anti-PD-1 - Grupo Gallego de Cáncer de Pulmón
advertisement

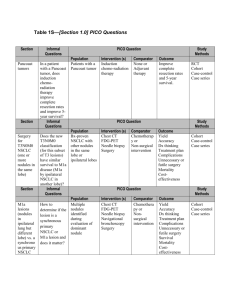
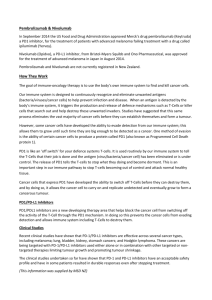
IV REUNIÓN GIDO-GGCP Inmunoterapia en Cáncer de Pulmón Dr. José Muñoz Langa Servicio Oncología Médica Hospital Universitario y Politécnico La Fe Baiona, 25 Abril 2015) Despite advances, only small incremental OS benefits in overall patient population Docetaxel 2002 1st-line combination with chemotherapy Maintenance treatment after 1st-line chemotherapy Bevacizumab‡ 2006 Paclitaxel 1998 Pemetrexed‡ 2008 Gemcitabine 1996 Pemetrexed‡ 2009 Vinorelbine 1994 Cisplatin* 1978 Pemetrexed‡ 2004 Erlotinib 2004 Docetaxel 1999 After failure of 1 prior chemotherapy 1st-line or unspecified setting single agent Gefitinib† 2003 Erlotinib 2010 Carboplatin* 1989 Crizotinib§ 13+ 2011 (US)/2012 (EU) Nab-Paclitaxel 2012 12+ ~8–10 ~6 ~2–4 1970 Erlotinib** 2013 Median OS, months 1980 1990 2000 2010 Afatinib**,# 2013 *Not approved in NSCLC, but commonly used; †Restricted to patients participating in a clinical trial or continuing to benefit from treatment already initiated; ‡Non-squamous #Afatinib NSCLC only; §ALK-positive NSCLC only; **EGFR exon 19 deletions or exon 21 (L858R) substitution mutations only; is approved for the treatment of patients with activating EGFR mutations but only PFS data have been published (May 2014). U.S. Food and Drug Administration. Available at www.fda.gov. Accessed September 2014; European Medicines Agency. Available at http://www.ema.europa.eu. Accessed September 2014; NCCN Guidelines. Non-small cell lung cancer. v3.2014. Immuno-Oncology (I-O): can it address unmet needs in lung cancer? “Immunotherapy represents a new hope for NSCLC patients”, Cancer patient “In any trial you get the odd patient who does very well, but this is an order of magnitude above that.”, Mick Peake, Glenfield Hospital “The PD-1 antibodies stop lung cancer cells from blocking the body's natural immune response to cancer. A drug that can inhibit PD-1 may be able to treat a variety of cancers, which is very exciting”, Myron Bednar, Hunterdon Regional Cancer Center “The high level of excitement around this space is that immune checkpoint inhibitors may apply to a very broad range of cancer types, as both monotherapies and combination therapies. The data we are seeing so far, including recently released at ASCO, also indicates the mechanism works in patients who have failed previous cancer therapies.”, Stephen Dunn, LifeTech Capital “We look forward to the potential for the combination of checkpoint inhibitors, like nivolumab, with small molecule inhibitors in patients with EGFR mutated lung cancer”, Naiyer Rizvi, Memorial Sloan Kettering Cancer Center “The field of immunotherapy has exploded in the last decade, and more and more patients are benefiting”, Steven O'Day, USC Objetivos de la Charla: Revisar los fundamentos científicos de la inmuno-oncología en el cáncer de pulmón y en qué se diferencia de otras modalidades de tratamiento. Discutir los últimos avances en inmunoterapia para el tratamiento del cáncer de pulmón. Analizar el problema de la identificación de biomarcadores para las terapias inumono-oncológicas y su potencial valor predictivo. Valorar el potencial de la inmunoterapia sola o en combinación con otras modalidades de tratamiento en la práctica clínica. Inmuno-edición del Cáncer: Las Tres “E”. Dunn GP et al. Immunity. 2008; 21:137-148. The Cancer-Immunity Cycle Chen DS and Mellman I. Immunity. 2013;39. Stimulatory and Inhibitory Factors in the Cancer-Immunity Cycle Chen DS and Mellman I. Immunity. 2013;39. Mecanismos Tumorales para Escapar del Sistema Inmune Goldman et al, Nature Biotechnology, 2009 Mecanismos Tumorales para Escapar del Sistema Inmune Mecanismos Tumorales para Escapar del Sistema Inmune Duray et al, J of Immunol Research, 2010 Inmunidad Adaptativa: Activación del Linfocito T Proliferación CD28 Célula T Moléculas coestimulatorias B7 APC Supervivencia Activación Célula T TCR MHC Abbas AK et al. Cellular and Molecular Immunology. 