2015_KSPAN_Spring_Seminar_Unusual_Suspects 791.4 KB
advertisement
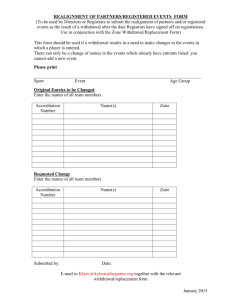
The (UN)usual Suspects: A Line-up of Medications Responsible for Withdrawal Syndrome Kathryn Ruf, PharmD, BCPS Clinical Pharmacist Specialist-Critical Care katieruf@kentuckyonehealth.org March, 2015 The Case of KR KR is a 56 YO female s/p 2 vessel CABG. She has a PMH significant for CAD, hyperlipidemia, GERD, depression/anxiety, back pain, HTN, and COPD http://www.ucg.org/files/images/articleimages/cold-case-file-closed.jpg.crop_display.jpg Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily The Facts…. •POD 0 is uneventful, but team unable to extubate because she did not leave the OR until 7pm. KR remains sedated on propofol. •On POD 1, patient is notably agitated and uncooperative. BP has increased to 170/105 and HR 130s, but is NSR. Due to the agitation, HTN, and h/o severe COPD, KR is not able to be extubated. Propofol continues. No other medications for sedation or any pain medications are administered. •By POD 3, lung function still has not improved and increased secretions are noted. Agitation still remains a problem, but has slightly improved when propofol was changed to midazolam on POD 2. BP/HR is still elevated, but better controlled on IV metoprolol. KR is now febrile and has diarrhea. Cultures are sent. KR appears more confused. The Facts… • By morning of POD 4, KR’s BP is low (MAP 40s-50s), WBC is 25K, and SCr has increased. She remains febrile. Team suspects sepsis/shock and starts antibiotics and ultimately norepinephrine. • BP remains poor and additional vasorpessors (vasopressin, epinephrine, and dobutamine) are started over the next 2 days. • Ultimately, KR expires on POD 6. What really happened to KR? • Could we have suspected that we may face a difficult post-op course for KR? • Is this a drug misadventure? If so, what drugs and how? • Did we contribute to KR’s death? • If so, can we prevent this from happening in the future? From a pharmacist’s perspective: ALWAYS suspect the drugs! www.mycutegraphics.com Your Mission (should you choose to accept it…..) • Describe under-recognized medications that may precipitate withdrawal syndromes. • Discuss the importance of medication reconciliation in the continuum of compassionate care. • Develop a nursing plan of care to recognize and manage these medication withdrawal syndromes. What is withdrawal? • A group of symptoms of variable clustering and degree of severity which occur on cessation or reduction of use of a psychoactive substance that has been taken repeatedly, usually for a prolonged period and/or in high doses…Typically the features of a withdrawal syndrome are opposite of those of acute intoxication. http://www.who.int/substance_abuse/terminology/withdrawal/en/index.html Concepts to Consider in Withdrawal Syndromes 1. 2. 3. 4. Mechanism of action of the medication/half life Duration of medication use prior to cessation Degree and mechanism of physiologic adaptation Pharmacodynamics/physiologic effect of the medication and physiologic effect of being without the medication 5. Risk of withdrawal versus benefit of therapy cessation Back to the case…. She is on 2 psychoactive medications…..that we did NOT continue on admission. Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily 1. www.definingcandada.ca The UN(usual) Suspects Steroid Statin Antidepressant PPI 1. 2. www.polyvore.com www.mycutegraphics.com Statin Withdrawal Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily Statin Withdrawal • Mechanism of Action: Inhibits HMG-CoA reductase thereby preventing the biosynthesis of cholesterol • Pleiotropic Effects: • Effects immune cells, like macrophages, dendritic cells, and T cells, and may exhibit an anti-inflammatory effect independent of its cholesterol lowering mechanism1 • Increases nitric oxide production and downregulates Ang II AT(1) receptors, endothelin-1, vascular inflammatory adhesion molecules, and inflammatory cytokines2 (anti-inflammatory, vasodilatory) • Investigated in sepsis/pneumonia: Proposed benefit due to immunomodulation and inhibition of endotoxin-induced cellular changes 3 • 2011 meta-analysis of 11 RCTs found no effect of statins on risk of infections or infection related mortality.4 Authors concluded benefit to be unlikely. 