Anoectochilus formosanus
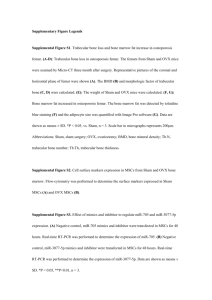
advertisement
1 2 The prebiotic arabinogalactan of Anoectochilus formosanus prevents ovariectomy-induced osteoporosis in mice 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Li-Chan Yanga, Ting-Jang Lua, Wen-Chuan Linb,* a Institute of Food Science and Technology, National Taiwan University, Taipei, Taiwan. School of Medicine, Graduate Institute of Basic Medical Science and Tsuzuki Institute for Traditional Medicine, China Medical University, Taichung, Taiwan b *Corresponding author: Department of Pharmacology, China Medical University, No. 91 Hsueh Shih Road, Taichung, Taiwan, R.O.C. Tel +886 4 22053366; fax +886 4 22053764 e-mail address: wclin@mail.cmu.edu.tw (W.C. Lin) 18 19 20 21 22 23 Keywords: Prebiotic; Arabinogalactan; Osteoporosis; Short chain fatty acids 1 ABSTRACT: 2 anti-osteoporosis and prebiotic properties in previous studies. In this study, these 3 bioactivities were verified and associated with an isolated type II arabinogalactan 4 (AGAF) in ovariectomized (OVX) mice model. Female ICR mice were OVX and 5 administrated AGAF (5 and 15 mg/kg) or inulin (400 mg/kg) orally for 3 weeks. 6 Streptomycin was used for blocking the bioactivities of AGAF. In results, AGAF 7 increased the level of fecal bifidobacteria, cecal soluble Ca and short chain fatty acids. 8 Comparing to OVX control group, AGAF improved bone mineral content, trabecular 9 bone volume, and the number of trabecular significantly. In RT-PCR analysis, AGAF 10 reduced the expression of tartrate-resistant acid phosphatase, cathepsin K, and 11 osteocalcin. Streptomycin inhibited both anti-osteoporosis and prebiotic effects of 12 AGAF. In vitro experiments revealed butyrate, not AGAF could activate osteoblasts 13 and inhibit osteoclasts differentiation. In conclusion, this study showed AGAF 14 prevented bone loss in OVX mice through prebiotic effects in vivo and in vitro. 15 Anoectochilus formosanus (Orchidaceae) has exhibited 1 2 1. Introduction 3 4 Osteoporosis is the most common skeletal problem caused by aging, especially in 5 postmenopausal women (Pietschmann, et al., 2009). The deficiency of ovarian 6 hormones is a major factor in postmenopausal osteoporosis. Bone loss may lead to 7 related fractures and high medical costs. Hormone supplements and bisphosphonate 8 are common therapies for osteoporosis; however, these therapies have several side 9 effects. For example, hormone supplements increase the risk of cardiovascular disease 10 and breast cancer; the risk of bisphosphate includes osteonecrosis of the jaw and 11 atypical femur fractures (de Villiers & Stevenson, 2012; Khosla, et al., 2012). The 12 lack of reliable and effective therapies to cure osteoporosis-related fragility fractures 13 remains an important global issue (Datta, 2011). Previous studies have indicated that 14 certain nutritional factors, such as fruit, prebiotics, and minerals, can increase bone 15 mineral density in people diagnosed with osteoporosis (Devareddy, et al. 2008; Chen, 16 et al., 2006; Stransky & Rysava, 2009). Nutrition could prevent and treat osteoporosis 17 with fewer side effects than medicine therapies (Stransky & Rysava, 2009). Prebiotics 18 are food component not absorbed or digested in the small intestine but are fermented 19 by microbiota in the large intestine (Roberfroid, 2005). Several prebiotics, such as 20 inulin, galactooligosaccharides, and fructooligosaccharides, are thought to improve 21 bone health (Roberfroid, 2005;Weaver, 2005). The microbial fermentation products of 22 prebiotics, such as short chain fatty acids (SCFA), are responsible for the increase of 23 calcium (Ca) absorption in the large intestine. The high concentration of SCFA in the 24 cecum leads to a decrease of cecal pH, which increases the concentrations of soluble 25 Ca (Coxam, 2007). In addition, butyrate, one of the SCFA, belongs to a new class of 26 antiosteoporotic agents that may be useful in the treatment of bone loss (Katono, et al., 1 2008; Rahman, et al., 2003; Schroeder & Westendorf, 2005). Furthermore, numerous 2 reports have indicated that the ingestion of prebiotics or fermentable dietary fibers 3 might be helpful in preventing osteoporosis (Coxam, 2007; Mitamura, et al., 2004). 4 Anoectochilus formosanus (Orchidaceae) is an important ethnomedicinal plant in 5 Taiwan. It has been popularly used as a nutraceutical herbal tea in Taiwan and other 6 Asian countries (Du, et al., 2008). In Taiwan, the aqueous extracts of A. formosanus 7 have been certified as health food for hepatoprotection bioactivity and showed safety 8 in the 13 week oral toxicity study in rats. In additional, Chang, et al. have indicated 9 that A. formosamus plants cultivated by artificial are safe for use as an herbal 10 medicine (Chang, et al., 2007). Several reports have shown that crude extracts of A. 11 formosanus could ameliorate osteoporosis in the ovariectomized (OVX) rat model 12 (Shih, et al.,2001; Masuda, et al., 2008; Yang, et al., in press). Masuda et al. shows 13 that aqueous extracts of A. formosanus suppress bone loss caused by estrogen 14 deficiency by inhibiting osteoclast formation (Masuda, et al., 2008). Our previous 15 study also shows that water extracts of A. formosanus prevent bone loss in rats caused 16 by OVX (Yang, et al., in press). In our previous studies, an indigestible 17 polysaccharide isolated from A. formosanus was shown to be a potent prebiotic (Yang, 18 et al., 2012). the indigestible polysaccharide of A. formosanus was mainly composed 19 of type II arabinogalactan (AGAF). Water extracts of A. formosanus could enhance 20 the level of cecal SCFAs and increase the number of fecal bifidobacteria in rats (Yang, 21 et al., 2012). Therefore, it was suggested that the anti-osteoporosis activity of A. 22 formosanus may be regulated by its prebiotic effect. This study examines the 23 anti-osteoporosis effects of AGAF in OVX mice, and investigates the relationship of 24 prebiotic properties and anti-osteoporosis activity. 25 1 2. Materials and methods 2 3 2.1. Arabinogalactan preparation 4 Cultured A. formosanus was purchased from Yu-Jung Farm (Pu-Li, Taiwan). Fresh 5 plants were homogenized with distilled water, and then partitioned with ethyl acetate 6 (Tedia Company, OH, USA). The aqueous extracts of A. formosanus were added with 7 a 4-fold volume of 95% ethanol to precipitate crude polysaccharides, and then the 8 crude polysaccharide was treated with α-amylase, protease and protease (Megazyme, 9 Wicklow, Ireland) to remove starches and proteins. After enzymic treatment, AGAF 10 was preserved in ethanol until use. 11 The identity and content of type II arabinogalactan in AGAF (> 80%) were 12 analyzed by precipitation with β-glucosyl yariv reagent according to a previous study 13 (Yang et al., 2012). For an in vivo experiment, AGAF was dissolved in distilled water, 14 and concentrations of 0.5 and 1.5 mg/mL were prepared. 