6th ed. Philadelphia, PA: Elsevier Saunders, 2010 Producción Citoquinas Blocking CTLA-4 and PD-1 pathways F. Presentacion Ag F. Efectora o citotóxica T cell T cell Cel Dendritica G.Linfatico Señales Activacion B7 CD28 Señales Inhibitorias B7 CTLA-4 Anti cpo Tejidos perifericos TCR MHC Cancer cell TCR MHC Cancer cell T cell Regulación Negativa PD-L1 PD-1 Anti cpo Anti cpo Sinapsis Inmunológica: Regulación función Linfocitos T Sinapsis Inmunológica: Regulación función Linfocitos T Nirschl CJ Clin Cancer Res 2013 Sinapsis Inmunológica: Regulación función Linfocitos T Glennie M. BJCP 2013 Regulating the T cell immune response Activating receptors Inhibitory receptors CTLA-4 CD28 PD-1 OX40 TIM-3 CD137 LAG-3 Agonistic antibodies Antagonistic (blocking) antibodies • T cell responses are regulated through a complex balance of inhibitory (‘checkpoint’) and activating signals • Tumours can dysregulate checkpoint and activating pathways, and consequently the immune response • Targeting checkpoint and activating pathways is an evolving approach to cancer therapy, designed to promote an immune response T cell stimulation aThe image shows only a selection of the receptors/pathways involved. CD = cluster of differentiation; CTLA-4 = cytotoxic T-lymphocyte antigen-4; LAG-3 = lymphocyte-activation gene 3; PD-1 = programmed cell death TIM-3 = T-cell immunoglobulin domain and mucin domain 3. Adapted from Mellman I, et al. Nature. 2011:480;481–489; Pardoll DM. Nat Rev Cancer. 2012;12:252–264. Objetivos de la Charla: Revisar los fundamentos científicos de la inmuno-oncología en el cáncer de pulmón y en qué se diferencia de otras modalidades de tratamiento. Discutir los últimos avances en inmunoterapia para el tratamiento del cáncer de pulmón. Analizar el problema de la identificación de biomarcadores para las terapias inumono-oncológicas y su potencial valor predictivo. Valorar el potencial de la inmunoterapia sola o en combinación con otras modalidades de tratamiento en la práctica clínica. Immuno-Oncology: an emerging immunotherapy strategy for NSCLC Immunotherapy Passive (adoptive) Active Designed to act on the immune system itself Antigen dependent Antigen independent Enhancing immune cell function Therapeutic vaccines Modulate T cell function Cytokines GSK1572932A TG4010 Belagenpumatucel-L Tergenpumatucel-L Racotumomab L-BLP25 CIMAvax Designed to act at tumour; immune-based mechanism Anti-tumour mAbs Adoptive Bavituximab EGFR inhibition Adoptive cell transfer Immuno-Oncology CTLA-4 inhibition PD-1 inhibition PD-L1 inhibition . EGFR = epidermal growth factor receptor. www.clinicaltrials.gov. Accessed September 2014; NCCN Guidelines. Non-small cell lung cancer. v3.2014; Peters S, et al. Ann Oncol. 2012;23:vii56–vii64. Blocking CTL4 and PD-1/PD-L1 Patway Un agente único es capaz de proporcionar beneficio clínico en múltiples líneas de tratamiento y con largos supervivientes. Anti-PD-1 demonstrates encouraging survival in pre-treated patients: Nivolumab as an example CA209-003: phase 1 follow-up study, up to 5 prior lines of therapy, stage IIIB/IV squamous and non-squamous NSCLC cohort Dose (mg/kg) Died/ Treated ORR, % (n/N) Median OS (95% CI) 1.0 Overall survival 1-year OS 2-year OS 1 26/33 3.0 (1/33) 9.2 (5.3, 11.1) 32 (16, 49) [8] 12 (3, 27) [2] 3 20/37 24.3 (9/37) 14.9 (7.3, —) 56 (38, 71) [17] 45 (27, 61) [9] 10 48/59 20.3 (12/59) 9.2 (5.2, 12.4) 40 (27, 52) [23] 19 (10, 31) [9] 0.8 0.6 OS rate, % (95% CI) [patients at risk] 0.4 0.2 0.0 0 Patients at risk 1 mg/kg 3 mg/kg 10 mg/kg 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 54 57 0 1 2 0 1 1 0 1 0 0 1 0 0 1 0 0 0 0 0 0 0 Months since treatment initiation 33 37 59 26 34 51 21 26 35 16 21 29 8 17 23 6 13 16 5 12 14 5 11 12 2 9 9 1 4 4 0 1 3 0 1 2 0 1 2 70% of patients had 3–5 prior lines of therapy; 46% of these patients had received 12 prior lines of therapy and 54% had received 35 prior lines of therapy. Gettinger NS et al. J Clin Oncol. 2015; 33 Anti-PD-1 clinical activity in pre-treated patients: Pembrolizumab as an example KEYNOTE 001: phase 1 study of pre-treated patients, stage IV NSCLC RECIST v1.1 Immune-related response criteria PD-L1 positive PD-L1 negative PD-L1 positive PD-L1 negative n = 159 n= 35 n = 177 n = 40 ORR, % (95% CI) 23 (16, 30) 9 (2, 23) 19 (14, 26) 12 (4, 27) Disease control rate, % (95% CI) 42 (34, 50) 31 (17, 49) 51 (44, 59) 53 (36, 69) 9 (6, 31) 14 (9, 18) 9 (6, 22) 13 (9, 18) 31 (0+ to 37+) NR (9+ to 22+) NR (0+ to 37+) NR (0+ to 30+) n = 177 n= 40 n = 177 n = 40 11 ( 9, 16) 10 (9, 16) 16 (10, 18) 16 (9, 28) Best overall response* Time to response, weeks, median (range) Response duration, weeks, median (range) PFS Median, weeks (95% CI) • Most common treatment-related AE: fatigue 20% • 10% experienced ≥1 grade 35 treatment-related AEs – Incidence of fatigue, arthralgia and nausea, <1% each • Grade 3–4 pneumonitis occurred in 2 patients in each dosing arm • Grade 3–4 immune-related AEs occurred in 2 patients in each dosing arm and