1. 2. 3. 4. Curr Opin Lipidol 2011;22(3):165-170. Pharmacotherapy 2006;26(9):1288-96. UTD 2013;Topic 1631. BMJ 2011;343:d7281. Statin Withdrawal • Statin Cessation: • • Rebound deterioration of vascular function1 Rebound inhibition of vascular protective substances and activation of vascular deleterious substances2 • Supporting Data: • • • Retrospective review of PRISM, National Registry of Myocardial Infarction 4, and GRACE trials revealed worse outcomes if statins were discontinued during a patient’s hospitalization for ACS.2 • If statins are withdrawn during the first 24 hours of hospitalization for NSTEMI mortality/morbidity was 11.9% v. 5.7% (p<0.01)3 Prospective RCT in ischemic stroke found stopping statins for 3 days was associated with a 4.7-fold increase in risk of death or dependency, neurologic deterioration, and larger infarct. 1,4 Discontinuation in the post-op period following a major vascular surgery was associated with increased myocardial ischemia, non-fatal MI, and CV death. 1,5 • Studies are limited, but most suggest that under conditions of acute vascular stress, discontinuation of statins should be contraindicated.1 • Consider use of extended release versions peri-operatively initiated several weeks before surgery to maximize anti-inflammatory and plaquestabilizing benefits. 6,7,8 1. Curr Atheroscler Rep 2011;13(1):23-30. 2. 3. 4. 5. 6. 7. 8. Pharmacotherapy 2006;26(9):1288-96. Arch Intern Med 2004;164(19):2162-8. Neurology 2007;69:904-910. Am J Cardiol 2007;100:316-320. NEJM 2004;350(15):1495-1504. JAMA 2004;292(11):1365-1367. Am Fam Physician. 2012;85(3):239-246. Anti-Hypertensive Withdrawal Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily Anti-Hypertensive Withdrawal • Mechanism of Action: • • Clonidine: α2 agonist: Activates pre-synaptic α2 receptors resulting in reduced sympathetic outflow and decreased HR and BP Metoprolol: β-blocker: Competitively blocks β1 receptors to reduce sympathetic activity resulting in decreased HR and BP • Antihypertensive Cessation: • • Clonidine: Increased sympathetic and parasympathetic discharge; increased catacholamines; “pheochromocytoma-like”1 Beta Blocker: Increased beta receptor sensitivity occurs after persistent beta blockade. Transient sympathetic hyper-response results from this increased receptor sensitivity rather than an increase in circulating catecholamines.2,3 • Withdrawal Syndrome: • • Clonidine: Increased BP, insomnia, tremor, restlessness, headache, stomach pains, nausea1 Beta Blocker: Increased BP and HR, palpitations, tremor, sweating, headache, general malaise2 • Post-operative discontinuation after vascular surgery may increase CV mortality and postoperative MI 4 1. 2. 3. 4. American Heart Journal 1973;85(5):605-610. European Journal of Clinical Pharmacology 1979;15(3):215-217. Clin PharmacolTher 1982;31(1):8-15. Am Heart J 2001; 141(1): 148-53. Antidepressant Discontinuation Syndrome Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily Antidepressant Discontinuation Syndrome • Mechanism of Action: Increases serotonin levels at the synapse through blockade of serotonin reuptake pump 1,2 • Physiologic Adaptation: Post-synaptic serotonin receptors down-regulate in response to the increased serotonin at the synapse 1,2 • SSRI Cessation: Mechanism is largely unknown 1 • May be associated with a decrease in serotonin at the synapse coupled with down-regulated receptors 1,3 • May directly relate with discontinuation syndrome, or cause downstream effects to other neurotransmitters (NE, dopamine, GABA)1,3 1. Am Fam Physicians 2006;74(3):449-56. 