15 The yield rate of AGAF was 0.15% from fresh plants. Chemical analyses showed 16 that AGAF contained 95.5% carbohydrates and 1.0% protein. AGAF is mainly 17 composed of a (1→3)-β-D-galactan backbone with a (1→6)-β-D-galactan side chain, 18 and is a type II arabinogalactan with an average molecular weight of 29 kDa. The 19 monosaccharide composition of AGAF was arabinose, galactose, glucose, and 20 mannose with a ratio of 22.4:56.5:15.4:5.4 (Yang, et al., 2012). 21 22 2.2. Animals 23 Eight-week-old female ICR mice were purchased from BioLASCO Co., Ltd. (Yi-Lan, 24 Taiwan). The experimental animals received humane care, and the study protocols 25 complied with the institutional guidelines of China Medical University for the use of 1 laboratory animals. The animals were housed in an air-conditioned room (21–24 °C) 2 under 12 h of light (8:00 a.m. – 8:00 p.m.), and were allowed free access to food 3 pellets and water throughout the study. 4 5 2.3. Anti-osteoporosis effects of AGAF on OVX mice. 6 The experiments were performed on 40 female ICR mice. Bilateral OVX operation 7 was performed under pentobarbital anesthesia (50 mg/kg) on the mice according to 8 the procedure described before (Idris, 2012). Briefly, the mice were laparotomized to 9 excise both ovaries clearly. The mice in the sham-operated group received anesthesia 10 and a laparotomy as OVX operation, and were then sutured without removing their 11 ovaries (Idris, 2012). After 3 days of adaptation after the surgery, the OVX mice were 12 randomly divided into four groups, and were orally administered H2O, AGAF (5, 15 13 mg/kg), or inulin (Alfa Aesar, Heysham, UK) for the positive control for 3 weeks. 14 The sham-operated group was orally treated with H2O. Each group contained 8 mice. 15 The body weight of each animal was measured once a week until the final day of 16 administration. 17 18 2.4. Assessment of prebiotic effect of AGAF 19 On day 7 after AGAF treatment, fresh feces were collected for analysis for 20 bifidobacteria. Fresh feces were homogenized with 0.1% peptone diluent, followed by 21 serial decimal dilutions. The number of bifidobacteria was counted on Bifidobacteria 22 iodoacetate medium-25 agar after incubation at 37 ℃ for 48 h under anaerobic 23 conditions (95% N2, 3% CO2, and 2% H2) (Munoa & Pares, 1988). After incubation, a 24 single colony was counted, and the results were expressed as the log values of the 25 CFUs per gram of wet weight of feces. 1 2.5. Ca concentrations and SCFA 2 After the mice were sacrificed, the ceca were removed and weighed immediately. The 3 cecal contents were collected. The cecal walls were then flushed with 0.9% saline, 4 blotted dry with filter paper, and weighed, and were then stored at -80 ℃ for reverse 5 transcription-polymerase chain reaction (RT-PCR) analysis. The cecal contents were 6 stored at -80 ℃ until SCFA determination using HPLC analysis (Niven, et al., 2004). 7 For SCFA analysis, the cecal content samples were defrosted on ice, and were diluted 8 with 0.0085N sulfuric acid. The cecum samples were shaken and centrifuged at 12000 9 × g for 20 min. The supernatant was diluted to proper concentrations for HPLC 10 analysis. The SCFAs were analyzed by a Transgenomic ICSep Transgenomic (300 × 11 7.8 mm, Omaha, NE, USA) at 65 °C, and eluted with 0.0085N sulfuric acid at a flow 12 rate of 0.4 mL min-1. The peaks were detected by a Shodex RI-71 detector (Showa 13 Denko, Tokyo, Japan). 14 15 2.6. Bone Ca content 16 Soft tissues were removed from the lumbar vertebra, and were immersed in a mixed 17 solvent (chloroform: methanol = 2:1, Showa, Tokyo, Japan) to remove bone lipids 18 subcutaneously (Honda, 2001). De-fatty lumbar vertebrae were incinerated at 1000 °C 19 for 12 h for ashing. Bone ash was weighed and solved in 6N HCl (Wako, Osaka, 20 Japan) for determination of Ca with the o-cresolphthalein complexone method with 21 commercial kits (Randox, Crumlin, UK). Values were expressed as milligrams of Ca 22 of bone dry weight. 23 24 2.7. Microcomputed tomography (microCT) analyses 25 The right femurs of the mice were preserved in 75% alcohol until scanning. The bone 1 microarchitecture of the distal right femoral metaphysis was measured using a 2 microtomography scanner (SkyScan 1076, Kontizh, Belgium), with an isotropic 3 resolution of 17 m in all 3 spatial dimensions. To analyze the interest volume of 4 trabecular, 100 slices were selected from the edge of distant direction to the proximal 5 direction. The region of interest volume was analyzed without the cortical bone. The 6 bone and tissue volumes were measured directly from the original 3-dimensional 7 images, and the trabecular volume fraction (bone volume/tissue volume, %) was 8 normalized to compare samples of different sizes. The other examined parameters of 9 the trabecular structure were trabecular thickness, trabecular number, and trabecular 10 separation, which were calculated directly from the 3-dimensional images. 11 12 2.8. RT-PCR analysis 13 Total RNA was extracted with Trizol (Invitrogen, CA, USA) from the tibia and cecal 14 walls, followed by acid guanidinium thiocyanate-phenol-chloroform extraction, as 15 described by Chomczynski and Sacchi (1987). A 3 g sample of total RNA was 16 subjected to reverse transcription with moloney murine leukemia virus reverse 17 transcriptase in a 50 L reaction volume. The cDNA was amplified by PCR. The 18 primers used for cecal wall RNA extract were CaBP and glyceraldehyde-3-phosphate 19 dehydrogenase 20 CAGAACCGAAGACTAGCGCA-3’ and 21 -3’(product 5’-TGTGTCCGTCGTGGATCTGA-3’ 22 5’-CCTGCTTCACCACCTTCTTGA-3’(product size, 76 bp), respectively. The 23 primers for mice tibia RNA extract were TRAP, 5’-CCAATGCCAAAGAGATCGCC 24 -3’ and 5’- TCTGTGCAGAGACGTTGCCAAG-3’(product size, 216 bp), Cathepsin 25 K , size, (GAPDH) 283 5’- as bp),and internal standard and were 5’- 5’-GCACAAAACAAAGTGGGTGC CTGCCCATAACCTGGAGG-3’ and and 5’- size, 230 bp), OCN, 5’- 1 GCCCTGGTTCTTGACTGG-3’(product 2 AGACCGCCTACAAACGCATC-‘3’ 3 -3’(product size, 113 bp), Runx2, 5’-CCGAGAAGTGGTTCCCGGTCCTG-3’ and 5’- 4 CGACAGATCTGGAGCCTGCGGA-3’(product size, 173 bp), and GAPDH as 5 internal standard. . Electrophoresis was performed on 2% agarose gels in a 0.5X TBE 6 buffer (Amersco, OH, USA) for PCR products, and each lane was loaded with a fixed 7 volume of the sample. PCR products were visualized using ethidium bromide 8 staining. and 5’-ACAGGGAGGATCAAGTCCCG 9 10 2.9. Plasma bone markers 11 At the end of the experiment, the mice were sacrified, and their blood was drawn with 12 heparin. The plasma was separated from the blood samples by centrifugation at 2000 13 × g for 10 min. The plasma was stored at -30 °C until assay. The plasma osteocalcin 14 (OCN) were measured by commercial enzyme-linked immunosorbent assay (ELISA) 15 kits (Biomedical Technologies Inc., Stoughton, MA, USA), and the plasma 16 carboxy-terminal collagen cross-links (CTx) were analyzed using ELISA kits 17 (Immunegiagnostic Systems, AZ, USA). 