Cardiac Output and Venous Return changed
advertisement
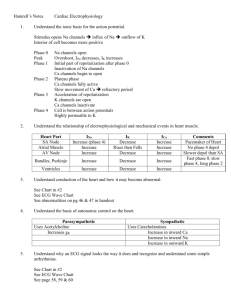
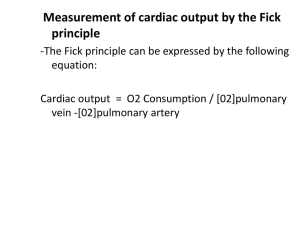
Cardiac Output and Venous Return Learning objectives • Define venous return. Understand the concept of “resistance to venous return” and know what factors determine its value. • Understand the principles underlying cardiac output measurements using the Fick principle, dye dilution, and thermodilution methods. • Know how cardiac function (output) curves are generated and how factors which cause changes in contractility in the heart can alter the shape of cardiac function curves. Learning objectives • Construct a vascular function curve. Predict how changes in total peripheral resistance, blood volume, and venous compliance influence this curve. • Use the intersection point of the cardiac function curve and vascular function curve to predict how interventions such as hemorrhage, heart failure, autonomic stimulation, and exercise will affect cardiac output and right atrial pressure. Cardiac output • Amount of blood ejected by each ventricle per minute is called cardiac output (CO). Its value is almost same for both the ventricles & is about 5L/min. in a normal adult male • Cardiac output = heart beat rate X stroke volume (stroke volume is amount of blood ejected/ventricle/beat or stroke = EDV-ESV) • CO = 72/min X 70ml = 5 L/min (approx.) Cardiac index: CI is the cardiac output per square meter of body surface area. Normal value is about 3 L/min/m2 (2.6 to 4.2 L/min/m2 ) Measurement of Cardiac Output • Calculation of flow through the pulmonary circuit provides a measure of the CO. Required data are: • oxygen consumption of the organ • A – V oxygen content (concentration) difference across the organ (not PO2) • In a test subject, oxygen consumption was measured at 700 mL/min.Pulmonary artery oxygen content was 140 mL per liter of blood and brachial artery oxygen content was 210 mL per liter of blood. Cardiac out-put was which of the following? a. 4.2 L/min b. 7.0 L/min c. 10.0 L/min d. 12.6 L/min e. 30.0 L/min Regulation of cardiac output • Factors effecting Regulation of Heart rate • Sympathetic & parasympathetic (vagus) nerves control the heart beat rate. • A normal heart beat is maintained by slow continuous discharge from sympathetic nerves • The vagal fibers are distributed mainly to atria than ventricles Regulation of Heart rate • Strong sympathetic stimulation can increase the heart rate from normal 70 beats / min. upto 180-200 beats / min. • Strong vagal stimulation bring down the rate to 20 40beats/min & also can decrease strength of heart muscle contraction by 20-30% 14-8 The output per minute per square meter of body surface is called A. Cardiac output B. Stroke volume C. Afterload D. Cardiac index E. Preload Baroreceptor Reflex Bainbridge Reflex, Atrial Receptors, and Atrial Natriuretic Peptide Respiratory Sinus Arrhythmia Determinants of Cardiac Output • Venous parameters, not arterial parameters, normally determine cardiac output. • Heart rate does not normally affect cardiac output but very low and very high heart rates impede venous return and cardiac output. • Increased resistance of arteries raises blood pressure but does not affect venous return and cardiac output. • For instance, aortic stenosis, coarc-tion of the aorta, and hypertension do not decrease cardiac output if the heart if able to pump against the increased afterload. Stroke Volume • Is determined by 3 variables: – Preload/End diastolic volume (EDV) = volume of blood in ventricles at end of diastole – Afterload/Total peripheral resistance (TPR) = impedance to blood flow in arteries – Contractility/Inotropy = strength of ventricular contraction 14-9 Regulation of Stroke Volume • EDV is workload (preload) on heart prior to contraction – SV is directly proportional to preload & contractility • Total peripheral resistance = afterload which impedes ejection from ventricle – SV is inversely proportional to TPR • SV is directly proportional to Contractility. Regulation of stroke volume 1. Preload :Passive tension in the muscle when it is being filled during diastole. • End diastolic volume • Venous return • Frank-Starling’s law (Energy of contraction is proportional to the initial length of cardiac muscle fibres) Preload General features • Preload is the load on the muscle in the relaxed state. • More specifically, it is the load or prestretch on ventricular muscle at the end of