included: – Fatigue, arthralgia and neck pain *Includes confirmed and unconfirmed responses as assessed in patients with measurable disease at baseline. Garon E, et al. Oral presentation at ASCO 2014 (Abstract 8020). Anti-PD-L1 clinical activity and safety in pre-treated patients: MEDI-4736 as an example Phase 1 dose expansion study, ≥1 prior lines of therapy, stage IIIB/IV squamous and non-squamous NSCLC cohort ORR RECIST v1.1, n/N (%) MEDI-4736 10 mg/kg Q2W* MEDI-4736 all evaluated doses 6/47 (13) 9/58 (16) PD-L1 positive 5/13 (39) 5/20 (25) PD-L1 negative 1/19 (5) 1/29 (3) Total evaluable • • • No DLTs in Q2W or Q3W dose phases during dose escalation No drug-related AEs leading to discontinuation Low rates of treatment-related grade 34 AEs – • • 10 mg/kg Q2W, 4%; all doses: 3% The most common related grade ≥3 AE was arthralgia (1%) No drug-related colitis; no grade 34 pneumonitis or dyspnoea *MEDI-4736 10 mg/kg Q2W for up to 1 year for study expansion. Approximately 45% of patients had ≥3 prior lines of therapy. Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8021). Anti-PD-L1 clinical activity and safety in pre-treated patients: MPDL3280A as an example Phase 1a expansion study ongoing, ≥1 prior lines of therapy, stage IIIB/IV NSCLC cohort RECIST 1.1 ORR*, % SD ≥ 24 weeks, % 24-week PFS rate, % 21 19 42 23 17 45 Non-squamous (n = 42) 21 17 44 Squamous (n = 11) 27 18 46 Overall (N = 175) NSCLC (n = 53) • • • • • The majority of AEs were grade 12 and did not require intervention There was no maximum tolerated dose or dose-limiting toxicities No grade 35 pneumonitis observed Treatment-related death (cardio-respiratory arrest) in one patient with sinus thrombosis and large tumour mass invading the heart at baseline Immune-related grade 34 AE observed in one patient with large cell neuroendocrine NSCLC (diabetes mellitus, 1%) *ORR includes investigator-assessed unconfirmed and confirmed PR. 55% of patients had ≥3 prior lines of therapy. Soria J, et al. Oral presentation at ECC 2013 (Abstract 3408). Phase 3 study of Nivolumab compared with docetaxel in second- line advanced/metastatic squamous cell NSCLC (CA209-017/NCT01642004) Phase 3 study of Nivolumab compared with docetaxel in second- line advanced/metastatic squamous cell NSCLC (CA209-017/NCT01642004) Anti-PD-1 clinical activity and safety as 1st-line treatment: nivolumab as an example CA209-012: phase 1 study interim results, chemotherapy-naïve, stage IIIB/IV squamous or non-squamous NSCLC cohort Nivolumab 3 mg/kg IV Q2W Squamous (n = 9) Non-squamous (n = 11) Total (N = 20) 2 (22) [2.8, 60.0] 4 (36) [10.9, 69.2] 6 (30) [11.9, 54.3] Complete response* 1 (11) 1 (9) 2 (10) Partial response* 1 (11) 3 (27)† 4 (20) Stable disease 3 (33) 4 (36) 7 (35) Progressive disease 4 (44) 2 (18) 6 (30) Unable to determine 0 1 (9) 1 (5) 44 (14, 72) 73 (37, 90) 60 (36, 78) Median PFS, weeks (range) 15.1 (5.9, 63.3+) 47.3 (9.6, 80.7+) 36.1 (5.9, 80.7+) 1-year OS rate, % (95% CI) 67 (28, 88) 82 (45, 95) 75 (50, 89) Median OS, weeks (range) 68.0 (13.3, 73.1) NR (16.6, 89.1+) NR (13.3, 89.1+) ORR, n (%) [95% CI] Best overall response, n (%) PFS rate at 24 weeks, % (95% CI) • • • Treatment-related AEs (all grades), n = 17 (85%), most frequently fatigue n = 8 (40%) No pneumonitis (any grade) was observed Five treatment-related grade 34 AEs were reported in 4 patients (20%) – – Increased AST or ALT, hyperglycaemia, rash and cardiac failure, n = 1 each All resolved with treatment discontinuation and/or management per guidelines *Confirmed responses by a subsequent tumour assessment per RECIST 1.1; †One patient with confirmed partial response had unconfirmed CR by the time of this analysis. NR = not reached; + = response ongoing. Gettinger S, et al. Poster presented at ASCO 2014 (Abstract 8024). Anti-PD-1 clinical activity as 1st-line treatment: pembrolizumab as an example KEYNOTE 001: phase 1 study of patients with treatment-naïve, PD-L1 positive ≥1%, stage IV NSCLC RECIST v1.1 • n ORR n (%) [95% CI] n ORR n (%) [95% CI] 2 mg/kg Q3W 6 2 (33) [4, 78%] 6 4 (67) [22, 96] 10 mg/kg Q3W 20 4 (20) [6, 44] 22 10 (46) [24, 68] 10 mg/kg Q2W 16 5 (31) [11, 59] 17 7 (41) [18, 67] Total 42 11 (26) [14, 42] 45 21 (47) [32, 62] Interim median PFS: – RECIST v1.1 central review: 27.0 weeks (95% CI: 13.6, 45.0) – irRC investigator review: 37.0 weeks (95% CI: 27.0, NR) • Most common treatment-related AE: fatigue 10/45 patients (22%) • Grade 34 treatment-related AEs, all n = 1: – • irRC Blood creatine phosphokinase increase (grade 