18 19 2.10. Effects of AGAF on OVX mice with streptomycin supplement 20 40 female ICR mice were treated with sham operations or OVX, and OVX mice were 21 allocated into groups that were H2O, AGAF (15 mg/kg po. daily) with or without 22 streptomycin sulfate (SM; Sigma Aldrich, MO, USA) treatment for 3 weeks. Each 23 group contained eight mice. SM was dissolved in the drinking water at a 24 concentration of 2 mg/mL (Asahara, 2001). The sham-operated group was orally 25 administrated H2O. The body weight of each mouse was recorded every week until 1 the end of the experiment. The mice were assessed for prebiotic activity in vivo. At 2 the end of the experiment, mice femurs were removed for microCT analyses. 3 4 2.11. In vitro assay of alkaline phosphatase activity on murine osteoblast MC3T3-E1 5 cells 6 The cells of murine osteoblast MC3T3-E1 were grown in Dulbecco’s modified 7 Eagle’s medium (DMEM, Hyclone, UT, USA) supplemented with 10% (v/v) FBS 8 (Hyclone, USA), 100 U/mL penicillin, and 100 mg/mL streptomycin. Incubation was 9 conducted in a CO2 incubator (5% CO2, 95% air) at 37 °C. The cells were 10 subcultured every 2 or 3 days by 0.25% (w/v) trypsin plus a 0.02% (w/v) 11 ethylenediaminetetraacetic acid tetrasodium salt solution (Gibco, NY, USA). 12 For the alkaline phosphatase (ALP) activity assay, the MC3T3-E1 cells were 13 seeded in 48-well plates (104 cells/well) containing DMEM in addition to 10% FBS 14 (Iwami & Moriyama, 1993). After the cells attached to the bottom of the wells, the 15 culture medium was changed to DMEM + 10% FBS medium containing 10 mM 16 disodium β-glycerophosphate (Sigma Aldrich), 0.15 mM ascorbic acid (Sigma 17 Aldrich), and 10-8 M dexamethasone (Sigma Aldrich) (Isama & Tsuchiya, 2003). 18 Simultaneously, different concentrations of sodium butyrate or AGAF were added 19 to the culture medium in the well. On day 6 after cultivation, the cells were washed 20 twice with phosphate buffered saline and harvested in a 200 μL/well of a lysis buffer 21 (pH 8.2, 10 mM Tris-HCl, 2 mM MgCl2, and 0.05% Triton X-100). Cells were lysed 22 through an ultrasonic processor (Vibra-Cell, Sonics & Materials, CT, USA) with 30 J 23 in energy. Aliquots were reserved for protein analysis. A total of 300 μL of 8 mM 24 p-nitrophenyl phosphate (Sigma Aldrich) in a 0.1 M sodium carbonate buffer (pH 10) 25 containing 1 mM MgCl2 were added to the reaction mixture, which was incubated at 1 37 °C for 30 min. The reaction was stopped by adding 50 μL of 1.0 N NaOH/well.26 2 The yellow sample solutions containing p-nitrophenol for the reaction product were 3 measured at 405 nm using a microplate reader. A standard curve was prepared using 4 p-nitrophenol phosphate. The total protein contents of cell lysates was measured by a 5 Bradford reagent (Sigma Aldrich) using albumin for the standard (Bradford, 1976). 6 7 2.12. In vitro Osteoclasts differentiation from murine macrophage RAW264.7 cell line 8 RAW264.7 cells were maintained in an α-modified Eagle’s medium (Hyclone), 9 supplemented with 10% FBS (Gibco, CA, USA), 100 U/mL penicillin, and 100 10 mg/mL streptomycin and L-glutamine (Biological industry, Kibbutz Beit-Haemek, 11 Israel). Cells were cultured at a density of 2 × 10 3 cells/mL in a 24-well plate in the 12 presence of a receptor activator of nuclear factor kappa B ligand (RANKL) for 5 days 13 (Rahman, et al., 2003). RAW264.7 cells were incubated with different concentrations 14 of sodium butyrate or AGAF to examine their effects on osteoclast differentiation. On 15 day 5, cells were treated with 4% formaldehyde solution for 10 min, and then stained 16 to obtain the tartrate-resistant acid phosphatase (TRAP) of the osteoclasts. TRAP 17 staining was applied to measure the presence of osteoclasts, and stained with a 18 standard kit (387A-1 kit, Sigma-Aldrich). The TRAP-positive multinucleated 19 osteoclasts (least 3 nuclei) were counted (Parfitt, et al. 1987). 20 21 2.13. Statistical analysis 22 The results were expressed as mean SD. All experimental data were analyzed using 23 one-way analysis of variance (ANOVA) with the Duncan multiple-range test. Values 24 of p < 0.05 were considered statistically significant. 25 1 2 3 3. Results 4 The number of fecal bifidobacteria was different between the sham and OVX-H2O 5 group. The OVX treatment caused a 9.1% decrease in the number of bifidobacteria for 6 the OVX mice than in the sham group. Administration of AGAF for 7 days led to a 7 20.7% (5 mg/kg) and 21.2% (15 mg/kg) increase in bifidobacteria in the stool 8 compared to the OVX-H2O group (Table 1). In addition, inulin treatment also led to a 9 15.2% increase in the number of fecal bifidobacteria over the OVX-H2O group. 3.1. Assessment of prebiotic effect of AGAF 10 11 3.2. Cecal Ca concentrations and SCFA 12 The cecal Ca concentrations in the OVX-H2O group and sham group were equal. For 13 the level of cecal Ca concentration, the AGAF administrated groups had 35.1% (5 14 mg/kg) and 42.7% (15 mg/kg) greater levels than the OVX-H2O group; administrated 15 with inulin were 39.8% greater than OVX-H2O group significantly (Table 1). 16 The results of SCFA analyses are shown in Table 1. Concentrations of butyric 17 acid in the sham group and OVX-H2O group have significant differences. The 18 OVX-H2O group had a decrease in the level of butyric acid of 12.1% compared to the 19 sham group. In addition, no differences in lactic acid, acetic acid, and propionic acid 20 were observed between the sham group and the OVX-H2O group. The analysis 21 showed significantly higher concentrations of acetic acid, propionic acid, and butyric 22 acid in the OVX-AGAF group (15 mg/kg) compared to the OVX-H2O group (26.3%, 23 66.0%, and 57.7% increases, respectively). The OVX-inulin group showed increases 24 in propionic acid and butyric acid of 53.6% and 16.4% compared to the OVX-H2O 25 group. In this study, total SCFA is the amount of lactic acid, acetic acid, propionic 26 acid, and butyric acid; no differences were observed between the sham and OVX-H2O 1 groups. Moreover, the OVX mice administered AGAF led to a 21.0% (5 mg/kg) and 2 31.25% (15mg/kg) increase; inulin led to a significant 12.8% increase in the total 3 SCFAs in the ceca of the OVX mice, compared to the OVX-H2O group. 4 5 3.3. Bone Ca content 6 The amount of Ca in the lumbar vertebrae was determined using o-cresophthalein 7 complexone. The total Ca content and Ca ratio of lumbar vertebrae was calculated. 8 The results were showed that OVX treatment reduced the Ca content by 11.4% (14.0 9 ± 1.3 mg) and the Ca ratio by 16.9% (12.3 ± 0.6%) in the lumbar vertebrae compared 10 to sham group (15.8 ± 1.0 mg in Ca content; 14.8 ± 0.8% in Ca ratio). The results of 11 AGAF treatment (5 mg/kg) were 13.3 ± 0.9 mg in Ca content and 13.1 ± 0.1% in the 12 Ca ratio, and shown no significant difference compared to OVX-H2O group. 