diastole. • Preload on ventricular muscle is not measured directly; rather, indices are utilized. • Indices of left ventricular preload: – Left ventricular end-diastolic volume (LVEDV) – Left ventricular end-diastolic pressure (LVEDP) • somewhat less reliable indices of left ventricular preload are those measured in the venous system. – Left atrial pressure – Pulmonary venous pressure – Pulmonary wedge pressure • Measurement of systemic central venous pressure is an index of preload on the right ventricle Question time again- In skeletal muscle the resting muscle length is approximately the optimal length at which maximal tension can be developed during a subsequent contractionA)True B)False. Frank-Starling Law of the Heart (a) is state of myocardial sarcomeres just before filling Actins overlap, actinmyosin interactions are reduced & contraction would be weak In (b, c & d) there is increasing interaction of actin & myosin allowing more force to be developed • The Frank–Starling law of the heart states that the stroke volume of the heart increases in response to an increase in the volume of blood filling the heart (the end diastolic volume) when all other factors remain constant. • Important in Balancing left and right ventricular Cardiac output. Fig. -. Frank-Starling Law of the heart. The graph illustrates the relationship between SV and changes in ventricular end-diastolic volume. The insets showing diagrammatic sarcomeres, illustrate the relationship between end-diastolic volume and myofilament overlap. Length-force relationships in intact heart: a Frank-Starling curve Optimal Length Figure 14-28 Factors affecting end-diastolic volume, e.g. the degree to which cardiac muscle is stretched Increase • Stronger atrial contraction • Increased total blood volume • Increased venous tone • Increased pumping action of skeletal muscle • Increased negative intrathoracic pressure Decrease • Standing • Increased intrapericardial pressure(Cardiac tamponade) • Decreased ventricular compliance •Pathological conditions such as ventricular systolic failure and valve defects such as aortic stenosis, aortic regurgitation (pulmonary valve stenosis and regurgitation have similar effects on right ventricular preload). B. Extrinsic Regulation of Stroke Volume • Any changes in the strength of cardiac contraction that occur independently of changes in EDV are referred to as changes in myocardial contractility • A change in myocardial contractility (Inotropism) is mechanistically different from the altered vigor of contraction seen with changes in muscle length • Changes in contractility are direct result of changes in the rate and extent of Ca2+ movement into the cytoplasm • Increased firing of cardiac sympathetic nerve results in in both the rate (chronotropic action) and extent (inotropic action) of myocardial contractions Relationship between contractility and intracellular Ca2+ : contractility is a result of cytoplasmic Ca2+ concentration. This is the result of both release of Ca2+ from the sarcoplasmic reticulum and influx of Ca2+ from the extracellular space. Increased Ca2+ results in activation of additional crossbridges (indicated in red) sympathetic Fig. 14. Effect of changes in myocardial contractility on the FrankStarling curve. The curve shifts downward and to the right as contractility is decreased. The major factors influencing contractility are summarized on the right (dashed lines indicate portions of the curve where maximum contractility has been exceeded). W.Ganong. Review of Medical Physiology Ejection Fraction – is the fraction of the enddiastolic volume that is ejected with each beat, that is, it is stroke volume (SV) divided by enddiastolic volume (EDV). stroke volume / end diastole volume X 100%, normal range, 55-65%. Commonly used as a clinical index for evaluating the inotropic state of the heart. Fig. . Changes in SV due to changes in contractility are mechanistically different from those occurring as a result of EDV. The two mechanisms can operate simultaneously to SV (lower panel). EDV = end- diastolic volume; ESV = end-systolic volume; SV = stroke volume (Human Physiology) Afterload and Cardiac Performance • Afterload: all the factors that impede fiber shortening, in this case it would be all the factors that impede the ejection of blood from the ventricle. What the heart has to pump against • • • • Volume of blood in the arterial circulation Pressure in aorta at onset of ejection (DAP) Compliance of aorta Size of outflow orifice Factors that affect stroke volume. Myocardial Hypertrophy Concentric • Cross sectional area of a muscle increases when repeatedly exposed to an elevated work load over a sustained period of time • In cardiac muscle this can be the result of increased wall tension caused by increased preload or increased after load . 