4), pericardial effusion (grade 3), pneumonitis (grade 3) Discontinuation due to AEs: acute kidney injury (grade 2), pneumonitis (grade 3) NR = not reached. Rizvi N, et al. Oral presentation at ASCO 2014 (Abstract 8007). Blocking CTL4 and PD-1/PD-L1 Patway Un agente único es capaz de proporcionar beneficio clínico en múltiples líneas de tratamiento y con largos supervivientes. Toxicidad clase específica con un perfil de seguridad manejable Common immune-related adverse events experienced with I-O therapies Pneumonitis (anti-PD-1) Rash (anti-CTLA-4)1 Reticular erythematous rash Perivascular lymphocyte infiltrate extending into epidermis Gastrointestinal adverse events (anti-CTLA-4)2 Colonoscopy Histopathology Bowel oedema and ulceration in the descending colon Focal active colitis (left) with crypt destruction, loss of goblet cells, and neutrophilic infiltrates in the crypt epithelium (right) 1. Hodi F, et al. Proc Natl Acad Sci USA. 2003;100:4712–4717; 2. Maker A, et al. Ann Surg Oncol. 2005;12:1005–1016. Select adverse events (≥1%) in patients with NSCLC treated with nivolumab • • Demonstrates a safety profile managed by protocol algorithms No new safety signals emerging; all patients >1 year of follow-up Patients, n (%) [N = 129] Any grade Grade 34 41 (53) 5 (6) Skin 16 (20) 0 Gastrointestinal 12 (15) 1 (1) Pneumonitis 8 (6) 3 (2)† Pulmonary 7 (9) 2 (3) Endocrinopathies 6 (8) 0 Hepatic 5 (6) 1 (1) Infusion reaction 4 (5) 1 (1) Renal 3 (4) 0 Any treatment-related select adverse event* *Defined as an event with potential immunological aetiologies that require more frequent monitoring and/or unique intervention. †2/3 cases were fatal. Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8112). Inhibition of CTL4 and PD-1/PD-L1 Patway Un agente único es capaz de proporcionar beneficio clínico en múltiples líneas de tratamiento y con largos supervivientes. Toxicidad clase específica con un perfil de seguridad manejable Respuestas rápidas y duraderas independientes del tipo histológico y de la presencia mutaciones. Anti-PD-1 response by histology: nivolumab as an example CA209-003: phase 1 follow-up study, up to 5 prior lines of therapy, stage IIIB/IV NSCLC cohort Time to and duration of response while on treatment Ongoing response Squamous (n = 9) Time to response Response duration following latest reported dose of therapy Non-squamous (n = 13) 0 16 32 48 64 80 96 112 128 144 160 Time , weeks Responses were durable and occurred early • 50% of patients (11/22) with ORs demonstrated response at first assessment (8 weeks) • Responses ongoing in 45% of patients (10/22) at time of analysis • 38% of responders (6/16) who discontinued for reasons other than PD responded for >30 weeks after last nivolumab dose; responses in 83% of patients (5/6) ongoing at the time of reporting Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8112). Anti-PD-1 survival rates appear independent of histology: nivolumab as an example 1.0 Overall survival 0.9 Group Died/TreatedMedian OS (95% CI) Squamous 38/54 9.2 (7.3, 12.5) Non-squamous 55/74 10.1 (5.7, 13.7) Censored 0.8 0.7 0.6 0.5 1-year OS Rate = 43% 0.4 1-year OS Rate = 40% 2-year OS Rate = 24% 2-year OS Rate = 23% 0.3 0.2 0.1 0.0 0 Patients at Risk Squamous Non-squamous 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 54 2 0 1 0 1 0 1 0 0 0 Months since treatment initiation 54 74 44 66 36 45 26 39 19 28 12 22 11 19 Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8112). 10 17 9 10 4 5 3 1 2 1 2 1 2 1 Response to anti-PD-1 by EGFR or KRAS mutation status: nivolumab as an example Subgroup ORR, % (n/N) [95% CI] EGFR status Mutant 17 (2/12) [2.1, 48.4] Wild-type 20 (11/56) [10.2, 32.4] Unknown 15 (9/61) [7.0, 26.2] 120 100 Mutant Unknown Wild-type 60 40 20 0 -20 -40 -60 -80 -100 Patients KRAS status 120 Wild-type 25 (9/36) [12.1, 42.2] Unknown 14 (10/72) [6.9, 24.1] KRAS mutation status 100 14 (3/21) [3.0, 36.3] Change in tumour size, % Mutant EGFR mutation status 80 Change in tumour size, % CA209-003: phase 1 follow-up study, up to 5 prior lines of therapy, NSCLC cohort Mutant Unknown Wild-type 80 60 40 20 0 -20 -40 -60 -80 Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8112). -100 Patients Objetivos de la Charla: Revisar los fundamentos científicos de la inmuno-oncología en el cáncer de pulmón y en qué se diferencia de otras modalidades de tratamiento. Discutir los últimos avances en inmunoterapia para el tratamiento del cáncer de pulmón. Analizar el problema de la identificación de biomarcadores