2. http://us.gsk.com/products/assets/us_paxilcr.pdf 3. J Serotonin Res 1996;3(2):75-83. Antidepressant Discontinuation Syndrome •Affects 20% of patients1 •Mean onset: 3 days (may be as soon as hours)1,2 and lasts ~ 5 days 1,16 •Degree of withdrawal associated with half life of the SSRI and duration of therapy 1 •Mild to moderate symptoms of withdrawal demonstrated after 12 weeks of treatment 1,3 •Symptoms are more rare after only 6-8 weeks of treatment1,19 •Increased symptoms of discontinuation syndrome when antidepressants with shorter half lives are discontinued1 1. 2. 3. 4. 5. Am Fam Physicians 2006;74(3):449-56. http://pi.lilly.com/us/cymbalta-pi.pdf CNS Drugs 2002;16:273-83. B J Psychiatry 1995;167:374-9. J Clin Psychiatry 1997;58(suppl 7):17-21. Antidepressant Discontinuation Syndrome • FINISH Pneumonic 1,26 • Flu-Like Symptoms • Fatigue/lethargy/malaise/muscle aches/HAs/diarrhea • Insomnia • Nausea • Imbalance • Dizziness/vertigo/gait instability • Sensory Disturbances • Paresthesia • Hyper-arousal • Anxiety/agitation 1. Am Fam Physicians 2006;74(3):449-56. 2. J Clin Psychiatry 1998;59:255. Glucocorticoid Withdrawal Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily Glucocorticoid Withdrawal • Mechanism of Action: Decreases inflammation/ Exhibits immunosuppressive activity 1 1. UTD 2013;Topic 159. 2. CCM 2004;8:243-252. Glucocorticoid Withdrawal • Physiologic Adaptation: Hypothalamic-Pituitary Axis Suppression 2. http://upload.wikimedia.org/wikipedia/en/b/b1/Basic_HPA_Axis.jpeg Glucocorticoid Withdrawal • Physiologic Adaptation: Patients may be at high risk for HPA suppression if: • Take glucocorticoid dose equivalent to 20 mg of prednisone/day for more than 3 weeks • Patients taking 10-20mg of prednisone/day for more than 3 weeks may be at an intermediate risk • Receive an evening/bedtime dose of prednisone for more than a few weeks • Have a cushingoid appearance 1. UTD 2013;Topic:7983. Glucocorticoid Withdrawal • Withdrawal Syndrome: Symptoms are consistent with secondary adrenal insufficiency and include1: • • • • • • • • • • Hypotension Electrolyte disturbances Anorexia/nausea/vomiting/abdominal pain Weakness Fatigue/lethargy Hypoglycemia lethargy Fever Confusion/coma High risk patients for withdrawal should be assumed to be adrenally suppressed and be given glucocorticoids surrounding ‘stressful’ events (ie. surgery, serious infection) 2 Testing may be warranted for intermediate risk2 • Low dose ACT stimulation test 1. UTD 2013; Topic:159. 2. UTD 2013;Topic:7983. Aspirin Withdrawal Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily Aspirin Withdrawal •Mechanism of Action: Irreversible inactivation of COX 1 and 2, thereby decreasing TXA2 and prostaglandin production. This results in anti-platelet and anti-inflammatory effects1 •Aspirin Cessation: Mechanism unclear. •Platelet aggregation “rebound phenonmenon”2 •Rapid increase of TXA2, rapid recovery of COX activity 2,3 •Withdrawal Syndrome: •Meta-analysis revealed a 3-fold increase of adverse cardiac events when aspirin was discontinued in patients receiving secondary prevention.1,4 •If the patient had stents, a 90-fold increase in complications resulted. 1,4 •Risk and benefit of aspirin cessation must be carefully evaluated in the perioperative period. •Increases surgical bleeding by ~22%1,5 •A meta-analysis of studies comparing patients who are taking low-dose aspirin to those that were not found no difference in severity of bleeding (with exception of intracranial and TURP procedures) or mortality between the groups. 1,6 1. Am Fam Physicians 2012;85(3):239-246. 2. 3. 4. 5. 6. J Am Coll Cardiol, 2005;45(3):456-459. Blood Coag Fibrinolysis 1996;7:80-84. Am J Cardiol 2001;88(12):1413-4. Br J Anesthesia. 