51 eccentric Changes in the radius of the ventricles (curvature of the ventricle) can affect ventricular pressure (Laplace’s Law) and efficiency of the heart as a pump • The pressure generated in a sphere is directly proportional to the wall tension (T) developed, and inversely related to the radius of the sphere (r) (Law of Laplace) P = 2T/r • In normal conditions, during ejection phase of cardiac cycle the volume of blood in the V falls, and the r of the V decreases. As the radius falls, the tension in the V walls is more effective in ventricular pressure • In chronic cardiac failure the contractility is reduced and the heart becomes less effective as a pump and dilates radius of the ventricles and reduces its curvature, and ejection gets more difficult as it proceeds Normal P-V loop Increased Afterload Increased Preload Increased Contractility 1. The figure below shows pressure volume loops for two situations. When compared with loop A, loop B demonstrates (A) Increased preload (B) Decreased preload (C) Increased contractility (D) Increased afterload (E) Decreased afterload Which of the following would cause a decrease in stroke volume, compared with the normal resting value? (A) Reduction in afterload (B) An increase in end-diastolic pressure (C) Stimulation of the vagus nerves (D) Electrical pacing to a heart rate of 200 beats/min (E) Stimulation of sympathetic nerves to the heart Point Y in the figure below is the control point. Which point corresponds to a combination of increased contractility and increased ventricular filling? (A) Point A (B) Point B (C) Point C (D) Point D (E) Point E Summary of the regulation of Cardiac Output The Cardiac output is the volume of blood pumped by each ventricle and equals the product of heart rate and stroke volume • Heart rate is by stimulation of the sympathetic nerves to the heart (NE) and by epinephrine (E); it is by stimulation of the parasympathetic nerves to the heart • Stroke volume is increased mainly by an in enddiastolic volume (the Frank-Starling mechanism) and by an in contractility due to sympathetic-nerve stimulation or to epinephrine. Afterload can also play a significant role in certain situations Swollen legs A 47 year old woman was brought to the hospital because of severe shortness of breath and swelling of her lower body. Over the last year *she had noticed periods of shortness of breath while doing her housework (exertional dyspnea). She also had shortness of breath while lying down (orthopnea). The patient often awoke at night with a sensation of not getting enough air and she had to sit or stand to obtain relief (paroxysmal nocturnal dyspnea). #More recently she noticed swelling first of her lower extremities and then of her lower abdomen. The swelling was worse through the day and decreased overnight. She reported awakening three to four times a night to urinate. The patient did not remember any ill health before these problems began. Physical examination revealed a woman sitting up in bed in mild to moderate respiratory distress. Her blood pressure was 100/70, pulse was 120 and weak. Respirations were 26 per minute and labored. There was jugular venous distension, even while she was sitting. Palpation of the sternum revealed a restrosternal lift. Auscultation of the heart revealed an opening snap and a long diastolic rumble at the apex. Auscultation of the lungs revealed crackles halfway up the lungs. There was also severe lower extremity edema. During her hospitalization, as part the work-up, the following studies were done. O2 consumption(VO2) Arterial-venous O2 content difference Heart rate Mean Pulmonary Capillary Wedge Pressure Right Ventricular Systolic pressure End-Diastolic pressure Right Ventricular End Diastolic volume Patient Normal 188 ml/min 5.3 ml/dl blood 200-250mL/min 3.0-5.0 ml/dl blood 122 25 mm Hg 60-100 beats/min <15 mmHg 80 mm Hg 16 mm Hg <28mmHg <8mmHg 140 ml/m2 60-88mL/m2 •Use the data in the table above to calculate cardiac output and ejection fraction · Evaluate the mean electrical axis of the heart using the ECG shown overleaf