para las terapias inumono-oncológicas y su potencial valor predictivo. Valorar el potencial de la inmunoterapia sola o en combinación con otras modalidades de tratamiento en la práctica clínica. Understanding of NSCLC subtyping has evolved in parallel with treatment strategies Lung cancer as 2 main diseases1–2 Current NSCLC landscape4–8 Tumour histology and genotype influence treatment selection (From 2011) Chemotherapy only (1990s) SCLC <15% NSCLC >85% Non-squamous NSCLC – adenocarcinoma1,2 (~40%) †,3 NSCLC: histology-based subtyping3 NRAS, 1% PDGFR, 1% EGFR, 15% VEGFR, 1% AKT1, 1% MEK1, 1% ROS1, 1% ALK, 7% BRAF, 3% RET, 1% Chemotherapy and targeted therapies (Early 2000s) Large cell 7% Other* 8% HLA-A, 3% ADC 36% Squamous 49% Squamous NSCLC4,5 (~2530%) †,3 KRAS, 25% Unknown, 35% FGFR2, 3% HER2, 4% BRAF, 4% DDR2, 4% PDGFRA, HER2, 2% MET, PI3K, 3% 3% Unknown, 18% PIK3CA, 16% † EGFR, 9% PTEN, 15% FGFR1, 15% 9% *Bronchioloalveolar carcinoma 6%, adenosquamous 2%; †Of all histologies. 1. Carney DN. N Engl J Med. 2002;346:126–28; 2. American Cancer Society. Lung Cancer (Small Cell). Available from http://www.cancer.org/cancer/lungcancersmallcell/detailedguide/small-cell-lung-cancer-what-is-small-cell-lung-cancer. Accessed September 2014; 3. Chansky K, et al. J Thorac Oncol. 2009;4:792-801; 4. Pao W, et al. Lancet Oncol. 2011;12:175–180; 5. Molecular profiling of lung cancer. Available at http://www.mycancergenome.org/content/disease/lung-cancer. Accessed September 2014; 6. American Cancer Society. Lung Cancer (Non-Small Cell); What is non-small cell lung cancer? Available at http://www.cancer.org/cancer/lungcancer-nonsmallcell/detailedguide/non-small-cell-lung-cancer-what-is-non-small-cell-lung-cancer. Accessed September 2014; 7. Kim HS, et al. Lung Cancer. 2013;80:249–255; 8. The Cancer Genome Atlas Research Network. Nature. 2012;489:519–525. Prognostic/predictive biomarkers in NSCLC Prognostic Predictive Provides information on outcome, independent of the administered therapy1 Provides information on outcome with regards to a specific therapy1 Ki672 MCM72 p533,4 • • ALK5 ERCC15 BRAF5,6 EGFR5,7 KRAS5,7 MET5,8 PD-L1?9,10 HER25 RET5 ROS15 Routine assessment recommended for EGFR and ALK only5 A number of additional potential predictive or prognostic biomarkers are being further investigated, e.g. AKT, BRCA1, PIK3CA, RRM1 and TS11,12 1. Oldenhius CNAM, et al. Eur J Cancer. 2008;44:946–953; 2. Liu YZ, et al. Lung Cancer. 2012;77:176-182; 3.Steels E, et al. Eur Respir J. 2001;18:705–719; 4. Tsao M-S, et al. J Clin Oncol. 2007;25:5240-5247; 5. Peters S, et al. Ann Oncol. 2012;23(suppl 7):vii56–vii64; 6. Marchetti A, et al. J Clin Oncol. 2011;29:3574–3579; 7. Eberhard D, et al. J Clin Oncol. 2005;23:5900–5909; 8. Cappuzzo F, et al. J Clin Oncol. 2009;27:1667–1674; 9. Mu C, et al. Med Oncol. 2011;28:682–688; 10. Garon E, et al. Oral presentation at WCLC 2013. (Abstract 2416); 11. Pao W and Girard N. Lancet Oncol. 2011;12:175–180; 12. Rothschild S, et al. Curr Opin Oncol. 2011;23:150–157. Lack of definitive biomarkers associated with anti-CTLA-4 therapy Potential predictive biomarker Association with anti-CTLA-4 treatment Absolute lymphocyte count (ALC) • ALC ≥1000 μL after 2 ipilimumab treatments (week 7) correlates with improved clinical benefit and OS1–4 CD8+/CD4+ T cells Absolute CD8+ T cell count • Clinical activity relates to increased frequency of absolute numbers of CD8+ cells2,4 ICOS • Positive correlation between clinical activity and frequency of CD8+ ICOShigh T cells4 • Correlation between CD4+ ICOShigh T cells and increased OS4 Tregs FOXp3 • Clinical activity relates to high protein expression2,5 IDO • Clinical activity relates to high protein expression2,5 1. Ascierto P, et al. Clin Cancer Res. 2013;19:1009–1020; 2. Hamid O, et al. J Transl Med. 2011;9:204; 3. Ku G, et al. Cancer. 2010;116:1767–1775; 4. Callahan M et al. Semin Oncol. 2010;37:473–484; 5. Ascierto P, et al. J Transl Med. 2013;11:54. ALC Treg cells 1.0 Individual responder 0.5 Individual nonresponder 0.0 Responder mean -0.5 Nonresponder mean C6D1 C5D1 C4D1 C3D1 C2D1 -1.0 Baseline flow cytometry value (cells/μL) 3 mg/kg C6D1 C1D1 ALC change from baseline (×10*3 c/μL) Biomarkers not predictive of response to anti-PD-1 350.00 300.00 250.00 200.00 150.00 100.00 50.00 0.00 -50.00 N=37 NSCLC No response N=14 NSCLC Response Brahmer J, et al. Poster presented at ELCC 2014 (Abstract 96PD). 