13 Administration of AGAF (15 mg/kg) caused a significant 13.6% increase in the Ca 14 content (15.9 ± 0.4 mg), and a 14.6% increase in the Ca ratio (14.1± 0.1%); however, 15 administration of inulin increased the Ca ratio (13.8 ± 0.5%) only, compared to the 16 OVX-H2O group. Bone Ca content of inulin treatment group was 14.9 ± 1.9 mg and 17 displayed a minor increase to OVX-H2O group. 18 19 3.4. MicroCT analyses 20 The OVX procedure caused significant decreases in the trabecular bone volume ratio 21 (12.6%), trabecular number (11.1%), and trabecular thickness (30.6%) in the OVX 22 group compared to the sham group (Figs. 1B, 1C). Although the trabecular separation 23 was 107.0% in the OVX-H2O group compared to the sham group, the data showed no 24 significant difference (Fig. 1C). These results show that OVX induced a loss of 25 trabecular bone in the femurs of the mice (Fig. 1A). Treatment of AGAF (15 mg/kg) 1 and inulin led to a significant 10.9% and 3.5% increase in the loss in trabecular bone 2 volume, respectively. OVX mice administered AGAF had a 24.5% (5 mg/kg) and 3 30.0% (15 mg/kg) increase in trabecular thickness, respectively. Treatment with inulin 4 caused an increase of 12.2% in trabecular thickness. The trabecular number and 5 separation was unaffected in the AGAF or inulin groups. 6 7 3.5. RT-PCR analysis 8 The expression of Ca-binding protein (CaBP) in cecal mucosal cells is shown in Fig. 2. 9 The gene expression of CaBP was significantly decreased in the OVX-H2O group 10 compared to the sham-H2O group (31.6% decrease). The expression of CaBP were 11 1.6- and 2.0-fold increased by the administration of AGAF (5, 15 mg/kg), and rose 12 1.8-fold in the inulin group compared to the OVX-H2O group. 13 Figure 2B showed that all data were presented as relative expressions compared to 14 GAPDH, which was used as the internal control. For mRNA expression of the tibia, 15 the relative expression of osteoclast-related genes involving TRAP, cathepsin K, and 16 osteoblast-associated genes, including OCN, was significantly upregulated by the 17 OVX operation compared to in the sham operation. The expression of TRAP, 18 cathepsin K, and OCN were 4.4-fold, 3.0-fold, and 1.8-fold higher than in the sham 19 group, respectively (Fig. 2). Administration of AGAF (5, 15 mg/kg) and inulin could 20 significantly inhibit the expression of TRAP and cathepsin K compared to the 21 OVX-H2O group. Both AGAF and inulin treatments could prevent the increased 22 expression of OCN. The expression of OCN in the AGAF administrated groups were 23 83.1% (5 mg/kg) and 67.6% (15 mg/kg), and 70.4% in the inulin administrated group 24 compared to the OVX-H2O group. There was no significant difference in the 25 expression of Runx2 between the OVX-H2O and sham groups (Fig. 2). However, only 1 AGAF treatment (15 mg/kg) could significantly suppress the expression of Runx2 2 (72.1%) compared to the OVX-H2O group. 3 4 3.6. Plasma bone markers 5 The results of the plasma CTx assay are shown in Fig. 3A. The concentration of CTx 6 was significantly increased in the OVX-H2O group over the sham group. Treatments 7 of AGAF (15 mg/kg) and inulin in the OVX mice caused decreases of 31.0% and 8 25.3% of the plasma CTx level, respectively. In the OCN assay, the OCN 9 concentration in the OVX-H2O group was 25% higher than in the sham group (Fig. 10 2B). The AGAF treatment (15 mg/kg) significantly lowered the level of OCN by 11 9.3% compared to the OVX-H2O group. 12 13 3.7. Effects of AGAF on OVX mice with streptomycin supplement 14 The assay for prebiotic effects was determinate by fecal number of bifidobacteria on 15 day 7 and day 21 during the experimental period. After 7 days treatment, the number 16 of bifidobacteria (log10CFU/g) showed no difference in sham and OVX-H2O group 17 and was 6.7 ± 0.7 and 6.2 ± 0.1, respectively. The mice administrated AGAF (15 18 mg/kg) has 24.0% increase in the number of bifidobacteria (7.6 ± 0.3 log10CFU/g) 19 compared to OVX-H2O group significantly. However, continuous treatment of mice 20 with SM in the drinking water (2 mg/mL) for 7 days resulted in the fecal 21 bifidobacteria decreasing to an undetectable level. The fecal bifidobacteria counts in 22 OVX-H2O-SM and OVX-AGAF-SM group was < 2.0 and 4.1 ± 2.5 log10CFU/g, 23 respectively. 24 The results of prebiotic assay on day 21 were similar to the results of day 7. The 25 bifidobacteria count of sham, OVX-H2O, OVX-AGAF groups was 6.7 ± 0.1, 6.3 ± 0.2 1 and 7.8 ± 0.4 log10CFU/g feces, respectively. The administration of AGAF promoted 2 the number of bifidobacteria in 24.1% increase than OVX-H2O significantly. In 3 additional, SM also blocked the prebiotic effects of AGAF on day 21. The results of 4 fecal bifidobacteria in OVX-H2O-SM and OVX-AGAF-SM group were showed as 5 undetectable and 3.7 ± 1.6 log10CFU/g, respectively. Though the bifidobacteria 6 number of OVX-AGAF-SM group on day 21 was minor than on day 7, but the data 7 was not significant difference. 8 The levels of plasma bone markers, including CTx and OCN, were shown in Fig. 9 3B. CTx and OCN in the OVX-H2O group increased 2.5-fold and 1.25-fold compared 10 to the sham group, respectively. No differences were noted between the OVX-H2O 11 group and the OVX-H2O+SM group. Administration of AGAF (15 mg/kg) could 12 prevent the increase of CTx and OCN. However, AGAF administration combined 13 with SM did not affect the levels of CTx or OCN. 14 Mice femurs were assessed for microCT. The OVX operation caused significant 15 reductions in trabecular bone volume, trabecular number, and the trabecular thickness 16 of the femur compared to the sham group. Trabecular separation showed no difference 17 among the groups. Adding SM to the drinking water of the OVX mice did not affect 18 the trabecular parameters, compared to the OVX-H2O group without SM. The results 19 showed that administration of AGAF (15 mg/kg) could improve the trabecular bone 20 volume and trabecular thickness of the femur in OVX mice. Treatment of AGAF with 21 SM caused no difference in trabecular bone volume, trabecular number, trabecular 22 thickness, or trabecular separation, compared to the OVX-H2O group (Table 2). 23 24 3.8. In vitro assay of ALP activity on murine osteoblast MC3T3-E1 cells 25 The ALP activity assay was used to evaluate the differentiation of MC3T3-E1. ALP is 1 a representative enzyme that can indicate osteoblast differentiation (Isama & Tsuchiya, 2 2003). Butyric acid is the most changeable SCFA in the cecum in the in vivo prebiotic 3 experiment. In the presence of different concentrations of butyric acid, MC3T3-E1 4 cells produced increasing ALP activity at concentrations from 0.5 mM to 1.0 mM 5 sodium butyrate after 6 days of treatment (Fig. 4A). No obvious differences were 6 observed in the sodium butyrate concentration of 0.1 mM and for all concentrations of 7 AGAF (Fig. 4A). It appears that sodium butyrate can effectively enhance the ALP 8 activity of MC3T3-E1, but AGAF cannot. The ALP activity results strongly suggest 9 that osteoblastic differentiation could be efficiently stimulated in the presence of 10 sodium butyrate. 