Dose - Andrew N. Schmelz, PharmD
advertisement

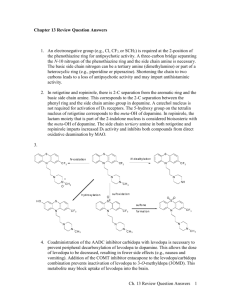
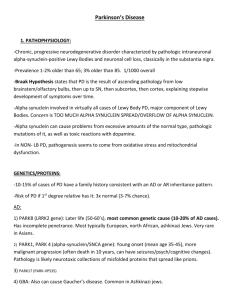
Parkinson’s Disease Dr. Andrew Schmelz, PharmD anschmel@purdue.edu Post-Doctoral Teaching Fellow Dept of Pharmacy Practice Purdue University March 4, 2009 Objectives Describe physiologic changes in patients with Parkinson’s Disease List symptoms with which Parkinson’s patients typically present List and define extrapyramidal symptoms For each drug class, state one example drug, mechanism of action, common dose, and associated side effects Background Parkinson’s disease: a degenerative disease of the brain that impairs motor skills, speech, and other functions Especially prevalent in elderly white males Characterized by specific changes in motor function Pathophysiology Substantia nigra – Region in brain that plays a role in movement – Parkinson’s is characterized by loss of neuronal cells in this region Pathophysiology (cont.) Neurons depleted in the substantia nigra result in imbalance of dopamine and acetylcholine – Reduced dopamine activity – Normal acetylcholine activity Dopamine Acetylcholine Acetylcholine Dopamine Symptoms Tremor (and pill rolling) Bradykinesia Rigid muscles (cogwheel rigidity) Impaired posture/balance Loss of autonomic movement Speech changes Dementia YouTube Video http://www.youtube.com/watch?v=S5EE8 EVv600&feature=related Extrapyramidal (EPS) Symptoms EPS symptoms usually occur secondary to medication Dyskinesias (Movement disorders) – Irregular body movements – Tongue movements, lip smacking – Finger movements, arm/leg movements Akathisia (Restlessness) – Extreme form of internal/external restlessness – Can be exhausting and debilitating EPS Symptoms (cont.) Dystonia (Muscle tension disorders) – Very strong, painful muscle contractions – Unusual twisting of parts of the body “Tardive” Disorders – Indicates long-term observation of EPS symptoms – Can be of any classification listed above – Often indicate permanence YouTube Videos Dyskinesias – http://www.youtube.com/watch?v=FUr8ltXh1 Pc&feature=related Akithisias – http://www.youtube.com/watch?v=pSXzuCNlI 6Q Dystonias – http://www.youtube.com/watch?v=nG1XrmEa sVk&feature=related Pharmacotherapy Approaches of therapy – Slow loss of dopamine in brain – Improve symptoms by other means – Prevent/delay non-muscular complications – Prevent/delay institutionalization Choice of medications used early in therapy will have a STRONG impact on long-term course of the disease Levodopa/Carbidopa Example: Sinemet® (levodopa/carbidopa) MOA: – L-Dopa - converted to DA in brain – Carbidopa – inc effectiveness and reduces SEs Dose: 25mg/100mg carbi/levo TID SE: EPS symptoms, orthostatic hypotension, “wearing off”, N/V Most effective, used as late as possible “Wearing-Off” Phenomenon Loss of effectiveness of levodopa before next dose – Increased with duration of therapy – Indicates need for dosage increase – Limits duration of therapy Dopamine Agonists Example: Mirapex® (pramipexole) MOA: Dopamine receptor agonist Dose: 0.125mg – 1.5mg TID SEs: orthostatic hypotension, impulsive behavior, hallucinations, EPS (especially when taken with levodopa) Often used as initial treatment Can be used concurrently with levodopa COMT Inhibitors Example: Comtan® (entacapone) MOA: inhibit COMT, responsible for breakdown of L-Dopa in periphery Dose: 200mg with each levodopa/carbidopa dose SEs: increase in EPS symptoms, N/V, dry mouth Used in combination with levodopa/carbidopa MAO-B Inhibitors Example: Deprenyl® (selegiline) MOA: inhibit MAO-B, responsible for breakdown of DA in brain Dose: 5mg BID SEs: dizziness, N/V, EPS symptoms Use with low-tyramine diet may be required Potential for drug interactions Anti-cholinergic Drugs Example: Cogentin® (benztropine) MOA: inhibit ACh; restore balance to DAACh relationship Dose: 0.5-6mg daily SEs: anti-ACh effects (see prev lecture!) Can impair cognitive function which limits use Amantadine Example: Symmetrel® (amantadine) MOA: enhance dopamine release, antiACh properties, NMDA antagonist Dose: 100-400mg/day (daily to BID) SEs: dizziness, anxiety, N/V/D, anti-ACh effects Most commonly used later in therapy as adjunct PT Considerations Coordinate therapy session with peak effects of drugs – After breakfast dose of levodopa Need to monitor BP while receiving antiparkinsons meds – Concern for orthostatic hypotension PT can reduce need for Parkinson’s drugs Features of PT Program Regular exercise – Walking (1+ miles/day), swimming, golf, etc Stretching and strengthening Exaggerated or patterned movements Mobility aids, orthotics Training in transfer techniques Training in techniques to improve posture and walking Questions? Alzheimer’s Disease Objectives Describe physiologic changes in patients with Alzheimer’s Disease For each drug class, state one example drug, mechanism of action, common dose, and associated side effects Background Alzheimer’s Disease is an age-related, non-reversible brain disorder – Characterized by memory loss and confusion – Gradually leads to personality and behavioral changes Most common cause of dementia in patients age 65 and older Pathophysiology Etiology of Alzheimer’s disease is unknown Disease is characterized by: – Amyloid plaques – Neurofibrillary tangles – Loss of connection of neurons responsible for memory and learning Pharmacotherapy Currently, no FDA-approved treatment for slowing progression of disease Pharmacotherapy aimed at treating symptoms and improving cognitive function Cholinesterase Inhibitors Example: Aricept® (donepazil) MOA: Increase ACh, increasing cholinergic function Dose: 5 – 10mg daily at bedtime SEs: SLUD, N/V, bradycardia, hypotension, GI bleeding (rare) Cholinesterase Inhibitors (cont.) Other examples: – Exelon® (rivastigmine) – Reminyl® (galantamine) Appear to help patients for months to a few years Indicated for mild to moderate Alzheimer’s symptoms NMDA Antagonist Example: Namenda® (memantine) MOA: inhibit NMDA receptor, which plays a role in transmission of excitatory neurotransmission Dose: 5mg daily to 10mg BID SEs: Drowsiness/dizziness PT Considerations Cognitive impairment will have negative effect on ability to follow instruction Questions?