exception :bundle branch reentrant VT) Contralateral BBB patterns in baseline vs WQRST ECGs-suggest VT WQRST complexes narrower than baseline ECGsuggest VT(the baseline ecg must have a bundle branch block pattern) Also look for…. VPCs Evidence of prior MI QT interval ECG clues to any other structural heart disease SVT vs VT ECG criteria: Brugada algorithm Brugada P. Ciculation 1991 Step 1 Step 2 Step 3 Step 4: LBBB - type wide QRS complex VT SVT R wave >30ms notching of S wave small R wave V1 fast downslope of S wave > 70ms Q wave V6 no Q wave V1 in LBBB type QRS True LBBB R-R duration <- 30 msec Interval from QRS onset to S nadir ≤70 msec (85% of SVT –A) VT R >30 msec,QRS onset to S nadir>70 msec (sensitivity-0.78,specificity 0.85,positive predictive value 0.97) Notching and slurring of QRS complex –myocardial disease V6 in LBBB type QRS True LBBB Monophasic R with slow upstroke VT qR or QS pattern Step 4: RBBB - type wide QRS complex VT SVT rSR’ configuration V1 or R/S > 1 V6 qR (or Rs) complex monophasic R wave R/S ratio < 1 QS complex or V1 in RBBB type QRS Initial ventricular activation is independent of RBB. RBBB abberation affects only the latter QRS True RBBB rR’,rsR’,rSr’,rSR’ VT qR,Rsr’,monophasic R wave (Sensitivity 0.97,specificity 0.88) VT SVT V6 in RBBB type QRS RBBB abberation-small s wave. qRs or Rs pattern RBBB type VTVT from left ventricle-LV and RV voltage contributes to S qRS,qrS,rS,QS patterns seen “R/S ratio in V6 rule” R/S ratio in RBB type wide QRS tachycrdia less than one, favours VT Sensitivity-0.73 Specificity-0.79 Positive predictive value 0.9 Josephson’s sign Notching near the nadir of the S-wave Suggest VT Wellens Criteria • QRS width > 140 msec • Left axis deviation • AV dissociation • Configurational characteristics of the QRS morphology Ultrasimple Brugada criterion Joseph Brugada - 2010 R wave peak time in Lead II Duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) in lead II. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8) Pava LF, Perafán P, Badiel M, Arango JJ, Mont L, Morillo CA, and Brugada J. R-wave peak time at DII: a new criterion for differentiating between wide complex QRS tachycardias. Heart Rhythm 2010 Jul; 7(7) 922-6. Vereckei A, Duray G, Szénási G, Altemose GT, and Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J 2007 Mar; 28(5) 589-600. aVR algorithm Criteria looks ONLY at lead aVR (if answer is yes, then VT): 1. Is there an initial R wave? 2. Is there a r or q wave > 40 msec 3. Is there a notch on the descending limb of a negative QRS complex? 4. Measure the voltage change in the first (vi) and last 40 msec (vt). Is vi / vt < 1? Vereckei et al, Heart Rhythm 2008 Sensitivity Specificity PPV NPV Brugada 89% 73% 92% 67% Vereckei 97% 75% 93% 87% Vereckei A, Duray G, Szénási G, Altemose GT, and Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J 2007 Mar; 28(5) 589-600. Sensitivity & Specificity For VT 88% and 53% by aVR algorithm VT vs AVRT ECG criteria Brugada P. Ciculation 1991 THANK YOU…….