11 12 3.9. In vitro osteoclasts differentiation from murine macrophage RAW264.7 cell line 13 The effects of sodium butyrate and AGAF on the osteoclast formation in the murine 14 macrophage cell line RAW264.7 cells were examined. On day 5, the number of 15 TRAP-positive cells with more than 3 nuclei was counted (Fig. 4B & 4C). 16 TRAP-positive cells with 3 or more nuclei are counted as osteoclasts after 5 days 17 cultivation. For the TRAP-positive cells, the presence of sodium butyrate (0.1, 0.5, 18 and 1 mM) in the culture medium caused a significant decrease. The presence of 19 AGAF (100 and 150 μg/mL) in the culture medium could also show decreases in the 20 number of TRAP-positive cells by 13.8% and 37.2%, respectively. The osteoclast 21 inhibition was 37.5%, 67.6%, and 86.9% under the treatment of sodium butyrate at 22 concentrations of 0.1, 0.5, and 1 mM, respectively. However, the suppression of 23 osteoclast differentiation of AGAF was not as remarkable as that of sodium butyrate. 24 25 4. Discussion 1 In this study, we showed that AGAF could prevent osteoporosis through its prebiotic 2 effects in OVX mice. Our results showed that AGAF could enhance the number of 3 probiotics and increase cecal SCFA and bone mass density in OVX mice. We 4 observed that the anti-osteoporosis effects of AGAF could be inhibited by SM, a 5 broad-spectrum antibiotic. The results suggested that the prevention effects of AGAF 6 on osteoporosis might cause by its prebiotic effects. Numerous prebiotic isolated from 7 botanic and found as polysaccharides, like inulin, larch wood arabinogalactan, 8 kiwifruit pectin, konjac glucomannan and resistant dextrin (Roberfroid, 2005; Degnan 9 & Macfarlane, 1995; Parkar, et al., 2010; Connolly, et al., 2010; Barczynska, et al., 10 2012). Those prebiotic carbohydrates are regarded to be hydrolyzed and utilized by 11 probiotics only (Tomasik & Tomasik, 2003). AGAF is a type II arabinogalactan and 12 has been reported as a potent prebiotic polysaccharide in our previous study (Yang, et 13 al., 2012). The previous study reported that AGAF promote the number of 14 bifidobacteria of feces especially and the prebiotic mechanism of AGAF may due to 15 up-regulate the expression of ATP binding cassette transporter, a part of nutrient 16 uptake system. 17 OVX mice mimicked middle-aged postmenopausal women. In this study, no 18 differences were observed in the fecal number of bifidobacteria between OVX-H2O 19 mice and the sham group (Chen, et al.,2009). The results of fecal bifidobacteria were 20 similar to those of our previous study (Chen, et al.,2009). However, AGAF could 21 increase the number of fecal bifidobacteria in OVX mice. A prebiotic is a selectively 22 fermented ingredient that allows specific changes, both in composition and/or activity 23 in gastrointestinal micoflora. Thus, AGAF possesses prebiotic characteristics, as 24 previous reported (Yang, et al. 2012). 25 SCFA are the products of prebiotic fermentation, and have been shown to enhance 1 bone health (Scholz-Ahrens, et al. 2007). Butyric acid, an SCFA and a histone 2 deacetylase inhibitor, can influence osteoblasts and osteoclasts and provide protection 3 from bone density loss (Rahman, et al., 2003; Iwami & Moriyama, 1993). In addition, 4 high concentrations of SCFA in the cecum lead to increases in the concentration of 5 soluble Ca (Lopez, et al., 2000). In our study, AGAF treatment increased the cecal 6 SCFA, especially butyric acid, and increased the cecal soluble-Ca concentration. 7 Cholecalciferol-induced CaBP is a key factor in the intestinal transcellular Ca 8 transport system (Bouillon, et al., 2003). A direct correlation exists between the 9 mucosal amounts of CaBP and the efficiency of Ca absorption (Bronner, 2003). 10 Hence, an increase in mucosal CaBP indicates an increase in Ca absorption in this 11 intestinal segment. A previous study reported that the high level of soluble Ca in the 12 cecum induces the expression of CaBP (Yang, et al., in press). In our study, the 13 soluble Ca level was higher in the cecum after AGAF treatment. Moreover, the 14 expression cecal CaBP was enhanced by AGAF administration in OVX mice. These 15 results showed that AGAF could promote intestinal Ca absorption in OVX mice 16 through prebiotic fermentation. 17 Other studies have also shown that increasing Ca absorption affects bone 18 characteristics, such as bone Ca content and bone strength, in OVX rats (Mitamura, et 19 al. 2004). In our study, an enhancement of Ca absorption caused by administration of 20 AGAF may also cause an increase in the Ca content in the lumbar vertebrae of OVX 21 mice. 22 In microCT analysis, trabecular bone volume, trabecular number, trabecular 23 thickness, and trabecular separation of the distal femur were analyzed. AGAF could 24 cause increases in femur trabecular bone volume and trabecular thickness compared to 25 OVX-H2O mice. Trabecular bone volume and trabecular thickness are important 1 factors in bone strength (Yao, et al., 2005). These results implied that AGAF could 2 decrease bone loss and bone structural fractures induced by OVX operation. 3 In plasma bone markers, CTx is part of the composition of bone. Plasma CTx 4 levels are markedly increased in postmenopausal women with osteoporosis, and their 5 values decrease markedly and rapidly with anti-resorption therapy (Qvist, et al., 2002). 6 Although the concentration of OCN is a sensitive marker of bone formation, the 7 plasma concentration of OCN is a feedback control mechanism during active bone 8 resorption (Swaminathan, 2001). Because a high turnover may lead to bone loss, a 9 downregulation of bone turnover may be beneficial to bone metabolism. Treatment by 10 AGAF and inulin could reduce the plasma levels of both CTx and OCN, which were 11 induced by OVX operations. 