100.00 50.00 0.00 -50.00 N=37 N=14 NSCLC No response NSCLC Response Activated CD4+ T cells Baseline flow cytometry value (cells/μL) Baseline flow cytometry value (cells/μL) Activated CD8+ T cells 150.00 200.00 150.00 100.00 50.00 0.00 N=37 N=14 -50.00 NSCLC No response NSCLC Response PD-L1 expression and response to anti-PD-1/anti-PD-L1 agents in NSCLC Nivolumab1,2 (anti-PD-1) Pembrolizumab3,4 (anti-PD-1) MEDI-47365 (anti-PD-L1) MPDL3280A6,7 (anti-PD-L1) Pre-treated (All doses) Pre-treated (All doses) Pre-treated1 (All doses) 1st-line2 (3 mg/kg dose) Pre-treated3 (10 mg/kg dose) 1st-line4 (All doses) Overall 22/129 (17) 6/20 (30) NR/194 (20) NR 9/58 (16) 12/53 (23) PD-L1+ 5/33 (15) 5/10 (50) NR/159 (23) 11/42 (26) 5/20 (25) IHC 3: 5/6 (83) IHC 2: 1/7 (14) IHC 1: 2/13 (15) PD-L1 5/35 (14) 0/7 NR/35 (9) NR 1/29 (3) IHC 0: 4/20 (20) Overall 2.3 mos 36.1 wks NR NR NR NR PD-L1+ 3.6 mos 45.6 wks 11 wks NR NR NR PD-L1 1.8 mos 36.1 wks 10 wks NR NR NR Overall 9.9 mos Not reached NR NR NR NR PD-L1+ 7.8 mos Not reached NR NR NR NR PD-L1 10.5 mos Not reached NR NR NR NR ORR, n/N (%) Median PFS Median OS NR = not reported. 1. Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8112); 2. Gettinger S, et al. Poster presented at ASCO 2014 (Abstract 8024); 3. Garon E, et al. Poster presented at ASCO 2014 (Abstract 8020); 4. Rizvi N, et al. Oral presentation at ASCO 2014 (Abstract 8007); 5. Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8021); 6. Soria J, et al. Oral presentation at ECC 2013 (Abstract 3408); 7. Soria J-C, et al. Poster presented at ESMO 2014 (Abstract 1322P). PD-L1 expression and response to anti-PD-1/anti-PD-L1 agents in NSCLC PD-L1 analysis: differences in evaluation and interpretation Agent Assay Analysis Definition of positivity Nivolumab (anti-PD-1) 14 Dako automated IHC assay (28-8 rabbit Ab) Analytically validated Pembrolizumab (anti-PD-1)5,6 PD-L1 expression • Archival FFPE • 1% and 5% cut-off among >100 evaluable tumour cells • 56%: 1% cut-off • 49%: 5% cut-off Dako automated • New tumour biopsy IHC assay within 60 days prior (22C3 mouse Ab) to first dose of pembrolizumab • Tumour dependent: - Melanoma > 1% - NSCLC PD-L1 (+): Strong (≥50%) and weak staining (1–49%) PD-L1 (–): no staining • ~25%: ≥50% staining • ~45–70%: ≥1% staining MPDL3280A (anti-PD-L1)7,8,9 Ventana • Archival FFPE automated clinical research IHC assay • PD-L1 (+): IHC 3 (≥10%), IHC 2,3 (≥5%), IHC 1,2,3 (≥1%) • PD-L1 (–): IHC 0 (<1%) • 11%: IHC 3 • 25%: IHC 2 and 3 • 49%: IHC 1/2/3 MEDI-4736 (anti-PD-L1)10 First-generation • Archival FFPE or Ventana IHC Automated Assay (in development) • Not reported • Not reported 1. Antonia S, et al. Poster presented at WCLC 2013 (Abstract P2.11-035); 2. Brahmer J, et al. Poster 293 presented at ASCO 2014 (Abstract 8112); 3. Gettinger S, et al. Poster presented at ASCO 2014 (Abstract 8024); 4. Topalian S, et al. N Engl J Med. 2012;366:2443–2454; 5. Garon E, et al. Poster presented at ASCO 2014 (Abstract 8020); 6. Gandhi L, et al. Oral presentation at AACR 2014 (Abstract CT105); 7. Soria J, et al. Oral presentation at ECC 2013 (Abstract 3408); 8. Rizvi N, et al. Poster presented at ASCO 2014 (Abstract TPS 8123); 9. Soria J, et al. Poster presented at ESMO 2014 (Abstract 1322P); 10. Brahmer J, et al. Poster presented at ASCO 2014 (Abstract 8021). Limitations associated with the assessment of tumour PD-L1 expression Tumour heterogeneity Tissue acquisition Role of fresh vs archived samples PD-L1 expression • Numerous histological subtypes and diverse genomic aberrations in patients with NSCLC • Intratumour heterogeneity with markers for both poor and good prognosis within the same tumour • Limited sample size • Difficult to retain tissue architecture and tumour microenvironment • Aging of FFPE tissue sections causes degradation of epitopes and DNA • Age, gender, histology and stage of disease appear associated with PD-L1 expression in patients with NSCLC • May change after exposure to treatment FFPE = formalin fixed, paraffin‐embedded. Li T, et al. J Clin Oncol. 2013;31:1039–1049; Thomas A, et al. Ann Oncol. 2013;24:577–585; Gerlinger M, et al. N Engl J Med. 2012;366:883–889; Kerr K, et al. Ann Oncol. 