2007;99(3):316-328. J Intern Med 2005;257(5):399-414 And yes, even proton pump inhibitors can be associated with a withdrawal syndrome! Oxycontin 40mg BID Alprazolam 1mg TID Simvastatin 20mg QHS Clonidine 0.1mg TID Citalopram 20mg daily Prednisone 30mg daily Prilosec 40mg daily Metoprolol 100mg BID Aspirin 81mg daily The Case of KR…Revisited • Could we have suspected that we may face a difficult post-op course for KR? • Is this a drug misadventure? If so, what drugs and how? • Did we contribute to KR’s death? •If so, can we prevent this from happening in the future? Medication Reconciliation • According to the Institute of Medicine1: • At least 1.5 million preventable ADEs (adverse drug events) occur in the US each year • Each preventable ADE: $8,750 • If you assume only 400,000 ADE/yr that would be: • $3.5 BILLION dollars!! • Medication reconciliation reduced the rate of medication errors by 70% and ADEs by over 15% 2,3 1. 2. 3. http://www.iom.edu/~/media/Files/Report%20Files/2006/Preventing-Medication-Errors-Quality-Chasm-Series/medicationerrorsnew.pdf How-to-Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011. Quality Management in Health Care 2004;13(1):53-59. Medication Reconciliation • It is NOT just ‘one more form’ to fill out. • We get caught up on focusing on the form rather than the INTENTION of the process1 • It should be a “critical thinking function” 1 not a mindless activity • It is a process.1 • Verification, clarification, and reconciliation • Performed On admission, transfer, and discharge • It may be the MOST important form you review on admission. 1. How-to-Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011. Medication Reconciliation • It is not always about what medications we do continue, but about what we DON’T continue! • Each medication that is NOT ordered counts as a discrepancy and should be reconciled.1 • Look for any adverse drug events that might be indicated in the chart to see if the ADE was the result of the inadvertent discontinuation of a medication or an order that was missed at a point of transition. • If you find this, it counts as an ERROR and an ADE. 1 Sometimes, you may be the only one aware of the complexities of a patients home medications. 1. How-to-Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011. Medication Reconciliation • Barriers1 – No clear owner of the process • Reconciliation is a TEAM process. All disciplines must be involved in the process. It is NOT just a physician’s job. • Physicians are, however. responsible for the ordering and management of the patient’s medication regimen. • Clear accountability must be assigned. It is vital that all staff understand the goals an dhow the process is designed. – Having complete information – Time 1. How-to-Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011. Medication Reconciliation Tips • Try to get as many details as possible • • • • Duration of use Exactly when they take the medication Last dose Medication Reconciliation form is an order…must have all details • Approach it from a patient perspective1 • Most patient’s would be surprised and disheartened to learn that collecting an accurate medication list and MAKING CLINICAL DECISIONS on the basis of that list are viewed as a burden and not done as a matter of routine 1. How-to-Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011. Closing Argument • Numerous medications are associated with some degree of withdrawal syndrome that may result in adverse drug events. • Medication reconciliation is a PROCESS (not a form) that can be used to reduce medication errors and adverse drug events associated with these syndromes. • The decision to not resume a medication for a hospital inpatient should be based in sound clinical judgment and not an error in omission or failure to fully engage in the process. • Use the medication reconciliation process as a way to advocate for your patient. Remain vigilant. Always look for the UN(usual) Suspects. Steroid Statin Antidepressant PPI 1. 2. www.polyvore.com www.mycutegraphics.com (REALLY) 1. www.definingcandada.ca The (UN)usual Suspects: A Line-up of Medications Responsible for Withdrawal Syndrome Kathryn Ruf, PharmD, BCPS Clinical Pharmacist Specialist-Critical Care katieruf@kentuckyonehealth.org March, 2015