12 In RT-PCR analysis, the expression of osteoclast-associated genes, TRAP, and 13 cathepsin K was induced by OVX. TRAP is a di-iron-containing metalloenzyme that 14 is expressed in osteoclasts and in subsets of tissue macrophages and dendritic cells 15 (Walsh, et al., 2003). TRAP expression is dramatically upregulated during osteoclast 16 differentiation. Therefore, TRAP activity is commonly used as an identifying marker 17 in osteoclasts (Walsh, et al., 2003). Cathepsin K, a lysosomal cysteine proteinase, is 18 expressed predominantly in osteoclasts. Cathepsin K cleaves key bone matrix proteins, 19 and is believed to have an important role in degrading the organic phase of bone 20 during bone resorption (Saftig, et al. 2000). In this experiment, the expression of 21 TRAP and cathepsin K was increased in OVX mice. The administration of AGAF in 22 OVX mice could suppress the induction of expression of TRAP and cathepsin K. The 23 results showed that AGAF could down-regulate osteoclast differentiation and bone 24 resorption in OVX mice. 25 Runx2 is an essential factor in osteoblast differentiation. Runx2 triggers the 1 expression of major bone matrix genes during the early stages of osteoblast 2 differentiation, but Runx2 is not essential for the maintenance of these gene 3 expressions in mature osteoblasts (Komori, 2010). Moreover, Runx2 inhibits 4 osteoblast maturation and mature bone formation at the late stage of osteoblast 5 differentiation (Komori, 2010). 6 In this study, no rebound increase of Runx2 was shown in the tibia of the OVX 7 mice compared to the sham mice. The results suggested that the OVX mice might 8 have been in the mid-to-late stage of the bone resorption process. A previous study 9 indicated that a supplement of dried plum could prevent OVX-induced bone loss 10 (Rendina, et al.,2012). In addition, the study also reported that the expression of 11 Runx2 decreased significantly in the presence of dried plums in OVX mice. The 12 results of our study showed that the expression of Runx2 was similar to those of 13 Rendina et al. (2012). This implies that AGAF might promote the transition of 14 osteoblasts into osteocytes in late stages of OVX-induced osteoporosis. 15 OCN is a major noncollagenous protein component of the bone extracellular 16 matrix, and is synthesized and secreted exclusively by osteoblasts in the late stage of 17 maturation; it is considered an indicator of osteoblast differentiation (Sila-Asna, et al., 18 2007). OCN is also a sensitive bone turnover marker. The expression of OCN showed 19 a rebounded increase in OVX mice caused by the over expression of osteoclasts in 20 this study. Treatment of AGAF significantly inhibited the increased expression of 21 OCN, which indicated that AGAF could suppress the bone turnover marker through 22 the inhibition of osteoclasts. The results of OCN expression were identical to those of 23 plasma OCN concentrations. These results show that bone protection by AGAF might 24 prevent bone resorption by osteoclasts in OVX mice. 25 We evaluated the effects of AGAF in the treatment of postmenopausal 1 osteoporosis using OVX mice. To test the hypothesis that the anti-osteoporosis effects 2 of AGAF were caused by its prebiotics, we supplemented drinking water with SM to 3 investigate the effects on OVX mice. SM in drinking water could significantly 4 eliminate not only the prebiotic effects of AGAF but also the anti-osteoporosis effects 5 in plasma bone markers in OVX mice. The preventative bone loss of AGAF was 6 inhibited by SM. The results showed that the anti-osteoporosis properties of AGAF 7 were derived mainly from its prebiotic effects. Certain studies have reported that 8 inulin, a well-known prebiotic fructan, could promote intestinal mineral absorption 9 and bone health (Scholz-Ahrens, et al. 2007; Kruger, et al. 2003). 10 An in vivo study showed that AGAF is an anti-osteoporosis component through its 11 prebiotic fermentation products. The results of the in vitro study showed that AGAF 12 could not influence the activity of ALP on osteoblast cell line MC3T3-E1, but butyric 13 acid could increase the activity of ALP significantly. Similar results were observed in 14 murine osteoclast differentiation. These results suggested that the mechanism of 15 anti-osteoporosis effects was caused by its prebiotic fermentation. 16 We investigated why AGAF or its fermentation products, such as SCFA, act as 17 anti-osteoporosis materials. The concentration of butyric acid was considerably 18 affected by AGAF administration. Sodium butyrate was used to examine the 19 anti-osteoporosis effects of SCFA. In an osteoblast differentiation study, AGAF did 20 not affect ALP production. ALP is crucial to the mineralization of osteoblasts (Zhao, 21 et al., 2007). Sodium butyrate, but not AGAF, could improve the mineralization 22 activities of osteoblasts. In osteoclast cell line differentiation, we observed that AGAF 23 and sodium butyrate could both influence the formation of osteoclasts. However, 24 AGAF activity in resisting osteoclast formation was considerably weaker than that of 25 sodium butyrate. These in vitro studies showed that sodium butyrate was a major 1 compound in anti-osteoporosis functions. In addition, certain studies have also shown 2 that histone deacetylase inhibitors, such as butyrate, accelerated in vitro osteoblast 3 maturation (Katono, et al., 2008; Schroeder & Westendrof, 2005). Therefore, it is 4 possible that AGAF partially ameliorates osteoporosis in OVX mice by enhancing 5 osteoblast maturation and inhibiting osteoclast differentiation through butyrate 6 production. 7 8 5. Conclusions 9 The results clearly showed that administration of AGAF inhibited bone turnover, 10 elevated intestinal Ca absorption, and prevented Ca loss and deterioration in bone 11 volume in OVX mice. Our study provides evidence that prebiotic activity was 12 involved in the anti-osteoporotic mechanisms of AGAF. In addition, the prebiotic 13 potency and bone protection activities of AGAF were higher than those of inulin, 14 based on the dosage. Daniel et al. demonstrate that the half-life of butyrate in mice 15 and rabbits is less than 5 min (Daniel, et al., 1989). This indicates that the rapid 16 elimination of butyrate is a limiting factor in practical applications (Daniel, et al., 17 1989). Our results showed that the prebiotic fermentation effects of AGAF might 18 prolong the absorption period of butyrate in OVX mice. The results showed that 19 AGAF could be a new source of food supplements in the promotion of bone health for 20 postmenopausal osteoporosis. 21 22 Acknowledgment. 23 This study was supported by grants from the National Science Council of the 24 Republic of China (NSC 101-2320-B-039-019) 25 1 REFERENCES 2 3 4 Asahara, T., Nomoto, K., Shimizu, K., Watanuki, M., & Tanaka, R. (2001). Increased resistance of mice to Salmonella enterica serovar Typhimurium infection by synbiotic administration of Bifidobacteria and transgalactosylated 5 6 7 8 9 10 oligosaccharides. Journal of Applied Microbiology, 91, 985-996. Barczynska, R., Slizewska, K., Jochym, K., Kapusniak, J., & Libudzisz, Z. (2012). The tartaric acid-modified enzyme-resistant dextrin from potato starch as potential prebiotic. Journal of Functional Foods, 4, 954-962. Bouillon, R., Van Cromphaut, S., & Carmeliet, G. (2003). Intestinal calcium absorption: Molecular vitamin D mediated mechanisms. Journal Cellular 11 12 13 Biochemistry, 88, 332-329. Bradford, M. M. (1976). A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. 