2014 Apr 8. [Epub ahead of print]; Sun J-M, et al. Poster presented at ASCO 2014 (Abstract 8066). PD-L1 expression is dynamic and may change after exposure to treatment Baseline CD8 T cells On-treatment PD-L1 CD8 T cells PD-L1 MPDL3280A T cells and tumour cells expressing PD-L1 Powderly J, et al. Oral presentation at ASCO 2013 (Abstract 3001). Objetivos de la Charla: Revisar los fundamentos científicos de la inmuno-oncología en el cáncer de pulmón y en qué se diferencia de otras modalidades de tratamiento. Discutir los últimos avances en inmunoterapia para el tratamiento del cáncer de pulmón. Analizar el problema de la identificación de biomarcadores para las terapias inumono-oncológicas y su potencial valor predictivo. Valorar el potencial de la inmunoterapia sola o en combinación con otras modalidades de tratamiento en la práctica clínica. Therapies that Might Affect the Cancer-Immunity Cycle Chen DS and Mellman I. Immunity. 2013;39. Base de la combinación de inmunoterapias Inmunoterapias combinadas I-O agents have a unique MoA, offering the opportunity for combination with other agents I-O Drake C. Ann Oncol. 2012;23(suppl 8):viii41–viii46; Hannani D, et al. Cancer J 2011;17:351–358; Ménard C, et al. Cancer Immunol Immunother. 2008;57:1579–1587; Ribas A, et al. Curr Opin Immunol. 2013:25:291–296. Anti-PD-1 plus TKI in EGFR TKI-resistant NSCLC: nivolumab plus erlotinib as an example CA209-012: phase 1 study interim results, chemotherapy-naïve, stage IIIB/IV EGFR mutation-positive NSCLC* Patient 1 (T790M-positive) * * 2 3 Time to and duration of response on treatment Ongoing response Time to response * 4 (Erlotinib-naïve) * * 0 6 12 18 24 30 36 42 48 54 60 66 72 78 84 90 Duration of study drug exposure at time of data analysis (dosing beyond progression) Response duration following latest reported dose of therapy Time, weeks Nivolumab + erlotinib (N = 21) ORR, n (%) [95% CI] 4 (19) [5.4, 41.9] Estimated median DOR, weeks (95% CI) NR (60.1, ) PFS rate at 24 weeks, % (95% CI) 51 (28, 70) Median PFS, weeks (range) 29.4 (4.6, 81.7+) 1-year OS rate, % (95% CI) 71 (46, 88) Median OS, weeks (range) NR (10.7+, 86.9+) *20/21 patients received prior erlotinib and represented a refractory population. Rizvi N, et al. Poster presented at ASCO 2014 (Abstract 8022). I-O agents have a unique MoA, offering the opportunity for combination with other agents I-O Drake C. Ann Oncol. 2012;23(suppl 8):viii41–viii46; Hannani D, et al. Cancer J 2011;17:351–358; Ménard C, et al. Cancer Immunol Immunother. 2008;57:1579–1587; Ribas A, et al. Curr Opin Immunol. 2013:25:291–296. Anti-CTLA-4 plus chemotherapy as 1st-line treatment: ipilimumab plus carboplatin/paclitaxel as an example CA184-041: phase 2 study results, no prior therapy for lung cancer, stage IIIB/IV NSCLC, ECOG PS ≤1, all histologies Ipilimumab + concurrent chemotherapy Ipilimumab + phased chemotherapy 1.0 irPFS, probability irPFS, probability 1.0 0.8 0.6 0.4 0.2 0 0.8 0.6 0.4 0.2 0 0 2 4 6 8 10 12 14 16 0 2 4 Placebo Ipilimumab 55/70 Median irPFS, months 4.63 5.52 95% CI 4.14, 5.52 HR P- value 4.17, 6.74 0.81 Lynch T, et al. J Clin Oncol. 2012;30:2046–2054. 8 10 12 14 16 Time, months Time, months Events/ patients 56/66 6 Placebo 0.13 Events/ patients 56/66 Ipilimumab 54/68 Median irPFS, months 4.63 5.68 95% CI HR P -value 4.14, 5.52 4.76, 7.79 0.72 0.05 Anti-PD-1 plus chemotherapy as 1st-line treatment: nivolumab plus platinum-based regimens as an example Change in baseline target lesions, % CA209-012: phase 1 study interim results, chemotherapy-naïve, stage IIIB or IV NSCLC, ECOG PS ≤1, all histologies 40 20 0 -20 -40 -60 -80 -100 Nivolumab 10 mg/kg + Gem/Cis (squamous) Nivolumab 10 mg/kg + Pem/Cis (non-squamous) Nivolumab 10 mg/kg + Pac/Carb (any histology) Nivolumab 5 mg/kg + Pac/Carb (any histology) Nivolumab 10 mg/kg Nivolumab 5 mg/kg Gem/Cis (n = 12) Pem/Cis (n = 15) Pac/Carb (n = 15) Pac/Carb (n = 14) 4 (33) [10, 65] 7 (47) [21, 73] 7 (47) [21, 73] 6 (43) [18, 71] 45.0 (17.7, 56.7) 25.4 (13.1, ) 23.9 (12.3, ) NR (22.0, ) 51 (19, 76) 71 (39, 88) 38 (14, 61) 51 (21, 75) Median PFS, weeks (range) 24.7 (0.1+, 61.4) 29.7 (4.0+, 91.9+) 21.0 (3.1, 97.9+) 31.0 (0.1+, 82.4+) 1-year OS rate, % (95% CI) 50 (21, 74) 87 (56, 96) 60 (32, 80) 85 (51, 96) Median OS, weeks (range) 50.5 (19.7, 99.3+) 83.4 (33.0, 105.1+) 64.9 (13.9, 105.0+) NR (33.7+, 87.1+) ORR, n (%) [95% CI] Est. median DOR, weeks (95% CI) PFS rate at 24 weeks, % (95% CI) Cis = cisplatin; Gem = gemcitabine; Pem = pemetrexed; Pac = paclitaxel; Carb = carboplatin. Includes patients with baseline target lesion and ≥1 post-baseline target lesion assessment with non-missing value. Antonia S, et al. Poster presented at ASCO 2014 (Abstract 8113); Antonia S, et al. Presented at LALCA 2014 (Abstract O.3). I-O agents have a unique MoA, offering the opportunity for combination with other agents I-O Drake C. Ann Oncol. 2012;23(suppl 8):viii41–viii46; Hannani D, et al. Cancer J 2011;17:351–358; Ménard C, et al. Cancer Immunol Immunother. 