14 15 Analytical Biochemistry, 72, 248-254. Bronner, F. (2003). Mechanisms of intestinal calcium absorption. Journal Cellular l 16 17 18 19 Biochemistry, 88, 387-393. Chen, H. L., Hong, L. T., Lee, J. K., & Huang, C. J. (2009). The bone-protective effect of a Taiwanese yam (Dioscorea alata L. cv. Tainung No.2) in ovariectomised female BALB/C mice. Journal of the Science of Food and 20 21 22 Agriculture , 89, 517-522. Chen, Y. M., Ho, S. C., & Woo, J. L. (2006). Greater fruit and vegetable intake is associated with increased bone mass among postmenopausal Chinese women. 23 24 25 26 British Journal of Nutrition, 96, 745-751. Chang, D. C. N., Chou, L. C., & Lee, G. C. (2007). New cultivation methods for Anoectochilus formosanus Hayata. Orchid Science and Biotechnology, 2, 56-60. Chomczynski, P., & Sacchi, N. (1987). Single-step method of RNA isolation by acid 27 28 29 30 guanidinium thiocyanate-phenol-chloroform extraction. Analytical Biochemistry, 162, 156-159. Connolly, M. L., Lovegrove, J. A., & Tuohy, K. M. (2010). Konjac glucomannan hydrolysate beneficially modulates bacterial composition and activity within the 31 32 faecal microbiota. Journal of Functional Foods, 2, 219-224. Coxam, V. (2007). Current data with inulin-type fructans and calcium, targeting bone 33 34 35 health in adults. The Journal of Nutrition, 137, (Suppl. 11), S2527-S2533. Daniel, P., Brazier, M., Cerutti, I., Pieri, F., Tardivel, I., Desmet, G., Baillet, J., & Chany, C. (1989). Pharmacokinetic study of butyric acid administered in vivo as 36 37 sodium and arginine butyrate salts. Clinica Chimica Acta, 181, 255-263. Datta, N. S. (2011). Osteoporotic fracture and parathyroid hormone. World Journal of 38 Orthopedics, 2, 67-74. 1 de Villiers, T. J., & Stevenson, J. C. (2012). The WHI: the effect of hormone 2 3 4 5 6 7 replacement therapy on fracture prevention. Climacteric, 15, 263-266. Degnan, B. A., & Macfarlane, G. T. (1995). Arabinogalactan utilization in continuous cultures of Bifidobacterium longum: effect of co-culture with Bacteroides thetaiotaomicron. Anaerobe, 1, 103-112. Devareddy, L., Hooshmand, S., Collins, J. K., Lucas, E. A., Chai, S. C., & Arjmandi, B. H. (2008). Blueberry prevents bone loss in ovariectomized rat model of 8 9 10 11 postmenopausal osteoporosis. The Journal of Nutritional Biochemistry, 19, 694-699. Du, X. M., Irino, N., Furusho, N., Hayashi, J., & Shoyama, Y. (2008). Pharmacologically active compounds in the Anoectochilus and Goodyera species. 12 13 14 Journal of Natural Medicines, 62, 132-148. Honda, A., Umemura, Y., & Nagasawa, S. (2001). Effect of high-impact and low-repetition training on bones in ovariectomized rats. Journal of Bone and 15 16 17 18 Mineral Research, 16, 1688-1693. Idris, A. I. (2012). Ovariectomy/orchidectomy in rodents. Methods in Moleculae Biology, 816, 545-551. Isama, K., & Tsuchiya, T. (2003). Enhancing effect of poly(L-lactide) on the 19 20 21 differentiation of mouse osteoblast-like MC3T3-E1 cells. Biomaterials, 24, 3303-3309. Iwami, K., & Moriyama, T. (1993). Effects of short chain fatty acid, sodium butyrate, 22 on osteoblastic cells and osteoclastic cells. The International Journal of 23 24 25 Biochemistry, 25, 1631-1635. Katono, T., Kawato, T., Tanabe, N., Suzuki, N., Iida, T., Morozumi, A., Ochiai, K., & Maeno, M. (2008). Sodium butyrate stimulates mineralized nodule formation and 26 27 28 29 30 osteoprotegerin expression by human osteoblasts. Archives of Oral Biology, 53, 903-909. Khosla, S., Bilezikian, J. P., Dempster, D. W., Lewiecki, E. M., Miller, P. D., Neer, R. M., Recker, R. R., Shane, E., Shoback, D., & Potts, J. T. (2012). Benefits and Risks of Bisphosphonate Therapy for Osteoporosis. The Journal of Clinical 31 32 Endocrinology and Metabolism, 97, 2272-2282. Komori, T. (2010). Regulation of osteoblast differentiation by Runx2. Advances in 33 34 35 Experimental Medicine and Bology, 658, 43-49. Kruger, M. C., Brown, K. E., Collett, G., Layton, L., & Schollum, L. M. (2003). The effect of fructooligosaccharides with various degrees of polymerization on 36 37 38 calcium bioavailability in the growing rat. Experimental Biology and Medicine, 228, 683-688. Lopez, H. W., Coudray, C., Levrat-Verny, M. A., Feillet-Coudray, C., Demigne, C., & 1 Remesy, C. (2000). Fructooligosaccharides enhance mineral apparent absorption 2 and counteract the deleterious effects of phytic acid on mineral homeostasis in rats. 3 4 5 6 Journal of Nutritional Biochemistry, 11, 500-508. Masuda, K., Ikeuchi, M., Koyama, T., Yamaguchi, K., Woo, J. T., Nishimura, T., & Yazawa, K. (2008). Suppressive effects of Anoectochilus formosanus extract on osteoclast formation in vitro and bone resorption in vivo. Journal of Bone and 7 8 9 Mineral Metabolism, 26, 123-129. Mitamura, R., Hara, H., & Aoyama, Y. (2004). Ingestion of raffinose promotes calcium absorption in the large intestine of rats. Bioscience, Biotechnology, and 10 11 Biochemistry, 68, 384-389. Munoa, F. J., & Pares, R. (1988). Selective medium for isolation and enumeration of 12 13 14 Bifidobacterium spp. Applied and Environmental Microbiology, 54, 1715-1718. Niven, S. J., Beal, J. D., & Brooks, P. H. (2004). The simultaneous determination of short chain fatty acid, monosaccharides and ethanol in fermented liquid pig diets. 15 16 17 18 Animal Feed Science and Technology, 117, 339-345. Parkar, S. G., Redgate, E. L., Wibison, R., Luo, X., Koh, E. T. H., & Schröder, R. (2010). Gut health benefits of kiwifruit pectins: Comparison with commercial functional polysaccharides. Journal of Functional Foods, 2, 210-218. 19 20 Pietschmann, P., Rauner, M., Sipos, W., & Kerschan-Schindl, K. (2009). Osteoporosis: an age-related and gender-specific disease-a mini-review. Gerontology, 55, 3-12. 21 22 Rahman, M. M., Kukita, A., Kukita, T., Shobuike, T., Nakamura, T., & Kohashi, O. (2003). Two histone deacetylase inhibitors, trichostatin A and sodium butyrate, 23 24 25 26 27 suppress differentiation into osteoclasts but not into macrophages. Blood, 101, 3451-3459. Parfitt, A. M., Drezner, M. K., Glorieux, F. H., Kanis, J. A., Malluche, H., Meunier, P. J., Ott, S. M., & Recker, R. R. (1987). Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry 28 29 30 Nomenclature Committee. Journal of Bone and Mineral Research, 2, 595-610. Rendina, E., Lim, Y. F., Marlow, D., Wang, Y., Clarke, S. L., Kuvibidila, S., Lucas, E. A., & Smith, B. J. (2012) Dietary supplementation with dried plum prevents 31 ovariectomy-induced bone loss while modulating the immune response in 32 33 34 35 36 37 C57BL/6J mice. Journal of Nutritional Biochemistry, 23, 60-68. Roberfroid, M. B. (2005). Introducing inulin-type fructans. British Journal of Nutrition, 93 (Suppl. 1), S13-25. Qvist, P., Christgau, S., Pedersen, B. J., Schlemmer, A., & Christiansen, C. (2002). Circadian variation in the serum concentration of C-terminal telopeptide of type I collagen (Serum CTx): Effects of gender, age, menopausal status, posture, 38 daylight, serum cortisol, and fasting. Bone, 31, 57-61. 1 Saftig, P., Hunziker, E., Everts, V., Jones, S., Boyde, A., Wehmeyer, O., Suter, A., & 2 von Figura, K. (2000). Functions of cathepsin K in bone resorption. Lessons from 3 4 5 6 7 cathepsin K deficient mice. Advances in Experimental Medicine and Bology, 477, 293-303. Sila-Asna, M., Bunyaratvej, A., Maeda, S., Kitaguchi, H., & Bunyaratavej, N. (2007). Osteoblast differentiation and bone formation gene expression in strontium-inducing bone marrow mesenchymal stem cell. The Kobe Journal of 8 9 10 Medical Sciences, 53, 25-35. Scholz-Ahrens, K. E., Ade, P., Marten, B., Weber, P., Timm, W., Acil, Y., Gluer, C. C., & Schrezenmeir, J. (2007). Prebiotics, probiotics, and synbiotics affect mineral 11 12 13 absorption, bone mineral content, and bone structure. Journal Of Nutrition, 137 ( Suppl 2), S838-846. Schroeder T. M., & Westendorf, J. J. (2005). Histone deacetylase inhibitors promote 14 15 16 osteoblast maturation. Journal of Bone and Mineral Research, 2254-2263. Shih, C. C., Wu, Y. W., & Lin, W. C. (2001). Ameliorative effects of Anoectochilus formosanus extract on osteopenia in ovariectomized rats. Journal of 17 18 Ethnopharmacology, 77, 233-238. Stransky, M., & Rysava, L. (2009). Nutrition as Prevention and Treatment of 19 20 Osteoporosis. Physiological research, 58 (Suppl.1), S7-S11. Swaminathan, R. (2001). Biochemical markers of bone turnover. Clinica Chimica 21 22 23 24 25 Acta, 313, 95-105. Tomasik, P. J., & Tomasik, P. (2003). Probiotics and prebiotics. Cereal Chemistry, 80, 113-117. Walsh, N. C., Cahill, M., Carninci, P., Kawai, J., Okazaki, Y., Hayashizaki, Y., Hume, D. A., & Cassady, A. I. (2003). Multiple tissue-specific promoters control 26 27 28 expression of the murine tartrate-resistant acid phosphatase gene. Gene, 307, 111-123. Weaver, C. M. (2005). Inulin, oligofructose and bone health: experimental approaches 29 30 and mechanisms. British Journal of Nutrition, 93 (Suppl. 1), S99-103. Yang, L. C., Lin, W. C., & Lu, T. J. (2012). Characterization and Prebiotic Activity of 31 Aqueous Extract and Indigestible Polysaccharide from Anoectochilus formosanus. 32 33 34 35 36 37 38 Journal of Agricultural and Food Chemistry, 60, 8590-8599. Yang, L. C., Wu, J. B., Lu, T. J., & Lin, W. C. (in press). The prebiotic effect of Anoectochilus formosanus and its consequences on bone health. British Journal Nutrition. Yao, W., Hadi, T., Jiang, Y., Lotz, J., Wronski, T. J., & Lane, N.E. (2005). Basic fibroblast growth factor improves trabecular bone connectivity and bone strength in the lumbar vertebral body of osteopenic rats. Osteoporosis international,16, 1 2 3 4 5 6 7 1939- 19474. Zhao, Y., Zou, B., Shi, Z., Wu, Q., & Chen, G. Q. (2007). The effect of 3-hydroxybutyrate on the in vitro differentiation of murine osteoblast MC3T3-E1 and in vivo bone formation in ovariectomized rats. Biomaterials, 28, 3063-3073. Figure legends 8 9 Fig. 1. MicroCT analyses of metaphysic of the distal femur in mice of different groups. 10 (A) The photos of microCT scans (i) Sham + H2O group. (ii) OVX + H2O group. 11 These mice showed a decrease in the trabecular bone volume. (iii) OVX + AGAF (5 12 mg/kg) group. (iv) OVX + AGAF (15 mg/kg) group. (v) OVX + inulin (400 mg/kg) 13 group. AGAF and inulin significantly prevented bone loss from OVX-induced 14 osteopenia. (B) Trabecular bone volume (BV/TV, %) and trabecular number (1/mm) 15 (C) Trabecular thickness (μm) and trabecular separation (μm). All values were means 16 ± SD (n = 8). Values with different letters were significantly different. 17 18 Fig. 2. Effects of AGAF and inulin on cecal mucosa CaBP mRNA expression and 19 tibia mRNA expression of TRAP, cathepsin K, OCN and Runx2 in OVX mice. A, 20 Fragments were amplified by RT-PCR. The fragments reflect the pooled data for eight 21 samples. B, The expression levels of CaBP, TRAP, cathepsin K, OCN and Runx2 22 mRNA were measured and quantified densitometrically. Values were normalized to 23 GAPDH mRNA expression. All values were means ± SD (n = 8). Values with 24 different letters were significantly different. 25 26 Fig. 3. Effects of AGAF and inulin on plasma bone marker in OVX mice. (A) The 27 plasma OCN and CTx in OVX mice were oral administration of AGAF (5, 15 mg/kg) 1 or inulin (400 mg/kg) for 3 weeks. (B) the plasma OCN and CTx in OVX mice were 2 administration of AGAF (15 mg/kg) and supplemented with or without SM in 3 drinking water for 3 weeks. All values were means ± SD (n = 8). Values with different 4 letters were significantly different. 5 6 Fig. 4. Effects of sodium butyrate and AGAF on ALP activity of murine osteoblast 7 MC3T3 E1 cell line and on the osteoclast differentiation from RAW264.7 cell line. (A) 8 ALP activity of murine osteoblast MC3T3 E1 cell under the treatment with sodium 9 butyrate or AGAF for 6 days. Cells were lysed by ultrasonic and analyzed for ALP by 10 p-nitrophenyl phosphate. (B) The number of counted osteoclasts per well (C) 11 Osteoclasts were stained by TRAP. All values were means ± SD (n = 3). Values with 12 different letters were significantly different. 13 14 Table 1. Effects of AGAF and inulin on fecal bifidobacteria, cecal free Ca, cecal butyric acid, lactic acid, acetic acid, propionic acid and total SCFA levels in OVX mice Dosage Fecal Bifidobacteria Cecal Lactic (mg/kg ) Log10CFU/g feces Cecal acetic Cecal Propionic Cecal butyric Cecal total acid (μmol/g) acid (μmol/g) acid (μmol/g) acid (μmol/g) SCFA (μmol/g) Cecal free Ca (mg/dL) Sham + H2O - 6.6 0.2b 16.8 0.3a 41.7 1.8a 4.3 0.3a 20.9 0.9b 83.7 2.6ab 18.1 4.0a OVX + H2O - 6.1 0.5a 16.7 0.3a 40.3 2.2a 4.1 0.4a 18.4 0.5a 79.5 1.5a 17.0 2.0a OVX + AGAF 5 7.0 0.2c 18.6 2.7a 46.6 3.2ab 5.8 0.6b 25.2 0.4c 96.2 5.4cd 23.0 5.7b OVX + AGAF 15 7.3 0.2c 17.6 2.4a 50.9 0.9b 6.9 0.1b 29.0 0.3d 104.4 0.8d 24.2 3.0b 7.4 0.3bc 19.2 2.1a 42.4 1.4a 6.4 0.3b 21.4 1.1b 89.7 0.9bc 23.8 2.7b OVX + Inulin 400 All values were means ± SD (n = 8). Values with different letters were significantly different. Table 2. MicroCT analyses of femur on OVX mice administrated AGAF and with or without SM supplement in drinking water Treatments Trabecular bone volume (%) Trabecular number ( 1/mm) Trabecular thickness (μm) Trabecular separation (μm) Sham + H2O + H2O 31.3 2.3b 3.7 0.2c 87.5 8.9c 186 24.0c OVX + H2O + H2O 27.5 1.0a 3.3 0.1ab 62.7 6.8a 199 16.9c OVX + AGAF + H2O 29.8 1.7b 3.5 0.2bc 75.0 7.9bc 194 12.8c OVX + H2O + SM 26.9 2.4a 3.2 0.3a 62.5 5.9a 202 15.4c OVX + AGAF + SM 27.6 2.1a 3.3 0.3ab 63.2 6.1a 200 14.3c SM (2 mg/mL) was supplement in drinking water. The mice were administrated H2O or AGAF (15 mg /kg) for 3 weeks. All values were means ± SD (n = 8). Values with different letters were significantly different.