2008;57:1579–1587; Ribas A, et al. Curr Opin Immunol. 2013:25:291–296. Anti-PD-1 plus anti-CTLA-4 tumour response and survival outcomes: nivolumab plus ipilimumab as an example Change in baseline target lesions, % 200 CA209-012: phase 1 study interim results, chemotherapy-naïve, non-squamous/squamous stage IIIB/IV NSCLC 180 160 140 120 100 80 60 40 20 0 -20 -40 -60 -80 Includes patients with baseline target lesion and ≥1 post-baseline target lesion assessment with non-missing value. -100 Nivolumab 1 mg/kg + ipilimumab 3mg/kg (squamous) Nivolumab 1 mg/kg + ipilimumab 3mg/kg (non-squamous) Nivolumab 3 mg/kg + ipilimumab 1mg/kg (squamous) Nivolumab 1 mg/kg + ipilimumab 3 mg/kg PFS rate at 24 weeks, % (95% CI) Median PFS, weeks (range) Median OS, weeks (range) Nivolumab 3 mg/kg + ipilimumab 1mg/kg (non-squamous) Nivolumab 3 mg/kg + ipilimumab 1 mg/kg Squamous (n = 9) Non-squamous (n = 15) Squamous (n = 9) Non-squamous (n = 16) 25 (4, 56) 51 (21, 74) 44 (14, 72) 20 (5, 43) 41 (20, 61) 8.9 (0.1+, 44.7) 32.9 (0.1+, 54.1+) 16.1 (0.1+, 54.1+) 44.3 (1.4, 53.1+) NR (4.9+, 54.1+) NR (1.4, 54.1+) Antonia S, et al. Poster presented at ASCO 2014 (Abstract 8023). 29 (13, 48) 20.6 (9.7, 33.3+) 9.9 (4.1+, 58.1+) 14.4 (4.1+, 58.1+) NR (9.7, 50.1+) NR (8.1, 58.1+) NR (8.1, 58.1+) I-O agents have a unique MoA, offering the opportunity for combination with other agents I-O Drake C. Ann Oncol. 2012;23(suppl 8):viii41–viii46; Hannani D, et al. Cancer J 2011;17:351–358; Ménard C, et al. Cancer Immunol Immunother. 2008;57:1579–1587; Ribas A, et al. Curr Opin Immunol. 2013:25:291–296. Potential of anti-CTLA-4 plus radiation: ipilimumab in one patient with melanoma as an example • • The target and other lesions regressed Regression of distant lesions may be due to an enhanced systemic response A B August 2009 C November 2010 D January 2011 E April 2011 October 2011 Ipilimumab F Recurrence of unresectable cancer Induction Maintenance Stable December 2010 Aug. 2009 A Sept. 2009 Radiation Maintenance Slow Progression Dec. 2009 Figure adapted from Postow M, et al. N Engl J Med. 2012;366(10): 925–931. Nov. 2010 A Response Dec. 2010 B Jan. 2010 C Stable April 2010 D Oct. 2010 E Examples of ongoing combination trials with I-O therapies Chemotherapy Radiotherapy Targeted Immunotherapy Nivolumab (anti-PD-1) + cisplatin/gemcitabine, cisplatin/pemetrexed or carboplatin/paclitaxel (NCT01454102) NR + bevacizumab or erlotinib (NCT01454102) + ipilimumab (NCT01454102) + anti-KIR (NCT01714739) + anti-LAG3 (NCT01968109) Pembrolizumab (anti-PD-1) + cisplatin/pemetrexed or carboplatin/paclitaxel (NCT01840579) + paclitaxel/carboplatin ± bevacizumab (NCT02039674) NR + gefitinib or erlotinib (NCT02039674) + ipilimumab (NCT02039674) + INCB024360 (NCT02178722) NR + gefitinib (NCT02088112) + AZD9291 (NCT02143466) + tremelimumab (NCT02000947, NCT02141347) + ipilimumab (NCT02174172) MEDI-4736 (anti-PD-L1) NR MPDL3280A (anti-PD-L1) NR NR + erlotinib (NCT02013219) + cobimetinib (NCT01988896) Ipilimumab (anti-CTLA-4) Various (NCT00527735; NCT01165216; NCT01285609; NCT01331525; NCT01450761;NCT1454102) + stereotactic radiosurgery* (NCT02107755, NCT02239900) + ionizing radiation (NCT02221739) + erlotinib or crizotinib (NCT01998126) + nivolumab (NCT01454102) + pembrolizumab (NCT02039674) Tremelimumab (anti-CTLA-4) NR NR + gefitinib (NCT02040064) + MEDI-4736 (NCT02000947) *Trial in patients with melanoma with metastatic disease to a visceral organ (lung, liver, brain, adrenal, nodal station outside the regional lymph drainage of the primary, vertebral bodies). NR = no trials reported. www.clinicaltrials.gov. Accessed September 2014. In summary Los agentes bloqueantes de los estímulos inhibitorios Inmunológicos han demostrao un potencial en respuestas duraderas a través de diferentes histologías, diferentes líneas de tratamiento e independiente de las mutaciones oncogénicas. La identificación de biomarcadores para terapias IO es compleja. Los futuros datos de los ensayos clínicos y el uso de métodos estandarizados de evaluación ayudarán a clarificar su papel pronóstico y predictivo en CPNM. Los AcMo IO ofrecen la oportunidad de tratamientos combinados con otros agentes IO y con otras modalidades de tratamiento, para aumentar aún más el potencial de beneficio clínico. La IO puede representar la base de los futuros tratamientos de los diversos tumores malignos sólidos o hematológicos, ofreciendo una posibilidad para la supervivencia a largo plazo.